Overview - WordPress.com
advertisement

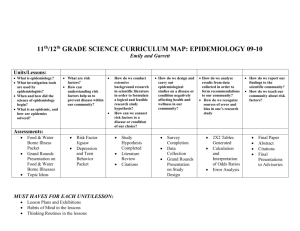
Disease Detectives Disease Detectives focuses on epidemiology, that is, the study of diseases and how they spread. The 2012-2013 focus topic is environmental quality. Event Format You are allowed to bring 2 non-graphing calculators and 1 page of Notes. Competitors in Division B should be able to do the following for competition: List and recognize examples of different modes of transmission Calculate health-related rates (attack, incidence, prevalence, case fatality) Calculate a simple relative risk and describe what it means Interpret epi curves, temporal patters and other simple graphic presentations of health data List, discuss, and recognize examples of disease-causing agents (physical and biological) Demonstrate an understanding and ability to use terms such as endemic, epidemic, pandemic, and concepts such as population versus sample and association versus cause Describe various types of prevention and control strategies, such as immunization, behavior change, etc., and situations where they might be used For the national level, B division competitors should also be able to do the following: Understand how units affect the relative magnitude of a set of rates with different units Calculate appropriate measures of risk when given the study design Complete tables when given all data needed to complete calculations Propose a reasonable intervention to a public health problem Recognize gaps in information In addition to these concepts, competitors in Division C should be able to: Identify types of Epidemiology o Classical Epidemiology- Looking at sociological, enviornmental, and behavioral aspects. o Analytical Epidemiology- Using quantitative data and equations to look at epidemiological scenarios. Recognize differences between study designs Calculate measures of risk, such as relative risk or odds ratio, when given a description of the study design Calculate measures based on data that is not given but that can be readily extracted Recognize how gaps in information influence the ability to extend conclusions to the general population At the national level, C division competitors should also be able to do the following: Recognize unmentioned factors that may influence results Convert between rates with different basic units (e.g. incidence per 10,000 persons/year to incidence per 100 persons/week) Propose a means to evaluate the effectiveness of an intervention or control program The Basics Epidemiology Epidemiology is the study of distribution and determinants of health-related states in specified populations, and the application of this to control health problems. There are four basic reasons for why disease detectives study and research outbreaks and epidemics. These reasons are: Control and Prevention, Research Opportunities, Training, and Legal Concerns. Two Basic Types of Epidemiology 1. Classical Epidemiology - population oriented, studies community origins of health problems related to nutrition, environment, human behavior, and the psychological, social, and spiritual state of a population. The event is more aimed towards this type of epidemiology. 2. Clinical Epidemiology - studies patients in health care settings in order to improve the diagnosis and treatment of various diseases and the prognosis for patients already affected by a disease. These can be further divided into: o Infectious Disease Epidemiology - heavily dependent on laboratory support o Chronic Disease Epidemiology - dependent on complex sampling and statistical methods Basic Epidemiology Terms Cluster - An aggregation of cases over a particular period closely grouped in time and space, regardless of whether the number is more than the expected number Outbreak - More cases of a particular disease than expected in a given area or among a specialized group of people over a particular period of time. Epidemic - Large numbers of people over a wide geographical area are affected Pandemic - An epidemic occurring over several countries or continents and affecting a large proportion of the population. Surveillance - The systematic and ongoing collection, analysis, interpretation, and dissemination of health data. The purpose of public health surveillance is to gain knowledge of the patterns of disease, injury, and other health problems in a community so that we can work towards their prevention and control. Plague - A serious, potentially life-threatening infectious disease that is usually transmitted to humans by the bites of rodent fleas. It was one of the scourges of our early history. There are three major forms of the disease: bubonic, septicemic, and pneumonic. Vector - An animal that transmits disease. For example a mosquito is a vector for malaria. Fomite - A physical object that serves to transmit an infectious agent from person to person. Risk - The probability that an individual will be affected by, or die from, an illness or injury within a stated time or age span. Zoonosis - An infectious disease that is transmissible from animals to humans. Incubation Period - Time in between when a person somes into contact with a pathogen and when they first show symptoms or signs of disease. Endemic Disease - Present at a continuous level throughout a population/geographic area; constant presence of an agent/health condition within a given geographic area/population; refers to the usual prevalence of an agent/condition. 2013 Topic- Environmental Quality Environmental Causes of Health Problems o Smoking, air pollution o Flooding and drought o o o o o o o o o o o o o o o o o o o o o o o o o o o o Extreme heat, UV exposure Pesticides, chemical spills, lead contamination Water pollutants, heavy metals Ventilation pollutants Noise induced hearing loss Waste and toxic substance Food contamination Other pathogenic agents as prions Foods most associated with food borne illness Raw meat and poultry Raw eggs Unpasteurized milk Raw shellfish Raw fruits and vegetables Unpasteurized fruit juice Food processing concerns Foods that mingle the products of several individual animals A pathogen in one animal can contaminate may contaminate a whole batch of food mingling the products of several animals as bulk raw milk, pooled raw eggs or ground beef A single hamburger may contain meat from hundreds of animals A glass of raw milk may contain milk from hundreds of cows. A broiler chicken carcass can be exposed to the drippings and juices of many thousands of other birds that went through the same cold water tank after slaughter. Washing fruits and vegetables can decrease but not eliminate contamination Processing food under less than sanitary conditions can cause outbreaks Raw sprouts that are eaten without cooking may contain growing microbes Storage and transport methods for food Reducing the risk of food borne illness Cook meat, poultry, and eggs thoroughly Separate – don’t cross-contaminate one food with another Chill – refrigerate leftovers promptly Clean – wash produce Report – suspected food borne illnesses to the local health department How to prove x caused y, or Causation Hill's Criteria for Causation Nine criteria must be met to establish a cause-and-effect relationship. This is commonly known as Hill's Criteria for Causation: 1. Strength of Association - relationship is clear and risk estimate is high 2. Consistency - observation of association must be repeatable in different populations at different times 3. Specificity - a single cause produces a specific effect 4. Alternative Explanations - consideration of multiple hypotheses before making conclusions about whether an association is causal or not 5. Temporality - cause/exposure must precede the effect/outcome 6. Dose-Response Relationship - an increasing amount of exposure increases the risk 7. Biological Plausibility - the association agrees with currently accepted understanding of biological and pathological processes 8. Experimental Evidence - the condition can be altered, either prevented or accelerated, by an appropriate experimental process 9. Coherence - the association should be compatible with existing theory and knowledge, including knowledge of past cases and epidemiological studies Hill's Criteria for Causation Explanations and History Epidemiological Triad The Epidemiological Triad is the traditional model of infectious disease causation. It is commonly known as the agent/host/environment triad. It includes three components: 1. an external agent 2. a susceptible host 3. an environment that brings the host and agent together, so that disease occurs Chain of Transmission Triad This is another common triad, which is an altered form of the Chain of Infection described below. It is a companion to the Epidemiological Triad. It also has three components: 1. an external agent 2. a vector or fomite that transmits the disease 3. a susceptible host for the disease This is used to define the major points of a disease case. Epidemiological Study Designs Basic Studies 1. Ecological- comparisons of geographical locations 2. Cross Sectional - a survey, "snapshot in time" 3. Case-control - compare people with and without disease to find common exposures 4. Cohort - compare people with and without exposures to see what happens to each 5. Randomized controlled trial - human experiment Advantages and Disadvantages to Study Designs Study Designs Advantages Disadvantages Time Consuming Most Scientifically Sound Trial Best Measure of Exposure Most Accurate Observational Study Cohort Study Good Measure of Exposure Case-Control Study Cross-Sectional Study Unethical for Harmful Exposures Most Expensive Time Consuming Expensive Can Study Rare Diseases Possible Time-Order Confusion Relatively Less Expensive and Relatively Fast Possible Error in Recalling Past Exposures Fastest Possible Time-Order Confusion Least Expensive Least Confidence in Findings 2*2 Table Table which has two columns and rows for people with or without exposure and with or without disease; shows amount of people with each characteristic. Disease No Disease Exposure a b No Exposure c d Using the 2*2 Table, we can calculate odds ratio and relative risk. These calculations allow comparisons between the control group and the group afflicted with the condition. One is the neutral value and means that there is no difference between the groups compared; when the value is greater than one it means that there has been some difference between the two groups, whether it was caused by bias, chance, or an actual relationship between the exposure and outcome is yet to be seen. The P-value tells us whether the results of the study can be used. The P-value is the measure of how confident you are that your findings are correct. You can only trust your findings to be correct if the P-value is less than .05. Odds Ratio - used in case-control study, ad/bc Relative Risk - used in cohort study, (a/(a+b))/(c/(c+d)) Attack Rate - the rate that a group experienced an outcome or illness equal to the number sick divided by the total in that group. (There should be a high attack rate in those exposed and a low attack rate in those unexposed.) For the exposed: a/(a+b) For the unexposed: c/(c+d) Using Epi-Curves An epi-curve is a histogram that shows the course of an outbreak by plotting the number of cases of a condition according to the time of onset. Epi-Curves fall into three classifications: Point source epidemics occur when people are exposed to the same exposure over a limited, well define period of time. The shape of the curve commonly rises rapidly and contains a definite peak, followed by a gradual decline. Continuous common source epidemics occur when the exposure to the source is prolonged over an extended period of time and may occur over more than one incubation period. The down slope of the curve may be very sharp if the common source is removed or gradual if the outbreak is allowed to exhaust itself. Propagated (progressive source) epidemics occur when a case of disease serves later as a source of infection for subsequent cases and those subsequent cases, in turn, serve as sources for later cases. The shape of this curve usually contains a series of successively larger peaks, reflective of the increasing number of cases caused by person-to-person contact, until the pool of those susceptible is exhausted or control measures are implemented. Disease and Disease Transmission Chain of Infection Agent leaves reservoir through portal of exit, and is conveyed by some mode of transmission, and enters the appropriate portal of entry to infect a susceptible host. Agent - A microbial organism with the ability to cause disease. Reservoir - A place where agents can thrive and reproduce. Portal of Exit - A place of exit providing a way for an agent to leave the reservoir; the route a pathogen takes out of an infected host. Portals of exit tend to be fairly well defined. What serve as portals of exit are often not terribly surprising, at least, once something is known of how and where a pathogen replicates and enters new hosts. Respiratory infections tend to utilize the mouth and nose as portals of exit. Gastrointestinal diseases tend to exit in feces or saliva, depending on the site of replication. Sexually transmitted diseases tend to have portals of exit at the urethra or genital region. Blood-bourne diseases tend to exit via arthropods, needles, bleeding, or hyperdermic syringes. A more general portal of exit occurs when an infected animal is butchered or an infected person undergoes surgery. The three most common portals of exit are the skin, gastrointestinal tract, and respiratory tract. Mode of Transmission - Method of transfer by which the organism moves or is carried from one place to another; the transfer of disease-causing microrganisms from one environment to another, particularly from an external environment to a susceptible individual. There are three general categories of transmission: contact, vehicle, and vector. Portal of Entry - An opening allowing the microorganism to enter the host; the route a pathogen takes to enter a host. Just as with the portals of exit, many pathogents have preferred portals of entry. Many pathogens are not able to cause disease if their usual portal of entry is artificially bypassed. The most common portal of entry is the mucous membrane of the respiratory tract. Susceptible Host - A person who cannot resist a microorganism invading the body, multiplying, and resulting in infection. Chain of Infection: Diagram and Explanation Characteristics of Agents 1. Infectivity - capacity to cause infection in a susceptible host 2. Pathogenicity - capacity to cause disease in a host 3. Virulence - severity of disease that the agent causes to host Modes of Disease Transmission o o o o Contact Transmission - sub-categories include direct (person-toperson), indirect (fomite), or droplet. Direct Contact - occurs through touching, kissing, and/or sexual intercourse. To prevent direct contact transmission, wear gloves and masks, use condoms, etc. Indirect Contact - occurs from a reservoir via inanimate objects called fomites. Fomites are basically almost anything an infected individual or reservoir can touch, upon which can be left a resdiue of contagious pathogent. Exceptions include the various inanimates ferred to as vehicles: food, air, and liquids. Typically, it is more difficult to avoid indirect contact transmission than it is to avoid direct contact transmission. A certain degree of organismal durability may be necessary to survive passage on a fomite. The best way to prevent indirect contact transmission is by avoiding contact with fomites, avoiding contact of hands with mucous membranes, especially when handling or potentially handling fomites, the use of barriers when handling fomites, and disinfecting fomites before handling. Droplet Transmission - consequence of being coughed, sneezed, or spit on. To be considered droplet transmission, mucous droplets must still be traveling with the velocity imparted on it leaving the mouth. As a rule of thumb, this is up to one meter after exiting the mouth. Any further and this is considered airborne transmission. Given interaction within one meter of people is certainly more difficult to avoid droplet transmission than it is to avoid either direct or indirect transmission. Not surprisingly, it is especialy respiratory diseases that are transmitted by droplets. Vehicle Transmission - transmission via a medium such as food, air, and liquid, which are al routinely taken into the body, and thus serve as vehicles into the body. Airborne Transmission - occurs via droplets (typically mucous droplets) where droplets are liquids that remain airborne whether as aerosols (very small droplets) or associated with dust particles. An example is within airliners where economizing measures reduces the turnover of cabin air and consequently increases air recycling. Organisms which can find their way into the air and remain viable thus have repeated opportunities to infect passengers. It requires greater organismal durability that droplet transmission simply because of the length of time the microorganism is exposed to the air, before infecting a new host, is longer. Increased durability is to the effects of desiccation, exposure to sunlight, etc. This is why breathing does not typically result in the acquisition of disease. o Food-bourne Transmission - any number of pathogens are found in food and not killed during processing may be transmitted via food product. Salmonella especially tends to be part of the normal flora of chickens and consequently associated with chicken products. o Water-bourne Transmission - fecal contaminated water. Generally, this is via sewage contaminated water supplies. It is especially gastrointestinal pathogens that are present in feces and therefore which rely on this type of transmission. Vector Transmission - no entry. o Portals of Entry to the Nervous System - the brain is typically fairly resistant to bacterial infection. There are four common portals of entry to the nervous system. For an organism to take advantage of these routes, they must display increasingly specialized adaptations as read from first to last: parenteral, via the blood, via the lymphatic systems, and up the peripheral nerve axons. Ordering of blood and lymphatic system was arbitrary and not intended ot imply that one serves as a significantly more difficult portal to take advantage of than the other. Disease Prevention Primary prevention - early intervention to avoid initial exposure to agent of disease preventing the process from starting Secondary prevention - during the latent stage (when the disease has just begun), process of screening and instituting treatment may prevent progression to symptomatic disease Tertiary prevention - during the symptomatic stage (when the patient shows symptoms), intervention may arrest, slow, or reverse the progression of disease Cook meat, poultry, and eggs thoroughly. Don't cross-contaminate one food with another. Chill and refrigerate leftovers promptly. Clean and wash all produce. Report suspected food-borne illnesses to the local health department. Ten Steps to Investigating an Outbreak Remember that this is a conceptual order, so steps have to be done simultaneously! 1. Prepare for Field Work 2. Establish the Existence of an Outbreak - Consider Severity, Potential for Spread, Public Concern, and Availability of Resources 3. Verify the Diagnosis 4. Define and Identify Cases - Case Definition and Line Listing 5. Describe and Orient the Data in Terms of Person, Place, and Time - Descriptive Epidemiology 6. Develop Hypotheses (Agent/Host/Environment Triad) = Chain of Transmission 7. Evaluate Hypotheses - Analytical Studies (MUST Have a Control Group) 8. Refine Hypotheses and Carry Out Additional Studies 9. Implement Control and Prevention Measures (ASAP!) 10. Communicate Findings Ten Steps to Outbreak Investigation - Explanation of Steps