Imaging Spectrum of Spinal Intramedullary Lesions
advertisement
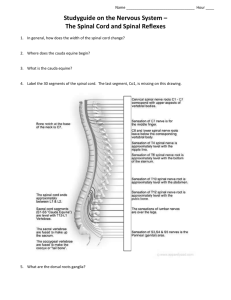
eEdE#: 243C Imaging Spectrum of Spinal Intramedullary Lesions Sagar M Patel DO Alicia Huang MD Francisco Delara MD Daniel R Lefton MD Mount Sinai St. Luke’s - Roosevelt Hospital Center Icahn School of Medicine 1000 Tenth Avenue, New York, NY 10019, USA DISCLOSURE STATEMENT No authors have any significant relationships, financial or otherwise, to disclose. INTRODUCTION/PURPOSE Pathological processes of the spinal cord can produce distinct clinical syndromes yet frequently have both clinical and imaging overlap. A spectrum of diagnostic considerations that may affect the spinal cord includes developmental anomalies, inflammatory and infectious processes, degenerative conditions, vascular disease, as well as benign and malignant neoplasms. The purpose of this exhibit is to describe relevant anatomy important for interpretation as well as present typical and atypical imaging findings of various pathological entities. METHOD An overview of the normal anatomy of the spine with compartmental classification will initially be provided with diagrammatic representation of cross sectional anatomy of the cord and its blood supply. A spectrum of intramedullary lesions will be discussed through a pictorial essay. DISCUSSION 1. 2. Anatomy 3. Neoplasms A. Glial Neoplasms I. Ependymoma II. Astrocytoma i. Juvenile Pilocytic 4. Astrocytoma ii. Anaplastic Astrocytoma iii.Glioblastoma Multiforme III. Ganglioglioma IV. Subependymoma B. Non-glial Neoplasms I. Hemangioblastoma II. Intramedullary Metastasis 5. III. Solitary fibrous tumor IV. Spinal cord lipoma Vascular A. Cavernous malformation B. Spinal dural arteriovenous fistula C. Arterial venous malformation D. Spinal cord ischemia/infarction Inflammatory/Infection A. B. C. D. E. F. Multiple Sclerosis Neuromyelitis Optica Lupus Myelitis Granulomatous Angiitis Neurosarcoid Tuberculosis Trauma/Degenerative A. Spinal cord contusion SPINAL CORD ANATOMY Compartments of the spinal cord Extradural Epidural space, vertebral bodies, neural arches, intervertebral discs, paraspinous muscles Intradural Subarachnoid space, spinal cord ligaments, nerve roots, cauda equina, filum terminale Intramedullary spinal cord, pia Arterial supply of the spinal cord Anterior spinal artery Originates from the intradural vertebral arteries, supplying anterior 2/3 of the cord. Posterior spinal arteries Originates from the posterior rami of the vertebral arteries, supplying posterior 1/3 of the cord. Aorta Segmental artery dorsal artery radicular artery Artery of Adamkiewicz – dominant thoracic anterior radicular artery (medullary feeder), arises from intercostal branches of thoracic aorta, typically left T9 level. Largest radiculomedullary artery of the cervical spinal cord is supplied by the artery of Lazorthes, typically at the C5 or C6 segment. “Watershed” of the cord is the central gray matter NEOPLASMS Spinal intramedullary neoplasms account for about 4%–10% of all central nervous system (CNS) tumors and about 2%–4% of CNS glial tumors. Account for 20% of all intraspinal tumors in adults and 35% of all intraspinal tumors in children. Intramedullary spinal neoplasms are more common in patients with NF-1 (astrocytomas), NF-2 (ependymomas), and VHL (hemangioblastomas). 70% of tumors are associated with cysts. Two types of recognized cysts: Intratumoral cysts: Contained within the tumor itself Typically demonstrate peripheral enhancement Most commonly occurs in ganglioglioma (46%), ependymoma (22%), astrocytoma (21%), and hemangioblastoma (2-4%) Non-tumoral cysts: Occurs at the rostral or caudal aspect of the tumor Occurs due to dilatation of the central canal Does not enhance Present in 60% of all intramedullary spinal tumors Syrinx occurs in approximately 50% of all intramedullary tumors but is most frequently associated with hemangioblastomas. In contrast to intracranial neoplasms, the vast majority of spinal cord neoplasms, including even low-grade forms, enhance after the administration of contrast material to some degree. Enhanced areas probably represent more active portions of the tumors and may indicate potential sites for biopsy if resection is not feasible. EPENDYOMOMA Most common intramedullary neoplasm in adults, comprising 60% of all glial spinal cord tumors. Second most common intramedullary neoplasm in the pediatric population, representing 30% of pediatric intramedullary spinal neoplasms. Classified as WHO Grade I or II neoplasm. Most commonly occurs in the cervical region (4467%). Characterized by slow growth and tends to compress rather than infiltrate adjacent spinal cord neural tissue. Well circumscribed lesion that almost always has a cleave plane, which facilitates microsurgical resection (treatment of choice). Symmetric cord expansion as it arises from the ependymal cells of the central canal within the spinal cord. Rostral and caudal non-tumoral polar cysts are common (Intratumoral cysts are less common). Intratumoral hemorrhage, cystic degeneration, and hemosiderin cap is common. Unlike intracranial ependymomas, calcifications are uncommon. Multiple ependymomas can be seen in the setting of NF-2 (MISME Syndrome – Meningioma, Schwannoma, and Ependymoma). Sagittal T2WI with hemosiderin capping of an ependymoma. Sagittal post-contrast T1WI, sagittal T2WI, and axial C+ T1WI demonstrates focal expansion of the cervical spinal cord with a centrally enhancing mass. Sagittal post-contrast T1WI of the cervical spine demonstrates multiple ependymomas in the setting of NF-2 (MISME Syndrome). ASTROCYTOMA Characterized as: 1. WHO Grade I – Juvenile Pilocytic Astrocytoma 2. WHO Grade II – Fibrillary Astrocytoma 3. WHO Grade III – Anaplastic Astryocytoma 4. WHO Grade IV – Glioblastoma Multiforme (GBM) Population Most common in children, 2nd most common tumor in adults. Location Ependymoma Astrocytoma Adult Pediatric Central Eccentric Wellcircumscribed Ill-defined Comprises approximately 40% of spinal tumors. Morphologic Appearance Generally large, diffuse fusiform enlargement without obvious (infiltrative) margins. Hemosiderin Cap Common Rare Patchy ill-defined enhancement. Can involve the full diameter of the cord but are more eccentric in location compared to ependymomas. Enhancement Intense, homogeneous Patchy, irregular Common Common Both polar and intratumoral cysts are common. Leptomeningeal spread in seen in 60% of intramedullary GBM. Amount and degree of pleomorphism is correlated with the biologic behavior of these tumors. Cysts JUVENILE PILOCYTIC ASTROCYTOMA Sagittal T2WI and post-contrast T1WI of the thoracic spine demonstrates a long segment heterogeneously enhancing mass with rostral and caudal syrinx formation. Thin, linear glial bands are noted within the syrinx. Sagittal T2WI and post-contrast T1WI demonstrate a focal enhancing heterogeneous hyperintense mass in the ventral cervical spinal cord. Confluent pial enhancement of the spinal cord is observed consistent with subarachnoid dissemination of disease. ANAPLASTIC ASTROCYTOMA Intramedullary anaplastic astrocytoma. Sagittal T2WI, sagittal post-contrast T1WI, and axial T2WI demonstrate fusiform enlargement of the distal thoracic spinal cord with mild increased T2 signal. No significant intramedullary enhancement is observed. Engorgement of the venous arcade around the conus is present. GLIOBLASTOMA MULTIFORME Intramedullary Gliobastoma Multiforme. Sagittal T2WI, sagittal post-contrast T1WI, axial T2WI and axial post-contrast T1WI, demonstrates fusiform expansion of the central thoracic spinal cord with abnormal heterogeneous T2 signal. Post-contrast images demonstrate peripheral enhancement with irregular margins. GANGLIOGLIOMA Most frequent in children and young adults. Most commonly occurs in the cervical cord however, holocord involvement is common. Classified as WHO Grade I or II neoplasm. Second most common intramedullary tumor in children after astrocytoma. Consists of large mature neurons, ganglion cells, and neoplastic glial cells. Eccentric in location and commonly contains polar and intratumoral cysts. Patchy enhancement is the most common pattern, but enhancement of the pial surface is also common. Approximately 15% of these lesions show no enhancement. Characteristically involves eight or more vertebral segments. Mixed signal intensity on T1 weighted images is common. Sagittal post-contrast T1WI and sagittal T2WI demonstrates marked widening of the cervicothoracic spinal canal with a long segment enhancing heterogenous intramedullary mass with rostral and caudal polar cysts. SUBEPENDYMOMA Uncommon entity occurring mostly in adult males with less than 50 cases reported in the literature. Believed to arise from tancytes cells that bridge the pial and ependymal layers. Usually manifests with fusiform dilatation of the spinal cord with well-defined borders. Unlike ependymomas, they are eccentrically located and often have bands of normal spinal cord tissue traversing the tumor. Sagittal T2WI, post-contrast T1WI, and axial T2WI demonstrate a T1 isointense, T2 hyperintense intramedullary lobulated tumor with eccentric cord expansion in the mid thoracic spine. HEMANGIOBLASTOMA Third most common intramedullary spinal neoplasm – 1 to 7%. Subpial, highly vascular, capillary rich low grade neoplasm. Multiple lesions indicate the manifestation of VHL syndrome (75% sporadic; 25% associated with VHL). Typically posterior in location. 25% are solid but can present with classic “cystic mass with an enhancing mural nodule” appearance. There is marked enhancement of the solid component. The cystic component does not enhance. Intratumoral arterial flow voids as well as posterior draining veins can be seen. Extensive surrounding edema. Commonly associated with cysts and syrinx. Spinal angiography demonstrates feeding arteries, tumor blush, and draining veins. Sagittal post-contrast T1WI and T2WI demonstrate an intensely enhancing mass in the dorsal cervical cord with peritumoral syrinx formation consistent with a hemangioblastoma. Sagittal post-contrast T1WI and angiographic image demonstrate an avidly enhancing hemangioblastoma with rostral flow voids with corresponding feeding arteries and draining vein. INTRAMEDULLARY SPINAL METASTASIS Accounts for 3-5% of cases of myelopathy in patients diagnosed with cancer. Results from tumor growth along the VirchowRobin spaces and through hematogenous dissemination. Mild cord expansion over several segments with homogeneous enhancement. Typically presents with surrounding edema, usually disproportionately increased for the size of the lesion. Most common intramedullary spinal metastasis (in order of frequency): Lung Breast Melanoma Colorectal Renal Gastric Sagittal T2WI, sagittal post-contrast T1WI, axial T2WI, and axial post-contrast T1WI demonstrate symmetric cord expansion with an avidly enhancing lesion in the distal spinal cord with surrounding edema and mild syrinx formation. Findings were consistent with an intramedullary melanotic metastasis. SOLITARY FIBROUS TUMOR Spindle-cell neoplasm of probable mesenchymal origin. Most commonly arises from the pleura, however extrapleural CNS solitary fibrous tumors can be seen originating from the dura, spinal cord parenchyma, and nerve roots. MR findings include: T1 isointense/hypointense T2 hypointense T1 post-contrast: avid and homogenous enhancement T2 hypointensity is caused by hypocellularity and abundant collagen stroma that helps distinguish from other spinal cord neoplasms. Peritumoral edema is commonly seen. Differential diagnostic considerations include meningioma and schwannoma. Sagittal T2WI, coronal post-contrast T1WI, axial T2WI, and axial post-contrast T1WI demonstrate a well-circumscribed eccentric intramedullary focal mass lesion with low T2 signal, mild peritumoral cord edema, and homogenous enhancement in the upper thoracic cord. Histopathologic correlation status post resection confirmed the diagnosis of solitary fibrous tumor. SPINAL CORD LIPOMA More commonly identified in the first three decades of life. Most commonly located in the thoracic spine. If the spinal cord lipoma is located in the lumbar region, it is usually associated with myelodysplasia or tethered cord. Should be followed in neonates as they can grow significantly during infancy. MRI characteristics: T1WI high signal T2WI lower signal Dark on fat suppression Fat-like lesions Ddx Epidural lipomatosis* Melanoma Neurenteric cysts Pantopaque* Ruptured dermoid* Subacute hemorrhage Teratoma* *suppresses with fat sat Two sagittal T1WI and sagittal T2WI demonstrate a lobulated, multi-segment dorsal cervical spinal cord lesion with hyperintense T1 signal and mild hyperintense T2 signal, consistent with an intramedullary lipoma. CAVERNOUS MALFORMATION Angiogenically immature vascular lesion with lobulated, thin, sinusoidal vascular channels and no interspersed neural tissue. Usually presents in patients aged 30-50. Predilection toward females by a ratio of 4:1. Can cause hematomyelia and BrownSequard syndrome. Minimal cord expansion and edema unless there has been recent hemorrhage. MRI is the study of choice for evaluation: Heterogeneous signal intensity on T1WI and T2WI from methemoglobin. Varying age of blood products give typical “popcorn appearance.” Low signal intensity rim on T2WI and hypointense “blooming” on gradient echo sequence due to hemosiderin. Angiography is typically negative. Axial T2WI demonstrate mild cord expansion secondary to an eccentric hyperintense lesion with a thin hypointense hemosiderin peripheral rim. Axial pre-contrast T1WI demonstrates heterogeneous blood products. Sagittal T1WI and sagittal T2WI demonstrates a predominately hyperintense heterogeneous mass at the cervicomedullary junction with a thin peripheral hypointense hemosiderin rim. A formation of a caudal syrinx (hematomyelia) is noted. ARTERIOVENOUS FISTULA/MALFORMATIONS There are four types of spinal AV malformations Type I Spinal Dural AV Fistula: Most common and usually affects a single radicular feeder. Usually located at the nerve root sleeve. Foix-Alajuoanine refers to the syndrome when myelopathy is present. Symptoms are typically insidious in onset with lower extremity weakness and/or sensory changes. Can cause venous hypertension of the cord. Type II Intramedullary Spinal Cord AV Malformation: Typically presents in the 3rd decade with a M:F ratio of 1:1.1. Typically located in the cervical or thoracic region. There are multiple arterial feeders from both the anterior and posterior arteries. Hemorrhage may occur and cause acute symptoms. Nidus is located within the spinal cord. Commonly associated with spinal artery aneurysms. IMAGING: recommend contrast enhanced MRI; consider spinal angiography +/embolization. T1WI – heterogeneous from blood products T2WI – cord hyperintensity from edema, gliosis or ischemia STIR – flow voids and edema in cord T2* GRE – more sensitive to blood products of AVM hemorrhage Variable enhancement of nidus, cord, and vessels MRA – dynamic enhanced MRA can define the feeding artery and vein Type III Juvenile AV Malformation: Has intramedullary, extramedullary and extraspinal components. Occurs early in life and has a poor prognosis. Type IV Spinal Cord AV Fistula: Located intradurally but along the ventral or lateral surface of the cord. Varied presentation: myelopathy or hemorrhage including subarachnoid hemorrhage. 20 DURAL ARTERIOVENOUS FISTULA Axial and sagittal T2WI of the thoracic spine demonstrates spinal cord edema and/or gliosis secondary to venous hypertension. Sagittal postcontrast T1WI demonstrates abnormally prominent enhancing vascularity along the surface of the spinal cord secondary to venous engorgement. ARTERIOVENOUS MALFORMATION Axial and sagittal T2WI (left two images) and T1WI (right two images) of the cervical spine demonstrate a heterogeneously T1 and T2 low signal intensity mass within the posterior aspect of the spinal cord at the levels of C4-C6. Low T1and T2 signal represent flow voids. The spinal cord demonstrates mild T2 hyperintensity compatible with edema and/or gliosis. SPINAL CORD INFARCT Spinal cord infarcts have a predilection for upper thoracic or thoracolumbar regions due to the limited blood supply (watershed region). Up to 50% of cases have no known etiology. Majority of known causes are related to aortic pathology (atherosclerotic disease). Other causes include septicemia, systemic hypotension, fibrocartilaginous embolism, and iatrogenic etiology. Patients typically present with abrupt onset of symptoms with rapid progression. The dominant blood supply to conus: Artery of Ademkiewicz Infarction of this vessel leads to impairment in bowel and bladder function. Infarcts present with mild cord enlargement and well demarcated region of abnormal signal. Cord atrophy can be seen in chronic infarcts. Hemorrhagic transformation is rare. MRI findings: T2WI hyperintense central gray matter Restricted diffusion Sagittal T2WI and sagittal post-contrast T1WI as well as two axial T2 WI demonstrate mild cord expansion and sharply demarcated region of increased T2 signal involving the distal thoracic spinal cord extending from T9 through the conus. The cord signal abnormality predominantly involves the anterior and midline of the distal spinal cord and is sharply demarcated from the uninvolved posterior thoracic spinal cord. There is no associated enhancement of the cord. Given the reported history of acute onset of symptomatology, these findings are consistent for ischemia of the cord, i.e. cord infarction. MULTIPLE SCLEROSIS Multiphasic primary demyelinating disease of the CNS with multiple lesions disseminated over time and space. Peak onset: 20-40 years of age; F>M 1.7:1. Majority of patients have associated intracranial lesions (5-24% of cases are confined to the spinal cord). 60% of spinal lesions are located in the cervical region. Lesions are peripherally located (most commonly at the dorsolateral aspect of the cord), oval, and asymmetric. They are usually less than 2 vertebral segments in length and less than half the cross-sectional area of the spinal cord. Wedge-shaped lesions are seen on axial images, with apex directed centrally. Lesions do not respect gray-white boundary. Cord enlargement is uncommon. There can be myelomalacia (parenchymal loss) overtime. MS can cause transverse myelitis. MRI Findings: Presents as T2 hyperintense, T1 isointense lesions. Enhancement is seen in acute demyelination. Enhancement can last 1-2 months but does not reflect disease progression. Axial and sagittal T2WI as well as axial and sagittal post-contrast T1WI demonstrate abnormal signal affecting the mid thoracic spinal cord, predominantly the dorsal columns, with associated patchy ill-defined enhancement. Findings are consistent with an active plaque of multiple sclerosis. LUPUS MYELITIS In patients with an established diagnosis of systemic lupus erythematosus, transverse myelitis can usually be presumed to be caused by the underlying disease. Etiology is proposed to be secondary to vacuolar degeneration from an autoimmune process or ischemia. Mid to low thoracic spine is the most common site of involvement. MR findings include high signal on T2WI and low/isointense signal of T1WI. Enhancement is seen in 50% of the cases. Lack of enhancement does not exclude active disease however may reflect disease remission during periods of clinical improvement or secondary to the stabilizing effect of high dose steroids. Axial T2WI and sagittal T2WI demonstrate mild cord expansion with central abnormal T2 signal. Given patients history of SLE, findings are consistent with lupus myelitis. NEUROMYELITIS OPTICA Autoimmune inflammatory disorder involving myelin of neurons of the optic nerves and spinal cord, without brain parenchymal involvement. Longitudinally extensive (>3 vertebral segments) abnormal signal in the spinal cord with thickening/enhancement of the optic nerve. NMO-IgG seropositivity. On first acute presentation, neuromyelitis optica cannot be differentiated from acute disseminated encephalomyelits in patients with simultaneous optic neuritis and myelitis. Other concomitant or associated disease: Prior viral infection ANA positive (10%) Autoimmune thyroiditis (9%) Myasthenia gravis (2%) Sjogren syndrome Sagittal FLAIR WI, axial T2WI, and sagittal T2WI demonstrate increased thickening and abnormal signal intensity within the optic chiasm as well as longsegment confluent patchy signal within the central thoracic spinal cord, findings which are consistent with neuromyelitis optica. GRANULOMATOUS ANGIITIS OF THE CNS Uncommon necrotizing vasculitis in adults of unknown cause restricted to vessels of the CNS. In the spectrum of Primary Arteritis of the CNS, which also includes benign angiopathy of the CNS and reversible vasoconstrictive syndrome. Diagnosis of exclusion. No evidence of systemic vasculitis. Irregularities, stenoses, and vascular occlusions in atypical pattern for atherosclerotic disease. Ddx: Intracranial atherosclerotic vascular disease, arterial vasospasm, drug abuse, moyamoya, viral infection (such as CMV or Herpes), and systemic CNS vasculitis. Spine: Axial and sagittal T2WI and post-contrast T1WI demonstrate abnormal T2 intramedullary signal without cord expansion in the lower thoracic spinal cord with mild patchy enhancement. There is enhancement of the ventral and dorsal nerve rootlets at the level of the distal thoracic cord, conus medullaris, and cauda equina. Brain: Axial T2WI and post-contrast T1WI demonstrate serpentine, mildly nodular enhancement in a medullary pattern within both frontotemporal and subinsular regions, which is associated with T2 signal abnormality within the adjacent brain parenchyma. There is no appreciable mass effect related to the confluent zones of T2 signal abnormality. Enhancing soft tissue is seen within the subarachnoid space within the frontal and temporal lobe regions. NEUROSARCOID Non-caseating granulomatous disease of the spine. 6-8% of patients with neurosarcoid have spinal cord lesions. Most commonly cervical and upper thoracic in location. Tumor nodules can present on the leptomeningeal surface, as a discrete mass, or as diffuse inflammation. Central intramedullary lesions are from infiltration of the Virchow – Robin spaces. Presents with fusiform cord enlargement, enhancing intramedullary masses, and focal or diffuse T2 hyperintense lesions. Combination of leptomeningeal (smooth or nodular) and peripheral intramedullary mass-like enhancement are highly suggestive of spinal sarcoidosis. Rarely can have calcifications or cysts. Improves with steroid therapy. Four stages of intraspinal sarcoidosis: Early Inflammation – linear leptomeningeal enhancement. Centripetal spread of leptomeningeal inflammatory process through perivascular spaces – parenchymal enhancement and swelling. Less prominent swelling with focal or multiple enhancement. Resolution of inflammatory process with normal size or atrophy of the cord and no enhancement. Sagittal T2WI, sagittal post-contrast T1WI, and coronal post-contrast T1WI demonstrate abnormal enlargement and signal in the spinal cord with enhancing intramedullary lesions as well as scattered nodular leptomeningeal enhancement, consistent with inflammation and noncaseating granulomas in the setting of sarcoidosis. 28 TUBERCULOSIS Granulomatous disease caused by Mycobacterium tuberculosis. Intramedullary tuberculosis is a rare form of spinal tuberculosis, even in tuberculosis endemic regions. Most commonly affects the osseous vertebral elements. Secondary to hematogenous spread from another focus of tubercular infection in the body, usually pulmonary and nodal disease. Occurs predominantly in young patients. Cinical presentation ranges from back pain to paraparesis and bowel/ bladder dysfunction with or without low grade fever. Clinical picture of compressive myelopathy usually warrants MRI evaluation in these patients. Can present with myelitis without identifiable granulomas on the precontrast scan. Appears as a diffuse ill-defined hyperintensity on T2WI and hypointensity on T1WI. Post-contrast T1WI usually demonstrates nodular or ring enhancing lesions. Sagittal T2WI and post-contrast T1WI demonstrates a long segment ill-defined regional of abnormal T2 signal with multiple underlying contiguous enhancing solid nodular lesions within the posterior cervical spinal cord. 29 SPINAL CORD CONTUSION Spinal cord contusion in adults are typically located at C4-C6 and associated with a fracture or subluxation in young adults. Degenerative disease predisposes the elderly population to spinal cord injury. Spinal cord edema without radiographic abnormality can be seen in children less than eight years old due to ligamentous laxity. Incidence in the setting of trauma is 3.7%. Good neurological prognosis if no hemorrhage is present. Poor prognostic factors: hematoma, C4-C6 injuries,greater than 50 years of age. Usually occult on CT. MRI findings: T1WI: acute: isointense/hypointense with cord swelling, hyperintense after 3 days if there is a hematoma; chronic: atrophy +/- cyst, syringomyelia. T2WI: acute: hyperintense from edema that worsens over a few days, then plateaus; chronic: atrophy, hyperintense gliosis, +/- cyst, syringomyelia, hypointensity from hemosiderin if there is a chronic hematoma. Sagittal STIR *key sequence: cord edema, ligamentous injury. T2*: hypointense if there is hemorrhage. DWI: restricted diffusion can show early ischemic changes. MRA/CTA can be obtained to evaluate for vascular injury. Sagittal T2WI and STIRWI demonstrates focal short segment cord abnormal signal signal at the level of C4-C5, consistent with cord contusion. There is associated disc herniation at these levels and edema in the posterior elements, suggestive of ligamentous injury. CONCLUSION After review of this educational exhibit, the reader will have an informed understanding of the normal anatomy of the spinal cord and characteristic imaging findings of various intramedullary spinal pathologies. REFERENCES Alblas CL et al. Acute spinal-cord ischemia: evolution of MRI findings. Journal of Clinical Neurology. 2012;8:218223. Borg B. Intramedullary Mass. Statdx.com. Accessed February 11th, 2015. Eddleman CS et al. Advanced noninvasive imaging of spinal vascular malformations. Neurosurgical Focus. 2009;26:E9 Ellingson BM, Salamon N, and Holly LT. Imaging techniques in spinal cord injury. World Neurosurgery. 2014;82:1351-1358 Koeller KK, et al: Neoplasms of the Spinal Cord and FilumTerminale: Radiologic-Pathologic Correlation. Radiographics. 20:1721-1749, 2000. Krings T, and Geibprasert S. Spinal dural arteriovenous fistulas. American Journal of Neuroradiology. 2009;30:639-648. Pretorius PM. The role of MRI in the diagnosis of MS. Clinical Radiology. 2003;58:434-448 Rubin MN and Rabinstein AA. Vascular diseases of the spinal cord. Neurologic Clinics. 2013;31:153-181 Yousem DM, Grossman RI. Neuroradiology: The Requisites, 3rdEd. Philadelphia, PA: Mosby, 2010. Print. Hakan A et al. Primary Angiitis of the Central Nervous System and Silent Cortical Hemorrhages. American Journal of Neuroradiology. 2002;23:1561-1563 Hussam JE et al. Subependymoma of the Spine. Neurosciences. 2010;15:126-128.