RNZCGP Medical Record Review Tool
advertisement
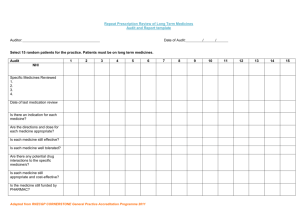
RNZCGP Medical Record Review tool Introduction: General practices deliver a service that must be managed effectively to ensure that it meets the needs of patients. The patient’s medical record is integral to maintaining good patient care and continuity of care. Patient records should describe and support the health care that has been provided. They should be understandable to a newcomer to the practice. The structure of the records should allow information to be obtained easily. It is important that adequate information is recorded for each consultation and that the person making the entry is identified – this includes telephone consultations. Conducting a record review helps to establish and improve the quality of medical records and supports the safe care of patients. This medical record review tool can be used by practices who are conducting self-assessments in preparation for practice accreditation processes. The tool enables doctors, practice nurses and practices to ensure that they are meeting Indicator 21 of the RNZCGP Foundation Standard and Indicator 22 of the Aiming for Excellence Standard for New Zealand General Practice: Patient records meet requirements to describe and support the management of health care provided. The criteria in this tool also link to a number of other criteria in the Standards. This medical record review tool is also a component of the general practice education programme and can be used as an audit activity for the continuing professional development programme (MOPS). The tool has three parts: Module 1 includes requirements for the practice patient record system and the demographic details that it records. This module should be undertaken for practice accreditation purposes. If this module has been done in the practice within the past three years, this module does not need to be completed by doctors undertaking Module 2 for training programme1 or professional development education purposes. The module contains both foundational and advanced criteria. Module 2 contains criteria which should be assessed for practice accreditation, training programme and professional development purposes. The module contains both foundational and advanced criteria. The bullets alongside criteria in the tool indicate the following: These are foundational criteria which must be examined in the Foundation Standard process. These criteria indicate that the medical record meets minimum legal, regulatory and professional standards and is sufficient for safe practice. These criteria are found in both modules 1 and 2. (These criteria are also indicated in red in the document.) These are advanced criteria which must be examined as part of the CORNERSTONE assessment process. These criteria indicate that the medical record is complete. These criteria are found in both modules 1 and 2. (These criteria are also indicated in blue in the document.) Note that both foundational and advanced criteria (red and blue) are completed for the training and continuing professional development programmes. 1 If your practice has completed Module 1, please provide a copy with your completed Module 2. RNZCGP Medical Record Review Tool Instructions: Modules 1 and 2 of the tool require a random audit of ten patient records. Applications which generate lists of random numbers are available online. However, the easiest way to generate a random sample is to select consecutive patient appointments, beginning at a random time, on a randomly selected day. Patient records should be electronic. All records selected should have an entry in the past 12 months. Modules 1 and 2 Randomly select ten patient medical records. Complete the Module 1 or 2 template attached by noting the NHI number for the record, and then mark the unshaded boxes for each of the records reviewed as follows: √ present and adequate IN present but inadequate X not present N/A not applicable/necessary in this case Complete the ‘Report and Plan’ template, identifying areas from development and a plan for improvement. Improvement plans should specifically address every gap in foundational standards (marked by a solid bullet, and in red), and should ideally also address any gaps identified in meeting the advanced standards (marked by a hollow bullet, and in blue). GPEP Registrars: It is your responsibility to check whether the practice has completed Module 1 of the tool in the past three years, and if not, to compete it as part of your audit requirements. If your practice has completed Module 1, please provide a copy with your completed Module 2. You are required to submit the completed medical record audit tool to the College. Complete and return both the Recording Sheet and the Report and Plan sheet to your GPEP Programme Administrator. You are encouraged to discuss the results of this audit activity with your medical educator, collegial relationship provider, or a peer. Document Owner: Education Standards Principal Advisor July 2015 Page 2 of 7 Objective ID A350088 RNZCGP Medical Record Review Tool Doctors name: MCNZ number: Date: Medical Record Review Tool Module 1: Patient record systems2 Met Part met Not met N/a NHI number: 1. Patient records are electronic, secure and traceable: recorded electronically All clinical information is: password protected reliably backed-up dated Clinical notes are: reliably identify the author 2. Basic demographic information is sufficient to allow for patient identification and to meet national enrolment requirements: NHI number Information Gender stored for each patient includes: Address Date of birth Ethnicity Registration status o Information held Contact phone number Contact in case of emergency (ICE) for enrolled Next of kin – where applicable patients Significant relationships includes: Hapu / Iwi for Māori patients Primary language – where applicable o Any need for an interpreter is flagged for patients with English as a second language. 2 This module is completed at practice level as part of the Foundation Standard. Provided it has been done at practice level in the past three years, it does not need to be completed by doctors undertaking modules 2 and / or 3 for other purposes. If not doing this section themselves, GPEP 2 / 3 registrars must attached a copy of the completed Module 1 done by their practice. Document Owner: Education Standards Principal Advisor July 2015 Page 3 of 7 Objective ID A350088 RNZCGP Medical Record Review Tool Medical Record Review Tool Module 2: Medical record review (foundational and advanced criteria) Doctors name: MCNZ number: Date: Met Part met Not met N/a NHI number: The record is objective, contemporary and sources are identified: Notes are made as soon as possible after contact and any delay is identifiable. When information is provided by other than the patient, the source is identified. Clinical notes can be understood by someone not working regularly at the practice: The notes are ordered, intelligible, and sequential. The use of keywords or templates does not compromise the validity of the notes. Important medical warnings (or the absence of any) are displayed for all records: Medical warnings, past medical history, and / or previous medication adverse reactions are recorded, where relevant. All important medical alerts available on the practice management system are activated. Allergy status (allergies or the absence of known allergies) is recorded for each patient. Prescriptions cannot be generated unless allergies are recorded. Specific patient needs and instructions are recorded and are available in easily accessible form at the clinically relevant point: Patient needs and instructions recorded include, where applicable, directives by patient, disabilities of patient, drug dependencies, end of life needs, and special alerts (e. g. deaf, blind, communication requirements, mental health issues). The recorded history is adequate for both safe management and evidential purposes: The reason for the encounter is recorded or apparent from the notes. The record of the examination includes all findings essential to diagnosis and management: Sufficient positive and negative findings are present to justify management decisions. Objective measurements (BP, pulse, temp., respiratory rate, pA02 etc.) are recorded, where relevant. Photographic evidence is included, where relevant (e.g. skin lesions). The working diagnosis/differential is apparent and consistent with supporting information: The diagnosis (and any differential) and level of certainty is clear from the notes. The record identifies information given to the patient, including risks and benefits of treatments and, where relevant, consent: Patient notification of test results and other clinical findings is recorded. There is a record of advice given to support any necessary consent and its confirmation. The record includes evidence of signed or verbal consent to procedures as required. Informed consent is documented when there is variance between evidence and practice. Notes include health information, preventative care information and referrals to wellness services given to patients. Clinical management decisions and any interventions provided are recorded: The management / treatment plan is clear from the notes, including contingency plans and follow-up arrangements (safety netting) where necessary. The notes include any clinical management decisions made outside consultations (e.g. telephone calls) and off-site consultations (home visit, aged care facilities etc.). Any brief interventions provided are recorded. Document Owner: Education Standards Principal Advisor July 2015 Page 4 of 7 Objective ID A350088 RNZCGP Medical Record Review Tool The record identifies all medication treatment provided including the type, dosage and total amount of any medications prescribed: There is a record of all prescriptions issued including drug name / dosage / frequency / time / volume and total amount. Any medications prescribed outside the practice have been recorded and reconciled in the PMS. Current and long-term medications are differentiated and the status is clear. Where long-term medications are changed, reasons for alteration or discontinuation are recorded. All long-term prescribed medications are linked with a medical condition. The record identifies all investigations requested and tracks high-risk tests: All tests and investigations requested are recorded. High-risk tests (e.g. histology, cervical smears) are tracked for completion. The record supports effective and timely referral for treatment and transfer / continuity of care: Copies of referral letters to and from the practice, certifications, referrals and responses, discharge summaries and test results are included in the patient PMS record or accessibly filed. Referrals include urgency, reason/expectation of referral, relevant findings, classifications, warnings and current treatment. The record confirms that all referrals are enacted in a timely way. The record confirms appropriate and timely action in response to incoming correspondence. Follow-up arrangements are clearly documented and actions are recorded: Follow-up actions on test results and referrals are recorded. When transferring patients to providers and services outside the practice in potentially significant cases, there is evidence of tracking of referral status and safe transfer of clinical responsibility. Screening history and results (or patient decline) are recorded: Screening history and results (or patient decline) is recorded for routine screening areas (this may vary with current national guidelines but examples include cervical smears, mammograms, cardiovascular risk assessment, diabetes screening). Screening recall status can be easily tracked. There is evidence of patient risk assessment and opportunistic screening for high risk conditions. Immunisation history and status is recorded: There is evidence that recommended immunisations are conducted and updated according to the national schedule. Records show advice given and immunisation status for nonscheduled immunisations. There is a systematic record of individual risk factors: Diseases are classified for common chronic diseases including all conditions for which the patient is on long-term treatment. Family history (or lack of history of note) for major risk factors, such as diabetes, early CVD, bowel and breast cancer etc. Current employment (where relevant) and any history of at-risk occupations. Blood pressure monitoring as clinically indicated. Baseline weight / BMI and monitoring as clinically indicated. Smoking status and history and cessation support offered, where relevant. Alcohol and drug usage. Regular diabetic review. Document Owner: Education Standards Principal Advisor July 2015 Page 5 of 7 Objective ID A350088 Doctors name: MCNZ number: Date: RNZCGP Medical Record Review Tool Report and Plan template After having completed modules 1 and/or 2 of the tool, summarise your findings and plan any necessary improvements on the template below. The template lists each of the indicators in modules 1 and 2. In column 1 under each indicator, record the proportion of records that did not meet the criteria. In column 2, give the areas that need improvement, and in column 3, briefly describe your plan for improvement. Audit finding: Area(s) of omission: Plan for improvement: Patient records are electronic, secure and traceable: Basic demographic information is sufficient to allow for patient identification and to meet national enrolment requirements: The record is objective, contemporary and sources are identified: Clinical notes can be understood by someone not working regularly at the practice: Important medical warnings (or the absence of any) are displayed for all records: Specific patient needs and instructions are recorded and are available in easily accessible form at the clinically relevant point: The recorded history is adequate for both safe management and evidential purposes: The record of the examination includes all findings essential to diagnosis and management: Document Owner: Education Standards Principal Advisor July 2015 Page 6 of 7 Objective ID A350088 RNZCGP Medical Record Review Tool The working diagnosis/differential is apparent and consistent with supporting information: The record identifies information given to the patient, including risks and benefits of treatments and, where relevant, consent: Clinical management decisions and any interventions provided are recorded: The record identifies all medication treatment provided including the type, dosage and total amount of any medications prescribed: The record identifies all investigations requested and tracks high-risk tests: The record supports effective and timely referral for treatment and transfer / continuity of care: Follow-up arrangements are clearly documented and actions are recorded: Screening history and results (or patient decline) are recorded: Immunisation history and status is recorded: There a systematic record of individual risk factors: Document Owner: Education Standards Principal Advisor July 2015 Page 7 of 7 Objective ID A350088