NEUROLOGICAL DISORDERS
advertisement

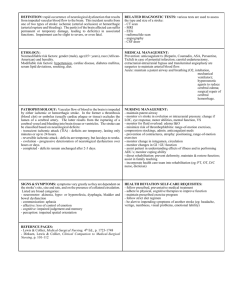
Nur-224 Identify the various types/causes of seizures. Identify clinical manifestations for clients experiencing neurologic deficits. Apply the principles of nursing management to care for the patient in the acute stage of ischemic stroke. Use the nursing process as a framework to develop a plan of care for the client with neurological deficits. 3rd leading cause of death in the US 800,000 people experience a stroke each year An emergency condition in which neurologic deficits result from a sudden decrease in blood flow to a localized area of the brain. Major loss of blood supply to the brain severe disability or death Types of stroke Ischemic (80–85%) Hemorrhagic (15–20%) Risk Factors Hypertension Sickle cell anemia Atrial fibrillation Diabetes mellitus Smoking Hyperlipidemia Obesity Sedentary lifestyle TIA or “little stroke” Characterized by a gradual/rapid onset of neurologic deficits compromised cerebral blood flow Stroke leads to a loss/impairment of sensorimotor functions on the opposite side the side of the brain that is damaged contralateral deficit. Stroke in the (R) hemisphere of the brain is manifested by deficits in the (L) side of the body (and vice versa) Disruption of the blood supply to the brain due to an obstruction a thrombus or embolism, or from stenosis of a vessel resulting from a buildup of plaque Types Large vessel stroke Small vessel stroke Cardiogenic embolism Symptoms depend upon the location and size of the affected area Numbness or weakness of face, arm, or leg, especially on one side Confusion or change in mental status Trouble speaking or understanding speech Difficulty in walking, dizziness, or loss of balance or coordination Sudden, severe headache Perceptual disturbances Paralysis/weakness on (R ) side of the body (R ) visual field deficit Aphasia Altered intellectual ability L sided stroke Paralysis/weakness on the (L) side of the body (L) visual field deficit Impulsive behavior and poor judgment Lack of awareness of deficits R sided stroke Sensoriperceptual deficits Cognitive and behavioral changes Communication disorders Motor deficits Elimination disorders Deficits may include Hemianopia Apraxia Neglect syndrome Cognitive changes Behavioral changes Emotional lability Loss of self-control Intellectual changes Usually a result of the stroke affecting the dominant hemisphere Aphasia Expressive Receptive Global Depending on the area of the brain involved strokes may cause: Hemiplegia Hemiparesis Flaccidity Spasticity Bladder elimination Bowel elimination Mini-stroke Brief period of localized cerebral ischemia that causes neurologic deficit lasting less than 24 hours Sudden loss of motor, sensory, or visual function Serves as a warning for impending stroke Acute phase diagnosis the type/cause of the stroke support cerebral circulation control/prevent further deficits Focus minimize brain injury maximize patient recovery Complete history/careful physical assessment CT scan DWI test PLAC tests Prevention Antiplatelet- Aspirin, clopidogrel(Plavix), ticlopidine(Ticlid) Acute Stroke fibrinolytic therapy-tissue plasminogen activator anticoagulant therapy Antihypertensive medications Used to treat ischemic stroke by dissolving the blood clot that is blocking blood flow to the brain. Recombinant t-PA Rapid diagnosis of a stroke and initiation of therapy (within 3 hours) decrease the size of the stroke and may improve functional abilities after 3 months Bleeding most common side effect Surgery (Carotid Endarectomy) Performed to prevent the occurrence of a stroke Restore blood flow when a stroke has occurred Repair vascular damage Rehabilitation Physical therapy Occupational therapy Speech therapy Position on the inoperative side – Assess respirations/oxygen saturation - hemorrhage -respiratory distress - cranial nerve impairment -hypotension/hypertension Stroke prevention – esp known risk factors Public awareness of signs of TIA/Stroke Sudden – - weakness/numbness - confusion, trouble speaking - trouble walking, dizziness, loss of balance - trouble with vision - severe headache without a cause Risk for Ineffective Tissue Perfusion- Cerebral Impaired Verbal Communication Impaired Swallowing Impaired Physical Mobility Self-care deficits r/t (bathing, grooming, hygiene) Maintain correct position good body alignment avoid deformities Change position every 2 hours – if sensation is impaired on one side – the amount of time spent on the affected should be limited. Prevent pressure ulcers. Affected extremities – ROM exercises Prepare for ambulation ASAP/active rehabilitation program May swallowing problems (dysphagia). Swallowing difficulties place the patient at the risk for aspiration, pneumonia, dehydration, and malnutrition. Start patient on thick liquid/pureed foods easy to swallow Patient unable to consume oral intake enteral feedings Long-termed feedings gastrostomy tube Aphasia –receptive/expressive Face the patient and establish eye contact Develop strategies to make the atmosphere conducive to communication Speak in a normal manner and tone, speak slowly Use gestures, pictures, objects, writing, Use same words and gestures be consistent At risk for skin and tissue breakdown Specialty bed Regular turning schedule Minimize shear/friction forces Recovery/rehabilitation may be prolonged and requires patience. Community based support groups Depression – common /serious problem Caregivers need to be reminder to attend their own health concerns/well-being respite care. Intracranial hemorrhage Cerebral blood vessel ruptures. May be due to: Intracerebral hemorrhage Intracranial aneurysm AV malformation Subarachnoid hemorrhage Similar to ischemic stroke Severe headache Early and sudden changes in LOC Vomiting Maintain optimum tissue perfusion -aneurysm precautions Manage potential complications - vasospasms - hyponatremia - seizures Promote home and community-based care A single event of abnormal, sudden, electrical discharge in the brain resulting in an abrupt and temporary altered state of cerebral function. Epilepsy (seizure disorder) – - chronic disorder of abnormal, recurring excessive electrical discharges - recurring seizures accompanied by some type of behavioral change affect more than 3 million people strong genetic component Precipitating factors birth defects head injury/trauma metabolic disorders/renal failure hyponatremia, IICP The cause is unknown in 70% of all cases All people with epilepsy have seizures, but not all people who have a seizure have epilepsy. Only after a person has two seizures dx. of epilepsy is made Classification of seizures Partial seizures: begin in one part of the brain Generalized seizures: involve both hemispheres of the brain Messages from the body are carried by the neurons (nerve cells) by electrical discharges. Impulses occur when a nerve cell has a task to perform. Sometimes there is an excessive imbalance and the cell continues to fire after the task is completed. Unwanted discharges cause the body to respond erratically. Consciousness is always impaired Absence seizures (petit mal) -sudden brief cessation of all motor activity accompanied by a blank stare and unresponsiveness. Tonic-clonic seizures (grand mal) - common type of seizures in adults - warning aura may precede generalized seizure activity Tonic Phase Begins with a sudden loss of consciousness, sharp muscle contractions Patient may fall to the floor Urinary incontinence is common Breathing ceases and cyanosis develops Pupils are fixed and dilated Tonic phase may lasts – 15 seconds – 1 minute Clonic Phase Alternating contraction/relaxation of the muscles in all extremities Eyes roll back and the patient froths at the mouth Phase varies in duration and subsides gradually Entire seizure generally lasts no more than 60-90 seconds Following clonic phase (postictal phase) Person remains unconscious /unresponsive to stimuli Person is relaxed and breathes quietly Regains consciousness gradually May be confused/disoriented Headache muscle ache and fatigue may follow Amnesia of the seizure may follow Because of lack of warning with tonic-clonic seizures, head injury, fractures, burns may occur secondary to seizure activity Can develop during seizure activity Seizure becomes continuous– with only short periods of calm between intense and persistent seizures Cumulative effect muscular contractions that interfere with respirations Hypoxia, acidosis, hypoglycemia, hyperthermia and exhaustion may occur if the convulsive activity is not stoped. medical emergency Goal – stop the seizure (ASAP) Establish and maintain airway is priority Diagnostic Assessment Confirm the diagnosis, determine any treatable causes and precipitating factors Diagnostic Testing MRI/CT Scan EEG Lab data – CBC, biochemistry Pharmacologic therapy ( AEDs) controls rather than cures seizures Medication blood levels should be monitored Antiseizure drugs should not be discontinued abruptly because it can precipitate seizures Protect the patient from harm, reduce/ prevent seizures activity without impairing cognitive function or producing undesirable side effects Phenytoin (Dilantin) Caramazepine ( Tegretol) Gabapentin (Neurotonin) Topiramate (Topamax) Valproate (Depakote,Depakene) Clonazepam (Klonopin) see page 1885 Note CNS side effects: blurred vision, slurred speech, confusion Patients on prolonged therapy may need a diet rich in Vitamin D Maintain good oral hygiene – phenytoin Obtain liver functions Carry identification indicating type of seizure -- being treated for Nursing Diagnosis Risk for Ineffective Airway Clearance Anxiety Risk for injury r/t seizure activity Readiness for Enhanced Knowledge Describe the mechanisms of injury, clinical manifestations, diagnostic testing, and treatment options for patients with brain and spinal cord injuries. Use the nursing process as a framework for care of clients with brain and spinal cord injury Involves damage to the neural elements of the spinal cord. Both sensory and motor function are often involved. Major causes contusion, compression, laceration, hemorrhage and damage to the blood vessels in the spinal cord. A major health problem 200,000 persons in the U.S. live with disability from SCI Injuries due to: MVAs, falls, acts of violence, and sports injuries Males account for 82% of SCIs Young people ages 16–30 account for more than half of all new SCIs African–Americans are at higher risk Risk factors include alcohol and drug use Spinal cord provides a two–way pathway for the conduction of impulses and information to and from the brain and the body Ascending (sensory) pathways carry information pain, temperature, touch, Descending (motor) pathways carry information about movement Involve damage to the vertebrae and supporting ligaments as well as the spinal cord. Are the result of excessive force to the spinal column. Most common causes -> acceleration and deceleration Acceleration: external force is applied in a rear end collision Deceleration: occurs in a head on collision Vertebrae frequently Involved 1st, 2nd, and 4th to the 6th cervical vertebra. The 11 thoracic to 2nd lumbar vertebra. Is determined by the amount of cord involvement Paraplegia Quadriplegia The patient requires emergency assessment and care and medications. Initial care immobilization and extrication/stabilization of injuries. And possible surgery. SCI affects every body system and function. When injury is C1 to C4 respiratory paralysis is common and ventilator assistance is required Neurological examination Diagnostic x-rays ( cervical spine) CT /MRI ABG’s Trauma Screen Fluids Medications – corticosteroids, vasopressors, antispasmodics, NSAIDs, PPI, anticoagulants Temporary loss of reflex function (areflexia) below the level of injury at the cervical and upper thoracic spinal cord. As a result –SNS is interrupted and the PSNS is unopposed. Muscles become completely paralyzed and flaccid/reflexes are absent Loss of urinary bladder tone, intestinal peristalsis, perspiration Recovery from spinal shock is gradual – usually 4-6 weeks. Exaggerated sympathetic response affects persons with SCI at or above the T6 level. Caused by visceral distention from distended bladder/impacted rectum Pounding headache, hypertension, profuse sweating, bradycardia, piloerection (goosebumps) HOB – high fowler’s, loosen tight clothing Asses bladder distention -catherization Fecal impaction – disimpact immediately Surgery – done to stabilize and support the spine Stabilization/Immobilization – a type of traction or external fixation device to stabilize the vertebral column and prevent further damage to the cord. Impaired Gas Exchange Impaired Physical Mobility Impaired Urinary Elimination and Constipation Sexual Dysfunction Long-term care rehabilitation is needed Learn strategies necessary to cope with their alterations that the injury imposed on ADL’s Care for the patient involves members of all health care disciplines Psychologic support Goal of rehabilitation independence Herniated intervertebral disk ( ruptured disc, slipped disk) is a rupture of the cartilage surrounding the intervertebral disk with protusion of the nucleus pulposus. Most common cause of low back pain . May affect 2/3 of people at some point in their lifetime. Most back problems are related to disk disease More common in men than women Most patient are between the ages of 30-50 Majority of herniated disks occur in the lumbar region (L4 or L5 to S1), when disk herniate in the cervical region, they occur most often in the C6-C7 region Herniation may be abrupt or gradual Intervertebral disk is a cartilaginous plate that forms a cushion between the vertebral bodies Herniation of the intervertebral disk, causes the nucleus of the disk to protrude into the fibrous ring around the disk. Immediate symptoms are short-lived, and those resulting from injury to the disk do not appear for months or years. Continuous pressure may cause degenerative changes in the involved area Lumbar Disk recurrent episodes of lower back pain pain radiates across the buttocks and down the posterior leg (sciatica) Cervical Disk (C5-C6, C6-C7) Most herniations are the result of degeneration pain and stiffness neck, shoulders, arms pain dull, intermittent pain parethesia of upper extremities Diagnostic findings MRI CT scan EMG Neurologic examination Herniations of the cervical and lumbar disks are most common and are treated conservatively unless the patient is experiencing severe neurologic deficits. Conservative Treatment Bedrest (no longer recommended) Patient is advised to continue with normal activities while taking medication for pain, inflammation, and muscle spasms. NSAID – ibuprofen (Motrin, Advil), naproxen (Naprosyn) Muscle relaxants – cycobenzaprine (Flexeril), methocarbamol (Robaxin) Hot moist compresses Surgery is sometimes necessary Significant neurological deficit Continuing pain or sciatica Loss of sensory /motor function Laminectomy-done to relieve the pressure on the nerves Spinal fusion- insertion of a wedge-shaped piece of bone or bone chips between the vertebrae to stabilize them. Craniotomy: opening of the skull Purposes: remove tumor, relieve elevated ICP, evacuate a blood clot, control hemorrhage Craniectomy: excision of portion of skill Cranioplasty: repair of cranial defect using a plastic or metal plate Burr holes: circular openings for exploration or diagnosis, to provide access to ventricles or for shunting procedures, to aspirate a hematoma or abscess, or to make a bone flap Preoperative diagnostic procedures may include CT scan, MRI, angiography, or transcranial Doppler flow studies Medications are usually given to reduce risk of seizures Corticosteroids, fluid restriction, hyperosmotic agent (mannitol), and diuretics may be used to reduce cerebral edema Antibiotics may be administered to reduce potential infection Diazepam may be used to alleviate anxiety Obtain baseline neurologic assessment Assess patient and family understanding of and preparation for surgery. Provide information, reassurance, and support Postoperative care is aimed at detecting and reducing cerebral edema relieving pain preventing seizures, monitor ICP The patient may be intubated and have arterial and central venous lines. frequent monitoring of respiratory function including ABGs monitor VS and LOC; noting any potential signs of increasing ICP assess dressing and check for evidence of bleeding or CSF drainage monitor for seizures; if seizures occur, carefully record and report these monitor fluid status and laboratory data Risk for imbalanced body temperature r/t damage to hypothalamus Disturbed sensory perception r/t periorbital edema, head dressing Body image disturbance r/t change in appearance or physical disabilities Impaired communication (aphasia) r/t injury to brain tissue Strategies to control factors that increase ICP Avoid extreme head rotation Head of bed may be flat or elevated 30° Suction or encourage coughing cautiously as needed (suctioning and coughing increase ICP). Humidification of oxygen may help loosen secretions. Sensory deprivation Periorbital edema may impair vision, announce presence to avoid startling the patient; cool compresses over eyes and elevation of HOB may be used to reduce edema if not contraindicated. Enhancing self-image Encourage verbalization. Encourage social interaction and social support. Attention to grooming. Cover head with turban and, later, a wig. What to expect after surgery medication is taken appropriately rehab – depending on post-op level of function physical therapy – residual weakness/mobility occupational therapy – self care concerns speech therapy – aphasic If prognosis is poor – discuss end of life preferences