Neurological System - Blog Unsri
advertisement
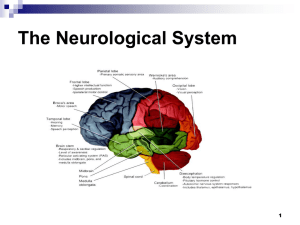
Neurological System dear d34r123@yahoo.co.id KOMUNITAS BLOGGER UNIVERSITAS SRIWIJAYA Neurological System Sympathetic division prods body into action during times of physiologic and psychologic stress. Parasympathetic division functions in complementary and counterbalancing manner to conserve body resources and maintain day-to-day functions such as digestion and elimination. Three major units of the brain are: cerebrum, cerebellum, brainstem Cranial Nerves Function Olfactory (I) Sensory Not checked unless suspected problems – test for patency Test ability to identify familiar aromatic odors, eyes closed, one naris at a time Sense of smell may diminish with age Anosmia – loss of sense of smell or inability to discriminate odors Optic (II) Sensory Central vision - checked with Snellen Chart Test visual fields by confrontation and extinction of vision Oculomotor (III) Motor Inspect eyelids for drooping Trochlear (IV) Motor Pupils’ size for equality and their direct and consensual response Trigeminal (V) Motor / Sensory Check chewing for muscle tone and strength, superficial pain and touch sensation (sharp, dull); test corneal reflex Abducens (VI) Motor Test extraocular eye movements Facial (VII) Motor / Sensory Test for facial movement and symmetry; check anterior 2/3 of tongue (salty/sweet) Acoustic (VIII) Sensory Test sense of hearing with whisper test; test for bone and air conduction and lateralization of sound with Weber Test (tuning fork) Vestibular function is tested with Romberg Test (stand still w/eyes closed) Glossopharyngeal (IX) Motor / Sensory Test ability to identify sour and bitter and swallowing and gag reflex Vagus (X) Motor / Sensory Observe for swallowing difficulty; evaluate guttural speech sounds – speaking; inspect palate and uvula movement Spinal Accessory (XI) Motor Test for trapezius and sternocleidomastoid muscle strength Hypoglossal (XII) Motor Inspect tongue symmetry, movement and strength; evaluate quality of speaking On Old Olympus’ Towering Tops A Finn And German Viewed Some Hops Spinal Nerves – 31 pair arise from spinal cord and exit at each intervertebral foramen dermatome - sensory and motor fibers of each spinal nerve supply and receive information in a specific body distribution Developmental Variations Infants and Children - primitive reflexes are present in newborn: yawn, sneeze, hiccup, blink at bright light and loud sound, papillary constriction with light and withdrawal from painful stimuli motor control of head and neck develops first, followed by trunk and extremities - brain growth continues until 12 – 15 yrs old Pregnant Women - physiologic alterations that may occur are: contraction or tension headaches and acroparesthesia (numbness and tingling of hand) which may be confused with carpal tunnel syndrome - during 1st trimester, increase in naptime and sleeptime, but may not feel rested even with increased sleep - late in pregnancy, more frequent night awakenings and less sleep time Older Adults - changes are more physiologic than anatomic - cerebral neurons decrease beginning at 50 - velocity of nerve impulse conduction declines so that responses to various stimuli take longer - sensory perceptions of touch and pain stimuli may be diminished II. Subjective Assessment A. History of Present Illness Seizures or Convulsions – sequence of events; level of consciousness (LOC); muscle tone, relationship of seizure to time of day, meals, fatigue, emotional stress, excitement, menses, and discontinuing medications or poor compliance with medications; activity before attack; frequency; medications (anticonvulsants, alternative or complementary therapies, antidepressants, tranquilizers, antitremor) Pain – onset, quality and intensity, location or path, efforts to treat Gait Coordination – balance, falling, legs simply give way, stiffness of limbs, associated problems (rheumatoid arthritis, stroke, sensory changes) Weakness or Paresthesia – onset, character (generalized, ascending or transient), associated symptoms (tingling, limb feels encased in tight bandage, SOB, stiffness of joints, spasms), concurrent chronic illness such as HIV, nutritional or vitamin deficiency Vertigo, dizziness, loss of balance Difficulty Swallowing B. Past Medical History Trauma – head, spinal cord, or localized injury; CNS insult; birth trauma; cerebrovascular accident or stroke Meningitis, encephalitis, plumbism, poliomyelitis Deformities, congenital anomalies Neurologic disorder, brain surgery, residual effects Psychiatric Counseling Cardiovascular, circulatory problems: HTN, aneurysm, stroke C. Family History Hereditary Disorders – muscular dystrophy, Tay-Sachs disease Alcoholism Mental Retardation Epilepsy or seizure disorder, headaches Alzheimer Disease Learning Disorders Weakness or gait disorders Medical or Metabolic Disorder – thyroid disease, HTN, diabetes D. Personal and Social History Environmental or Occupational Hazards – exposure to lead, arsenic, insecticides; operate farm or other dangerous equipment; work at heights or in water Hand, Eye, Foot dominance; family patterns of dexterity and dominance Ability to care for self – hygiene, ADL, finances, communication, shopping Sleeping or Eating Disorders Use of alcohol or street drugs (especially mood-altering drugs) III. Objective Assessment A. Test Cranial Nerves (See Chart) B. Observe Balance, Coordination, and Gait 1. Rapid Rhythmic Alternating Movements – have patient pat knees, alternately turning up palm and back of hands and increasing rate gradually - have patient touch thumb to each finger on same hand (index finger to little finger and back) - observe for stiff, slowed, nonrhythmic, or jerky clonic movements 2. Accuracy of Movements – finger-to-finger test performed with pt’s eyes open - use index finger and alternately touch nose then your finger (changing location several times) - movements should be rapid, smooth, and accurate finger-to-nose test performed with pt’s eyes closed, touching nose alternating with index finger of each hand and gradually increasing speed - movements should be smooth, rapid, and accurate - heel-to-shin test performed with pt standing, sitting or supine, running heel of one foot up and down shin (knee to ankle) of opposite leg - should move heel up and down shin in straight line, without irregular deviations to side 3. Balance a. Equilibrium – Romberg Test, with eyes open then closed, have patient stand, feet together and arms at sides - slight swaying is expected, but not to extent that there is danger of falling loss of balance is positive sign - with staggering or loss of balance, postpone other tests test with pt standing with feet slightly apart, push shoulders with enough effort to throw him/her off balance - recovery of balance should occur quickly - test with pt standing on one foot, eyes closed, and arms straight at sides - balance on each foot should be maintained for 5 seconds, but slight swaying is expected - test with eyes open, have pt hop in place first on one foot and then the other - note any instability, need to continually touch floor, or tendency to fall b. Gait – observe walk without shoes, first with eyes open then closed - note simultaneous arm movements and upright posture - note any shuffling, widely placed feet, toe walking, foot flop, leg lag, scissoring, loss of arm swing, staggering or reeling - pt should continuously sequence both stance and swing, step after step - gait should have smooth, regular rhythm and symmetric stride length - trunk posture should sway with gait phase, and arm swing should be smooth and symmetric - heel-toe walking will exaggerate any unexpected findings - pt walk straight line, first forward then backward, w/eyes open, arms at sides - touch toe of one foot with heel of other - note any extension of arms for balance, instability, tendency to fall, or lateral staggering and reeling - consistent contact between heel and tow should occur, slight swaying is expected C. Test for Sensory Abilities - routinely evaluate hands, lower arms, abdomen, feet, and lower legs - sensory discrimination of face is determined with cranial nerve evaluation - each sensory discrimination is tested with pt’s eyes closed - use minimal stimulation initially, increasing gradually - stronger stimulus is needed over back, buttocks, and heavily cornified areas (lower levels of sensitivity) - pt should compare perceived sensations, side to side; there should be: - minimal differences - correct interpretation of sensations (hot/cold, sharp/dull) - discrimination of side of body tested - location of sensation and whether proximal or distal 1. Primary Sensory Functions (Protective) a. Superficial Touch – touch with cotton wisp or fingertips using light strokes - avoid stroking areas w/hair - have pt point to area touched/ tell when felt b. Superficial Pain – alternating sharp and smooth edges of split tongue blade, touch skin in unpredictable pattern - have pt identify each sensation as sharp or dull and where it was felt - combine evaluation of superficial pain and touch c. Temperature – use only when superficial pain sensation is not intact - roll test tubes of hot and cold water alternately against skin, in unpredictable pattern, evaluating temperature sensation - ask pt to indicate which temperature is perceived and where it is felt - deep pressure is tested by squeezing trapezius, calf, or biceps muscle (should experience discomfort) d. Vibration – place stem of vibrating tuning fork against several bony prominences, beginning at most distal joints - buzzing or tingling sensation should be felt - tell when / where vibration is felt e. Position of Joints – hold joint being tested by lateral aspects to avoid giving clue about direction moved - with eyes closed, begin in neutral position, raise or lower digit, and ask pt to tell which way it was moved - return to neutral position proprioception – awareness of body in space 2. Cortical or Discriminative Sensory Functions – tests cognitive ability to interpret sensations - inability should indicate lesion in sensory cortex or posterior columns of spinal cord - eyes should be closed for these procedures a. Stereognosis – hand pt familiar object (key, coin) identify by touch and manipulation tactile agnosia – inability to recognize objects by touch; suggests parietal lobe lesion b. Two-Point Discrimination – with wooden end of two q-tips, alternately touch pt’s skin with one or both points simultaneously at various locations - find distance at which pt can no longer distinguish two points c. Extinction – simultaneously touch check, hand, or other area on each side of body - ask pt to tell you how many stimuli there are and where they are - bilateral sensations should be felt d. Graphesthesia (Number Identification) – with blunt pen or applicator stick, draw letter or number on palm of pt’s hand - ask pt to identify figure - letter should be readily recognized e. Point Location – touch area on pt’s skin and withdraw stimulus - ask pt to point to area touched - no difficulty localizing stimulus to should be noted - performed simultaneously with superficial tactile sensation D. Test for Deep Tendon Reflexes - performed with pt relaxed, either sitting or lying down - focus pt’s attention on alternate muscle contraction (pulling clenched hands apart) - position limb with slight tension on tendon to be tapped - palpate tendon - hold reflex hammer loosely between thumb and index finger and briskly tap tendon with flick of wrist - symmetric visible or palpable responses should be noted 1. Biceps Reflex – (C5, C6) - flex pt’s arm to 45° angle with thumb over tendon and fingers under elbow - palpate biceps tendon - strike thumb with reflex hammer - contraction causes visible or palpable flexion of elbow 2. Brachioradial Reflex – (C5, C6) - flex pt’s arm to 45° angle, strike brachioradial tendon (~1 – 2”above wrist) directly w/ reflex hammer - pronation of forearm and flexion of elbow should occur 3. Triceps Reflex – (C6, C8) - flex pt’s arm to 90° angle and rest pt’s hand against side of body - palpate triceps tendon and strike it directly with reflex hammer, just above elbow - contraction causes visible or palpable extension of elbow 4. Patellar Reflex – (L2, L4) - flex knee to 90° angle, allowing lower leg to hang loosely - support upper leg, not allowing it to rest against exam table - strike patellar tendon just below patella contraction of quadriceps causes extension of lower leg 5. Achilles Reflex – (S1, S2) pt sitting, flex knee to 90° angle with ankle in neutral position, holding heel - pt may kneel on chair with toes pointing toward floor, strike Achilles tendon at ankle level - contraction causes plantar flexion of foot Babinski Sign – plantar response (Dorsiflexion) indicative of pyramidal tract disease in all over 2 yrs - fanning of toes and dorsiflexion of great toe - found until 16 – 24 mos 6. Meningeal Signs – nuchal rigidity = stiff neck, sign associated with meningitis and intracranial hemorrhage - pt supine, raise head, flexing neck - try to make pt’s chin touch sternum, but don’t force it - raising shoulders slightly will help relax neck, making determination of true stiffness - pan and resistance neck motion are associated with nuchal ridigity Brudzinski Sign – neck stiffness - involuntary flexion of hips and knees when flexing neck is positive sign for meningeal irritation Kernig Sign – flex leg at knee and hip with pt supine, attempting to straighten leg - pain in lower back and resistance of straightening is positive sign, indicating meingeal irritation IV. Developmental Variations A. Infants - suspect neurologic problems when child is not doing something we expect them to do, rather than because we find a problem on exam - cranial nerves are not directly tested, observations are made in physical exam - observe spontaneous activity for symmetry and smoothness of movement coordinated sucking and swallowing is function of cerebellum - hands usually held in fists for first 3 months of life, but not constantly - purposeful movement begins at ~2 mos., taking objects with one hand at 6 mos., transferring objects hand to hand at 7 mos., purposefully releasing object by 10 mos. - should be no tremors or constant overshooting of movements withdrawal of all limbs from painful stimulus provides measure of sensory integrity - other sensory function is not routinely tested - patellar tendon reflexes are present at birth Achilles and brachioradial tendon reflexes appear at 6 mos - when testing deep tendon reflexes use finger to tap tendon - posture and movement should be inspected for rhythmic twitching of facial, extremity and trunk musculature, as well as for sustained asymmetric posturing Moro (birth) – infant supported in semi-sitting position, allow head and trunk to drop back to 30° angle - observe symmetric abduction and extension of arms; fingers fan out and thumb and index finger form a C; arms adduct in embracing motion followed by relaxed flexion; legs may follow similar pattern; reflex diminishes in strength by 3 – 4 mos., disappears by 6 mos. Stepping (between birth & 8 wks) – infant upright under arms and allow soles of feet to touch surface - observe alternate flexion and extension of legs, simulating walking; it disappears before voluntary walking B. Children - neurologic exam is done by observing neuromuscular developmental progress and skills displayed during exam - exam of cranial nerves is often by playing a game to elicit response - observe child at play, noting gait and fine motor coordination - beginning walker exhibits wide-based gait - older child walks with feet closer together, with better balance, and recovers more easily with unbalanced - observe skill in reaching for, grasping, and releasing toys - no tremors or constant overshooting movements should be present - heel-to-toe walking, hopping, and jumping are all coordination skills that develop 3 Penny Test (tests vision, extraocular movements, hearing) coin dropped on floor = ask child who is standing to pick it up, testing vision and balance moistened coin on child’s nose = ask child to walk across room, observing gait and any posturing balanced coin = have child balance coin on nose and dorsum of each extended hand, testing Romberg - deep tendon reflexes are not routinely tested because poor cooperation is often a problem - reflexes tested, use same techniques described for adults - responses should be same - evaluate light touch sensation by having child close his/her eyes and point to where you touch or tickle - use tuning fork to evaluate vibration sensation, asking child to point to area where buzzing sensation is felt superficial pain sensation is not routinely tested - when checking cortical sensory integration, use geometric figures - draw each figure twice and ask child if figures are the same or different - practice may be needed with eyes open to get good compliance - soft signs can be found in gross motor, fine motor, sensory, and reflex functional areas - multiple soft signs are often found with learning problems C. Pregnant Women - reflexes increase signs of preeclampsia (HTN usually accompanied with edema and proteinuria) D. Older Adults exam is identical to adult - medications can impair CNS function and cause slowed reaction time, tremors, and anxiety - markedly diminished senses of smell and taste - sweet and salty tastes usually impaired first - common cranial nerve changes include reduced ability to differentiate colors, reduced upward gaze, slower adjustment to lighting changes, decreased corneal reflex, middle to high frequency hearing loss, and reduced gag reflex Tinetti Balance and Gait Assessment Tool – used for any older adult thought to be at risk for falls, or for people who have difficulty performing daily activities (rising from chair, task that involves unsupported standing) - tactile, vibratory sensation and position sense are impaired - may need stronger stimuli to detect sensation - deep tendon reflex changes - less brisk or even absent reflexes w/ response diminishing in lower extremities before upper - Achilles and plantar reflexes may be absent or difficult to elicit - superficial reflexes may disappear increase in benign essential tremor - fine motor coordination and agility may be impaired V. Common Abnormalities A. Multiple Sclerosis – debilitating, degenerative disorder in which blood-brain barrier breaks down and permits immune cells to pass into myelinated white matter of brain or spinal cord tissue - myelin is destroyed and axons no longer permit nerve impulse transmission - brain mass decreases - progression is gradual, with or without remissions - primary symptoms include fatigue, bowel and bladder dysfunction, sexual dysfunction, sensory changes, muscle weakness, and cognitive and emotional changes onset occurs between 20 – 40 yrs old and affects women twice as often as men B. Generalized Seizure Disorder – characterized by episodic, sudden, involuntary contractions of a group of muscles, resulting from excessive discharge of cerebral neurons may be caused by systemic disease, head trauma, toxins, stroke, or hypoxic syndromes disturbances in consciousness, behavior, sensation, and autonomic functioning often occur C. Meningitis – inflammatory process in meninges, caused by bacteria and viruses signs and symptoms include fever, chills, nuchal rigidity, headache, seizures, and vomiting, followed by alterations in LOC - young infants do not demonstrate nuchal rigidity; those affected generally will be very irritable and inconsolable and have fever, diarrhea, poor appetite, and toxic appearance - bacterial form is life-threatening if not rapidly treated with appropriate antibiotics D. Encephalitis – inflammation of brain and spinal cord that also involves meninges - onset is often mild, febrile viral illness followed by disturbance in CNS function and characterized by headache, drowsiness, and confusion, eventually progressing to stupor and coma - motor function may be impaired with severe paralysis or ataxia E. Cerebrovascular Accident (Brain Attack or Stroke) – CVA; sudden, focal neurologic deficit resulting from impaired circulation of brain, associated with cardiovascular disease - thrombosis, embolism, or hemorrhage causes circulation impairment Major Warning Signs: · sudden weakness, numbness, or paralysis of arms or legs, especially one side · sudden blurred vision or blindness in one or both eyes · sudden difficulty speaking, understanding speech, confusion, or slurred speech · sudden severe headache without apparent reason · sudden loss of balance or falling without apparent reason - signs and symptoms include headache, progressive sudden neurologic deficits (restlessness, lethargy, changes in LOC), vital sign and pupil changes, nausea and vomiting, impaired communication, shock, and cardiac arrest F. GuillainBarre’ Syndrome – acute polyneuropathy that commonly follows nonspecific infection that occurred 10 – 14 days earlier and primarily affects motor autonomic peripheral nerves - characterized by ascending symmetric weakness (w/sensation preserved) that increases in severity over days or weeks - motor paralysis and respiratory muscle failure may result, requiring life support - 85% eventually have full functional recovery after recovery period lasting several wks or mos. G. Peripheral Neuropathy – disorder of PNS that results in motor and sensory loss in distribution of one or more nerves sensation of numbness, tingling, burning and cramping - most common cause is diabetes, but may be caused by toxins - moderate to severe diabetic neuropathy has wasting of foot muscles, absent ankle and knee reflexes, decreased or no vibratory sensation below knees, and loss of pain or sharp touch sensation to mid-calf - temperature sensation may be less impaired - loss of pain sensation leads to loss of protective reflex or awareness of injury loss of skin integrity can lead to ulceration and infection - compounded by impaired circulation that results in poor healing and may result in amputation H. Parkinson Disease – slowly progressive, degenerative neurologic disorder of brain’s dopamine neuronal systems - results in poor communication between parts of brain that coordinate and control movement and balance - may be genetic, environmental, viral, vascular, toxic, or other factors associated with onset - pts over 50 are most often affected - symptoms begin with tremors at rest and with fatigue, disappearing with intended movement and sleep, respectively - progresses with tremor of head, slowing of voluntary movements, and bilateral pillrolling of fingers - motor impairment causes delays in execution of movement, masked facial expression, and poor blink reflex - muscular rigidity interferes with walking, leading to gait of short, shuffling steps with trunk in forward flexion posture - speech becomes slowed, slurred, and monotonous - behavioral change and dementia occur in 10 – 15% DOWNLOAD