Sherwood 7
advertisement

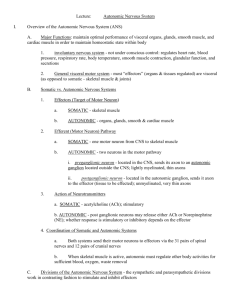
Chapter 7 The Peripheral Nervous System: Efferent Division Outline • Autonomic nervous system • Somatic nervous System • Neuromuscular Junction Outline • Autonomic nervous system – Anatomy • Pre and post fibers, sympathetic ganglia chain, collateral ganglia, terminal ganglia – Neurotransmitters • Pre = Acetylcholine (ach) • Post = adrenaline (epinepherine) noradrenaline (norepinepherine) – Sympathetic and parasympathetic branches • Dual innervation • Sympathetic dominance “fight or flight” • Parasympathetic dominance “rest and digest” – Receptor types • Cholinergic, muscarinic, nicotinic • Adrenergic. a1 a2 b1 b2 – CNS control PNS: Efferent Division • Communication link by which CNS controls activities of muscles and glands • Two divisions of PNS – Autonomic nervous system (ANS) • Involuntary branch of PNS • Innervates cardiac muscle, smooth muscle, most exocrine glands, some endocrine glands, and adipose tissue – Somatic nervous system • Subject to voluntary control • Innervates skeletal muscle Table 7-1, p. 234 ANS • Autonomic nerve pathway – Extends from CNS to an innervated organ • Ganglion = neuronal cell bodies in the PNS • Nuclei = neuronal cell bodies in the PNS CNS – Two-neuron chain • Preganglionic fiber (synapses with cell body of second neuron) • Postganglionic fiber (innervates effector organ) ANS Sympathetic Nervous System • Two subdivisions – Sympathetic nervous Fibers originate in system thoracic and lumbar – Parasympathetic Nervous System Fibers originate from cranial and sacral areas • Thoracic and lumbar regions of spinal cord of CNS Most preganglionic Preganglionic fibers are Parasympathetic fibers are short longer nervous system • Cervical and sacral Long postganglionic fibers Very short postganglionic fibers Preganglionic fibers release acetylcholine (Ach) Preganglionic fibers release acetylcholine (Ach) Most postganglionic fibers release noradrenaline (norepinephrine) Postganglionic fibers release acetylcholine Brain ACh ACh Effector organs Terminal ganglion Spinal cord ACh Cardiac muscle Craniosacral parasympathetic nerves = Parasympathetic system = Preganglionic fiber = Postganglionic fiber NE Sympathetic ganglion chain = Sympathetic system Smooth muscle = Acetylcholine = Norepinephrine = Epinephrine Thoracolumbar sympathetic nerves Adrenal medulla = Cell body = Cell body = Axon Blood E,NE NE ACh Collateral ganglion ACh Terminal ganglion Most exocrine glands and some endocrine ACh glands Fig. 7-2, p. 235 ANS • Most visceral organs innervated by both sympathetic and parasympathetic fibers • In general produce opposite effects in a particular organ • Dual innervation of organs by both branches of ANS allows precise control over organ’s activity ANS • Sympathetic system dominates in emergency or stressful (“fight-or-flight”) situations – Promotes responses that prepare body for strenuous physical activity • Parasympathetic system dominates in quiet, relaxed (“rest-and-digest”) situations – Promotes body-maintenance activities such as digestion Eye Lacrimal gland Nasal mucosa Parotid gland Sympathetic Salivary glands Spinal nerves Sympathetic trunk Liver Splanchino nerves Adrenal gland Parasympathetic Trachea Lung Cranial nerves Heart Stomach Gall bladder Pancreas Spleen Sympathetic preganglionic fiber Sympathetic postganglionic fiber Spinal nerves Kidney Small intestine Colon Parasympathetic preganglionic fiber Parasympathetic postganglionic fiber Rectum Urinary bladder Genitalia Fig. 7-3, p. 237 Effects of Autonomic Nervous System on Various Organs ANS • Exceptions to general rule of dual reciprocal innervation by the two branches of autonomic nervous system – Most arterioles and veins receive only sympathetic nerve fibers (arteries and capillaries are not innervated) – Most sweat glands are innervated only by sympathetic nerves – Salivary glands are innervated by both ANS divisions but activity is not antagonistic – both stimulate salivary secretion ANS • Adrenal medulla is a modified part of sympathetic nervous system – Modified sympathetic ganglion that does not give rise to postganglionic fibers – Stimulation of preganglionic fiber prompts secretion of hormones into blood • About 20% of hormone release is norepinephrine • About 80% of hormone released is epinephrine (adrenaline) • Broadcast vs. localized Autonomic Neurotransmitters Brain ACh ACh Effector organs Terminal ganglion Spinal cord ACh Cardiac muscle Craniosacral parasympathetic nerves = Parasympathetic system = Preganglionic fiber = Postganglionic fiber NE Sympathetic ganglion chain = Sympathetic system Smooth muscle = Acetylcholine = Norepinephrine = Epinephrine Thoracolumbar sympathetic nerves Adrenal medulla = Cell body = Cell body = Axon Blood E,NE NE ACh Collateral ganglion ACh Terminal ganglion Most exocrine glands and some endocrine ACh glands Fig. 7-2, p. 235 Autonomic Neurotransmitter Receptors • Tissues innervated by autonomic nervous system have one or more of several different receptor types for postganglionic chemical messengers – Alter tissue/cell response instead of chemical message – Alter the distribution (localized – varicosity, broadcast – adrenal medulla) – Cholinergic receptors – bind to ACh • Nicotinic receptors – found on postganglionic cell bodies of all autonomic ganglia – nicotine • Muscarinic receptors – found on effector cell membranes – Mushroom poison – Andrenergic receptors – bind to norepinephrine and epinephrine • Alpha (α) receptors • Beta (β) receptors Autonomic Neurotransmitter Receptors – Cholinergic receptors – bind to ACh • Nicotinic receptors – found on postganglionic cell bodies of all autonomic ganglia – Nicotine – Respond to Ach, opens Na and K channels, triggers AP • Muscarinic receptors – found on effector cell membranes – – – – Mushroom poison Smooth muscle, cardiac muscle, glands 5 subtypes G protein linked Autonomic Neurotransmitter Receptors – Andrenergic receptors – bind to norepinephrine and epinephrine • G protein coupled • Alpha (α) receptors - Ca second messenger system a 1= stim cyclic amp, sympathetic tissues, vessel constriction, contraction of smooth muscle, constrictor a 2 blocks cyclic amp, decreased smooth muscle contraction in the digestive tract, inhibitory to the effector organ • Beta (β) receptors - cyclic amp b1 Found in the heart, increases contractility and rate b2 Found in the arterioles and airways, dilator Spinal cord = Acetylcholine = Norepinephrine Sympathetic preganglionic fiber = Epinephrine Adrenal medulla Sympathetic postganglionic fiber norepi Blood both epi Fig. 7-4, p. 239 Autonomic Agonists and Antagonists • Agonists – Bind to same receptor as neurotransmitter – Elicit an effect that mimics that of neurotransmitter • Antagonists – Bind with receptor – Block neurotransmitter’s response Regions of CNS Involved in Control of Autonomic Activities • Can be influenced by prefrontal association complex through its involvement with emotional expression characteristic of individual’s personality • Hypothalamus plays important role in integrating autonomic, somatic, and endocrine responses that automatically accompany various emotional and behavioral states • Medulla within brain stem is region directly responsible for autonomic output • Some autonomic reflexes, such as urination, defecation, and erection, are integrated at spinal cord level Distinguishing Characteristics of Sympathetic and Parasympathetic Nervous Systems Outline • Somatic nervous system – Anatomy • • • • • Motor neurons Continuous to effector Voluntary Final common pathway ALS = Amyotropic lateral sclerosis, death of motor neurons Somatic Nervous System • Consists of axons of motor neurons of motor neurons that originate in spinal cord or brain stem and end on skeletal muscle • Motor neuron releases neurotransmitter, Ach, which stimulates muscle contraction • Motor neurons are final common pathway by which various regions of CNS exert control over skeletal muscle activity – These areas of CNS include spinal cord, motor regions of cortex, basal nuclei, cerebellum, and brain stem Comparison of Somatic and Autonomic Nervous System Spinal cord = Acetylcholine = Norepinephrine Sympathetic preganglionic fiber = Epinephrine Adrenal medulla Sympathetic postganglionic fiber Blood Target organs Fig. 7-4, p. 239 Outline • Neuromuscular junction – Anatomy • Muscle fiber, terminal button • “motor end plate” – Ach release • Presynaptic vesicular • Postsynaptic intracellular – Ach activation of end plate potentials • Activation of nicotinic receptors • Inflow of sodium and potassium • Ap propagated along the muscle fiber – Ach breakdown • AChe Neuromuscular Junction • Axon terminal of motor neuron forms neuromuscular junction with a single muscle cell • Signals are passed between nerve terminal and muscle fiber by means of neurotransmitter ACh • Released ACh binds to receptor sites on motor end plate of muscle cell membrane • Binding triggers opening of specific channels in motor end plate • Ion movements depolarize motor end plate, producing endplate potential • Local current flow between depolarized end plate and adjacent muscle cell membrane brings adjacent areas to threshold • Action potential is initiated and propagated throughout muscle fiber Neuromuscular Junction • Acetylcholinesterase – Inactivates ACh – Ends end-plate potential and the action potential and resultant contraction • Neuromuscular junction is vulnerable to chemical agents and diseases – Black widow spider venom causes explosive release of ACh – Botulism toxin blocks release of ACh – Curare blocks action of ACh at receptor sites – Organophosphates prevent inactivation of ACh – Myasthenia gravis inactivates ACh receptor sites Axon of motor neuron Action potential propagation in motor neuron Myelin sheath Axon terminal Terminal button Voltage-gated calcium channel Vesicle of acetylcholine Acetylcholine receptor site Action potential propagation in muscle fiber Acetycholinesterase Plasma membrane of muscle fiber Voltage-gated Na+ channel Chemically gated cation channel Motor end plate Contractile elements within muscle fiber Fig. 7-6, p. 245 Neuromuscular conditions and compounds • ALS – Lou Gehrig’s Disease • death of motor neurons – Black widow venom • Explosive release of Ach • Paralysis of the diaphram – Botulinum toxin • Inhibits Ach release – Curare • Ach receptor blocker (chloinergic) – Organophosphates • Ache inhibition – Mysanthia Gravis • Autoimmune, body attacks Ach receptors – Rigor mortis