In the term SGA fetus with normal umbilical artery Doppler, an
advertisement
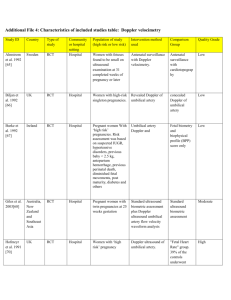
Why umblical artery doppler Venous doppler DV and umbilical vein Arterial doppler umbilical aorta middlde cereberal artery How assess the umbilical artery doppler Location where the cord is sampled — The indices are higher at the fetal than at the placental end of the cord [11]. For PW Doppler, a mid-level free floating loop of the cord should be used for sampling when the site of Doppler sampling can be selected. Others recommend using the fetal end of the umbilical cord [13]. The clinical significance of these variations in measurement technique remains unclear Management of increased PI in umbilical artey When defined by customised fetal weight standards 81% of SGA fetuses have a normal umbilical artery Doppler.141 Outpatient management is safe in this group142 and it may be reasonable to repeat Doppler surveillance every 14 days; one small randomised trial involving 167 SGA fetuses with normal umbilical artery Doppler investigated frequency of surveillance; twice–weekly compared to two weekly monitoring resulted in earlier deliveries and more inductions of labour with no difference in neonatal morbidity. When umbilical artery Doppler flow indices are abnormal (pulsatility or resistance index > +2 SDs above mean for gestational age) and delivery is not indicated repeat surveillance twice weekly in fetuses with end–diastolic velocities present and daily in fetuses with absent/reversed end–diastolic frequencies. In SGA fetuses with abnormal umbilical artery Doppler where there is not an indication for delivery the optimal frequency of surveillance is unclear. Until definitive evidence becomes available it is reasonable to repeat surveillance twice weekly in fetuses with end–diastolic velocities present and daily in fetuses with absent or reversed end–diastolic velocities (AREDV). Up to date Increased pI 0r AEDV After or 34 deliver before 34 Daily doppler and nst BPP Before 34 Revesed UA flow or non reassuring BBP deliver High pi and after 34 A high or increasing DI in the presence of end-diastolic flow warrants more intensive fetal surveillance, such as weekly umbilical Doppler ultrasound and once or twice per week NST, BPP, or modified BPP, as dictated by the clinical condition. If fetal surveillance tests indicate fetal compromise (eg, nonreactive NST, poor fetal heart rate baseline variability, persistent late decelerations, oligohydramnios, or BPP score <4), delivery should be strongly considered, with the mode of delivery determined by obstetrical factors (eg, gestational age, presentation, fetal heart rate tracing) and maternal factors (eg, medical complications, cervical status). Individualized management Application of the BPP to the growth restricted fetus remote from term may be less reliable since the preterm fetus may not have achieved maturity of the biophysiologic processes measured by this test. Furthermore, although many large observational studies have demonstrated the usefulness of the BPP in antepartum fetal assessment, there is a paucity of evidence derived from randomized trials Frequency of fetal surveillance Weekly Doppler should be complemented by twice weekly BPP or another combination of two antenatal tests (nonstress test and modified BPP or BPP) when FGR is complicated by oligohydramnios, preeclampsia, deceleration of fetal growth, increasing umbilical Dopper index, or other complications, even when umbilical artery end diastolic flow is present. c In the term SGA fetus with normal umbilical artery Doppler, an abnormal middle cerebral artery Doppler (PI < 5th centile) has moderate predictive value for acidosis at birth and should be used to time delivery. Cerebral vasodilatation is a manifestation of the increase in diastolic flow, a sign of the ‘brain–sparing effect’ of chronic hypoxia, and results in decreases in Doppler indices of the middle cerebral artery (MCA) such as the PI. Reduced MCA PI or MCA PI/umbilical artery PI (cerebroplacental ratio) is therefore an early sign of fetal hypoxia in SGA fetuses.162– An axial section of the brain, including the thalami and the sphenoid bone wings, should be obtained and magnified. Color flow mapping should be used to identify the circle of Willis and the proximal MCA . The pulsed-wave Doppler gate should then be placed at the proximal third of theMCA, close to its origin in the internal carotid artery (the systolic velocity decreases with distance from the point of origin of this vessel). • The angle between the ultrasound beam and the direction of blood flow should be kept as close as possible to 0◦ (Figure 6). • Care should be taken to avoid any unnecessary pressure on the fetal head. • At least three and fewer than 10 consecutive waveforms should be recorded. The highest point of the waveform is considered as the PSV (cm/s). • The PSV can be measured using manual calipers or autotrace. The latter yields significantly lower medians than does the former, but more closely approximates published medians used in clinical practice11. PI is usually calculated using autotrace measurement, but manual tracing is also acceptable. No systematic reviews of effectiveness of MCA Doppler as a surveillance tool in high risk or SGA fetuses were identified. A systematic review of 31 observational studies (involving 3337 fetuses) found that MCA Doppler had limited predictive accuracy for adverse perinatal outcome (LR+ 2.79, 95% CI 1.10–1.67; LR– 0.56, 95% CI 0.43–0.72) and perinatal mortality (LR+ 1.36, 95% CI 1.10–1.67; LR– 0.51, 95% CI 0.29–0.89).16 Reduce MCA Pi 1 to 3 weeks before abnormal biophysical profile Use for timing delivery is limited Most studies investigating MCA Doppler as a predictor of adverse outcome in preterm SGA fetuses have reported low predictive value MCA Doppler may be a more useful test in SGA fetuses detected after 32 weeks of gestation where umbilical artery Doppler is typically normal In one study of 210 term SGA fetuses with normal umbilical artery Doppler, MCA PI < 5th centile was predictive of caesarean section for nonreassuring fetal status (OR 18.0, 95% CI 2.84–750) and neonatal metabolic acidosis, defined as umbilical artery pH < 7.15 and base deficit > 12 mEq/L (OR 9.0, 95% CI 1.25–395).173 Based on this evidence it is reasonable to use MCA Doppler to time delivery in the term SGA fetus with normal umbilical artery Doppler. A Ductus venosus Doppler has moderate predictive value for acidaemia and adverse outcome. • The ductus venosus (DV) connects the intra-abdominal portion of the umbilical vein to the left portion of the inferior vena cava just below the diaphragm. The vessel is identified by visualizing this connection by 2D imaging either in a midsagittal longitudinal plane of the fetal trunk or in an oblique transverse plane through the upper abdomen. • In early pregnancy and in compromised pregnancies particular care has to be taken to reduce the sample volume appropriately in order to ensure clean recording of the lowest velocity during atrial contraction. Observational studies have identified venous Doppler as the best predictor of acidaemia What is the optimal gestation to deliver the SGA fetus? RCOG In the preterm SGA fetus with umbilical artery AREDV detected prior to 32 weeks of gestation, delivery is recommended when DV Doppler becomes abnormal or UV pulsations appear, provided the fetus is considered viable and after completion of steroids. Even when venous Doppler is normal, delivery is recommended by 32 weeks of gestation and should be considered between 30–32 weeks of gestation. C If MCA Doppler is abnormal delivery should be recommended no later than 37 weeks of gestation. Timing delivery is therefore a critical issue in order to balance the risks of prematurity against those of continued intrauterine stay; death and organ damage due to inadequate tissue perfusion. Given the mortality associated with umbilical artery AREDV alone delivery should be considered based on this finding alone after 30 weeks of gestation and recommended no later than 32 weeks of gestation FMF After 34 weeks; high PI in umbilical artery or high PI in ductus venosus or low PI in MCA or AFI below 5 31-33 weeks : absent end diastolic flow in UA or absenta wave in DV or deepest pocket of AF less than 2 cm 28-30 weeks: reversed a wave in DV or reversed end distolic flow in UA and deepest pocket of AF less than 2 cm and no movement Less than 28 :reversed a wave in DV ,and reversed end diastolic in UA and deepest pocket of AF less than 2 cm How should the SGA fetus be delivered? In the SGA fetus with umbilical artery AREDV delivery by caesarean section is recommended. In the SGA fetus with normal umbilical artery Doppler or with abnormal umbilical artery PI but end–diastolic velocities present, induction of labour can be offered but rates of emergency caesarean section are increased and continuous fetal heart rate monitoring is recommended from the onset of uterine contractions.B