001_Altered mental s..
advertisement
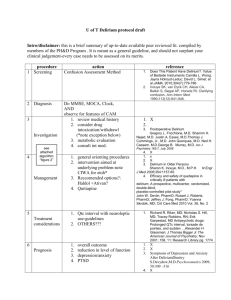
Altered Mental Status: Delirium and Coma DR. MOHAMMAD ALJAWADI PHARMD, MSC, PHD PHCL 478 CLINICAL PHARMACY DEPARTMENT COLLEGE OF PHARMACY KING SAUD UNIVERSITY APRIL 2015 In ICUs: This is what we usually see This is what might happening Introduction • Altered mental status is very common in ICUs • Severe disease processes • Iatrogenic • Altered metal status can be due to brain dysfunction • Acute: Coma and Delirium • Chronic: Subsequent long-term cognitive impairment after discharge In ICU: Acute Brain Dysfunction • Coma is characterized by unresponsiveness to physical or verbal stimuli. • Delirium is an acute and fluctuating disorder of consciousness characterized by inattention, disorganized thinking, and perceptual disturbances with hypoactive and hyperactive subtype Acute Brain Dysfunction Etiology • Despite increasing research in the field, the multifactorial pathophysiological processes of delirium and coma remain poorly understood. • Numerous hypotheses: • Neurotransmitter imbalance (eg, dopamine, γ-aminobutyric acid, and acetylcholine) • Inflammatory perturbations (eg, tumor necrosis factor-α, interleukin-1, and other cytokines and chemokines) • Impaired oxidative metabolism • Cholinergic deficiency • Changes in various amino acid precursors Incidence • The incidence of acute brain dysfunction is common in the ICU • Between 50% and 80% of patients with critical illness developing delirium depending on the severity of illness and the need for mechanical ventilation • Still underdiagnosed Consequences of Acute Brain Dysfunction Longer weaning time from mechanical ventilator Patients without delirium compared to those with delirium (3.6 days vs. 10.7 days) Increased Hospital length of Stay ( an additional 1.18 days compared to non-delirious patients) Increased ICU mortality Increased Readmission after hospital discharge Higher ICU and hospital costs Delirium and Mortality Death among patients without delirium compared to those with delirium (15 of 126 [11.9%] vs. 69 of 228 [30.3%]) Each additional day of delirium increases the risk of dying. Days in ICU Hazard of Death 1 HR: 1.70; (95% CI, 1.27-2.29) 2 HR: 2.69; (95%CI, 1.58-4.57) 3 HR: 3.37; (95%CI, 1.92-7.23) Number of delirious days was associated with increased risk of 1 year post-ICU mortality (hazard ratio, 1.10; 95% confidence interval, 1.02–1.18). Consequences of brain dysfunction after discharge • Among patients who survive their critical illness, up to 75% experience long-term cognitive impairment • Longer periods of acute brain dysfunction in the hospital are associated with greater degrees of cognitive decline 1 year after hospital discharge Diagnosis of Acute Brain Dysfunction • To diagnose delirium in the ICU: • The validation of the Confusion Assessment Method for the ICU (CAM-ICU) • The Intensive Care Delirium Screening Checklist (ICDSC) • Many scales are used to assess the level of sedation and agitation of patients in ICU: • Ramsay scale • Riker Sedation-Agitation Scale • Motor activity assessment scale • Glasgow Coma Scale • Richmond Agitation-Sedation Scale (RASS) We use one of these with CAM-ICU or ICDSC to diagnose delirium FYI FYI FYI Riker Sedation-Agitation Scale FYI Required Diagnosis criteria • To diagnose delirium: 1) RASS score of –3 or higher ( -2 , -1, 1, 2, 3, 4) 2) Feature 1 of CAM-ICU (acute change or fluctuation in mental status) 3) Feature 2 of CAM-ICU (inattention) 4) One of the following: Feature 3 (disorganized thinking) OR Feature 4 (altered level of consciousness of CAM-ICU) Diagnosis criteria • Coma: • RASS score of -4 or -5 Risk factors: Let us focus on them Source: Delirium in the intensive care unit;Timothy D Girard, Pratik P Pandharipande, and E Wesley Ely Psychoactive Medications • The temporal association of psychoactive medications with delirium in critically ill patients has been examined in different ICU cohort • Among mechanically ventilated patients: • Lorazepam be an independent risk factor for the daily development of delirium • Propofol, morphine, and fentanyl were associated with higher but not statistically significant odds ratios for delirium development in the same cohort. • In surgical, trauma, and burn ICU patients, midazolam has been associated with increased delirium incidence. Delirium potential: Benzodiazepines vs. Opioids ? Delirium potential: Benzodiazepines vs. Opioids ? • Opioids: • The effects on acute brain dysfunction are not as consistently demonstrated as the effects of benzodiazepines. • Insufficient pain relief has been shown to be a risk factor for delirium • In a prospective cohort study that enrolled delirium free-patients with hip fractures,: • Doses <10 mg morphine daily was associated with higher delirium incidence than receiving > 10 mg a day. • Thus, opiates may be protective of acute brain dysfunction in patients at high risk for pain but may be detrimental if used excessively to achieve sedation. Depth of sedation: The dilemma between too much or to little Depth of sedation: The dilemma between too much or to little • Under-sedation and inadequate pain relief: • Hyperactive stress response • Tachycardia, increased oxygen consumption, hypercoagulability, immunosuppression, hypermetabolism, and increased endogenous catecholamine activity. • Agitation can lead to the removal of medical devices (e.g., endotracheal tubes, intravascular lines), creating life-threatening situations. • Posttraumatic stress disorder (PTSD) after discharge Depth of sedation: The dilemma between too much or to little • Over-sedation is the norm in ICUs, however, it has its own consequences: • Higher probability of developing delirium • Longer duration of mechanical ventilation and ICU length of stay • Increased use of radiological evaluations of mental status • The presence of burst suppression on electroencephalograms, associated with deep sedation, has been shown to be an independent predictor of mortality in critically ill patients • To reduce deep sedation, multiple strategies have been evaluated to decrease patients’ psychoactive drug exposure. • Target-based sedation • Protocolizing sedative drug delivery • Daily interruptions of sedations decrease sedative administration and improve patient outcomes Mechanically Ventilated Patients Sedation discontinuation based on a prespecified protocol The Awakening and Breathing Controlled Trial: Spontaneous Awakening Trials (SATs) + SBT Spontaneous Breathing Trials (SBTs) Outcomes: Spontaneous breathing ICU discharge Hospital Discharge Self-extubation 12-months mortality The Awakening and Breathing Controlled Trial: • Patients in the intervention group were : • • spontaneously breathing more than the control group (14·7 days vs. 11·6 days; mean diference 3·1 days, 95% CI 0·7 to 5·6; p=0·02) and • discharged from intensive care earlier (median time in intensive care 9·1 days vs 12·9 days; p=0·01) • discharged from the hospital earlier (median time in the hospital 14·9 days vs 19·2 days; p=0·04). More patients in the intervention group self-extubated than in the control group • (16 patients vs six patients; 6·0% difference, 95% CI 0·6% to 11·8%; p=0·03), but the number of patients who required reintubation after self-extubation was similar (five patients vs three patients; 1·2% difference, 95% CI –5·2% to 2·5%; p=0·47) • 12-months mortality: patients in the intervention group were less likely to die than were patients in the control group (HR 0·68, 95% CI 0·50 to 0·92; p=0·01). • For every seven patients treated with the intervention, one life was saved (number needed to treat was 7·4, 95% CI 4·2 to 35·5). What about after discharge: • Interrupted sedation methods have not been associated with an increase in long-term neuropsychological outcomes PTSD. • Sedating agents have been associated with increased PTSD symptoms • Number of days of sedation in the ICU is associated with a greater likelihood of depression and PTSD. • Delusional memories of the ICU stay are more likely to result in PTSD than factual, even if painful, memories. • Patients with recall of their ICU stay have been shown to manifest less cognitive dysfunction than patients who have complete amnesia for their ICU experience. The ultimate objective • To reduce the incidence and duration of acute and long-term brain dysfunction in critically ill patients. • ABCDEs: • Awakening and Breathing trials • Choice of sedation • Delirium monitoring and management • Early Exercise Management of Delirium: • Choice of Sedatives • Non-Pharmacological • Pharmacological •Alpha2-Adrenergic Agonist; •Sedative Choice of Sedatives: Study Comparators Favors Outcome and its result Propofol vs. BDZs Propofol Lower ventilator days Opioids (morphine or remifentanil) vs. BDZs morphine or remifentanil Lower ventilator days Dexmedetomidine vs. lorazepam (MENDS study) dexmedetomidine decrease the duration of brain organ dysfunction, with a lower likelihood of delirium development on subsequent days Dexmedetomidine vs. midazolam (SEDCOM study) Dexmedetomidine Reduction in delirium incidence and shorter time on mechanical ventilation Dexmedetomidine vs. morphine (DEXCOM study) Dexmedetomidine reduced the duration but not the incidence of delirium Dexmedetomidine: Selective alpha2-adrenoceptor agonist Dexmedetomidine: Non-pharmacological: • Orientation • Clinical parameters: • Provide visual and hearing aids. • maintain systolic blood pressure >90 mm hg. • Encourage communication and reorient patient repetitively. • Maintain oxygen saturations >90%. • Treat underlying metabolic derangements and infections • Have familiar objects from patient’s home in the room. • Attempt consistency in nursing staff. • Allow television during day with daily news. • Allow nonverbal music. • Environment • • Maintain sleep hygiene: • Keep lights off at night, on during the day. • Consider sleep aids (zolpidem, mirtazapine). • Control excess noise (staff, equipment, visitors) at night. Ambulate or mobilize patient early and often. Risk factors: Pharmacological Therapy: • Only after minimizing contributing factors and optimizing treatment of the underlying physiological abnormalities • Antipsychotics: • Lack of large RCT comparing typical or atypical antipsychotics to placebo • Small studies and case reports consist the constitute the best data available • While tapering or discontinuing sedatives, consider: • Typical: • Haloperidol 2 to 5 mg IV initially (0.5-2 mg in elderly) and then q 6 hours. • Guideline for max haloperidol dose is 20 mg/day. • Atypical: • Olanzapine, quetiapine, risperidone, ziprasidone, or abilifide • Discontinue if high fever, QTc prolongation, or drug-induced rigidity. Comparative Effectiveness: Study Comparators Favors Outcomes Olanzapine vs. Haloperidol No difference Severity of delirium symptoms Quetiapine vs. Placebo Quetiapine Resolution of delirium Risperidone vs. Placebo Risperidone Reduced the incidence of delirium ziprasidone vs. Haloperidol vs. placebo (MIND Study) No difference number of days patients were alive without delirium or coma. Rivastigmine vs. Haloperidol No difference Duration of delirium, rivastigmine may increase ICU mortality Points regarding Haloperidol: • Onset of action 15 to 20 minutes after intravenous infusion. • Duration of effect: re-dosing may be needed 4 to 12 hours after symptoms have been controlled with the initial doses. • Highly protein bound, has a large volume of distribution, is metabolized hepatically by CYP3A4, CYP2D6, and glucuronidation (many many many drug interactions) • Adverse effect: • Rare but serious : polymorphic ventricular tachycardia (including torsades de pointes) • The QT interval should be monitored every shift (ie, every 8 to 12 hours) and haloperidol should not be given if the corrected QT interval exceeds 500 msec (normal in males: 460 msec; females: 480 msec) • Extrapyramidal side effects are less common with IV intravenous haloperidol than among those receiving oral haloperidol • Death in elderly??? (may not be applicable in the ICU) Antipsychotics: • They have psychoactive effects that may further cloud the sensorium and promote a longer overall duration of cognitive impairment. • The lowest effective dose for the shortest possible time may be the most important delirium management recommendation Not in the ICUs Required Questions