Board of directors minutes June 2014 538.4 KB
advertisement

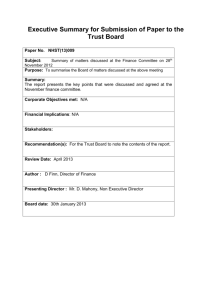
85th Meeting of the Board of Directors Thursday 5 June 2014 Room 4, Memorial Hospital Board of Directors Dave Mellish Archie Herron Anne Taylor James Kellock Seyi Clement Steve James Paul Ward Stephen Firn Helen Smith Ify Okocha Wilf Bardsley Ben Travis Simon Hart Chair Vice Chair and Non-Executive Director Non-executive Director Non-executive Director Non-executive Director Non-executive Director Non-executive Director Chief Executive Deputy Chief Executive and Director of Service Delivery Medical Director Director of Nursing and Governance Director of Finance Director of HR and Organisational Development In attendance Ann Rozier Susan Owen Trust Secretary and Head of Governance Risk Manager (Minutes) Members of the Council of Governors in attendance Chris Purnell Service User/Carer Governor, Working Age Adult Mental Health John Woolgrove Public Governor, Bromley Judy Wolfram Public Governor, Greenwich Action 1 Apologies for absence None. Noted 2 Minutes of the Board of Directors meeting 3rd April 2014 and Extraordinary Meeting 1st May 2014 Page 1 – Michael Witney was in attendance at the meeting on 3 April 2014 Page 2 – Amend the first sentence of item 6 to read: The Trust took on the management of the Children and Young Peoples Ambulatory Unit at the QMH site on 1 April 2014, for an interim period, pending the outcome of the tender. Pending these amendments, the minutes of the Board of Directors meeting on 3rd April 2014 were approved as an accurate record. The minutes of the Extraordinary Meeting of the Board of Directors meeting on 1st May 2014 were approved as an accurate record. Approved 3 Matters arising Page 5 – The Trust was not successful with the bid for the Urgent Care Centre. The contract has been awarded to the Hurley Group. Transfer will take place on 1 July 2014. Staff will retain NHS terms and conditions. Page 5 – The Liaison and Diversion Service has been awarded funding to expand in Bexley, Bromley and Greenwich. Investment for the ALD dementia care worker been withdrawn. The directorate is considering alternative options to address this. Noted 4 Key Performance Indicators Report All Monitor targets have been achieved. Attendance at the Urgent Care Centre remains high and all patients were seen within four hours. Psychological Therapies waiting times continue to improve steadily. In in-patient services, there have been few UEAs but sleepover activity remains Noted Page 1 of 9 Action high. Occupancy is low at Atlas House but we are continuing negations with Bromley and Croydon CCGs. A marketing plan is being developed. Recording of ethnicity and unoutcomed appointments is improving. Patients with an estimated discharge date has improved on the Stepup, Step-down Unit but has decreased on the Bevan Unit. DM – Can we access data on UCC performance after this has transferred to the Hurley Group? HS – There is not much information in the public domain. PW – How engaged are the Commissioners in terms of in-patient activity in working age adults? HS – Greenwich are very involved. Much of the pressure is managed through the Home Treatment Team. Bromley CCG have purchased less beds. SC – Why are CAMHS not meeting the target for clients on a CPA caseload receiving a review within six months? SF – CAMHS have a clear focus on providing care to children and families. There are no safety or quality concerns but clinicians are not always sighted on targets. HS – There is some work to do to ensure that clinicians engage with data processes. 5 Service Delivery Report The Bexley MSK Service is performing well. Activity levels have been sustained and both legacy and new patients are being triaged and treated. Waiting times have reduced and the conversion rate has improved from 25% to 60%. Lorraine Regan has been appointed as Clinical Director for the Adult Mental Health and ALD Directorate. She will be supported by three Assistant Clinical Directors; Dr Derek Tracy (inpatient and crisis services), Jane Harris (community mental health services) and Sandra Baum (ALD services). Bromley CLDT are embarking on development work to become an integrated health and social care team, with support from the Institute of Public Care. AH – With regard to the Healthy Weight programme, we need to be careful about how concerns are communicated to parents and children. There has been some negative media coverage about the way in which providers have done this. JK – Is the number of changes in clinical directors a positive move? IO – The changes will enable clinical directors to focus on improving quality and developing our relationship with GPs. SC – What services will be affected by the Supreme Court ruling on the Mental Capacity Act and Deprivation of Liberty safeguards? IO – This will affect dementia patients, those with functional mental health needs and also the work of Approved Mental Health Professionals (AMHPs). The impact on work is substantial. SC – How will we address this? IO – We will need to have focus on ensuring that clinicians test capacity and understanding and monitoring that this is documented. PW – How are we approaching the HMP Belmarsh bid? HS – The Forensic Directorate are very focused on this and a structure is being developed. PW – Are there any re-design issues? HS – We are not sure of the detail at this stage. AH – We will need to ensure that there is an adequate balance between price and quality. Noted 6 Audit Committee and Procurement Update KPMG have introduced a RAG rating scale to replace the one used last year. The audit on NED succession planning arrangement received an opinion of Green. The HR and payroll audit made recommendations to streamline processes. Counter-fraud services have been assessed as adequate and sufficient. The Annual Report and Accounts and Quality Accounts for 2013/14 have been approved. Procurement update There is a national focus on reducing procurement costs. A rationalised pricing list is being developed. It is projected that there will be a core list of 1000 items by September 2014 with 5000 items by 2015. The Trust has established a Strategic Procurement Group. Noted 7 Governance Board update The Corporate Risk Register has been updated to reflect the strategic priorities in the two-year Operational Plan. There are five new risks and nine carried over from the 2013-14 risk register. The new risks include one significant (4 x 4 = 16) risk escalated from the Children and Young Noted Page 2 of 9 Action Person’s Directorate. This relates to defending the Greenwich CAMHS contract, which is due to be re-tendered by October 2014. This has been rated as significant as this is a strategically important contract for the Trust and there are a number of credible competitors. A directorate Re-tender Project Group has been established to ensure that there this is a high level of focus on preparing the bid. The Directorate has been asked to ensure that there is clinical leadership. DM – We know we have a high quality service; much work will be needed to ensure that we can defend this. AT – What is the position with the Bexley CAMHS tender? SF – Bexley CCG intend to re-tender all children’s services using a prime contractor model. Regulatory update The Governance Board received an update on the CQC’s new approach to regulating, inspecting and rating services, to be rolled out from October 2014. The Trust’s Peer Review programme has been remodelled to ensure that services are preparing for the new regime. 8 Crisis Care Concordat – Trust position The Mental Health Partnership Board working group is overseeing implementation of the Crisis Care Concordat action plan. We have increased our focus on monitoring the use of s136. PW – How much will this cost and what are the priorities? WB – This will be taken forward within existing resources. Areas that require partnership working will need greater consideration. DM – We will need detailed information on s136. This will put additional pressure on services. 9 Quality Report Noted QSIP – April 2014 The number of QSIP indicators has reduced from 27 to 23. Pressure ulcer information is provided in a separate report. The RAG rating thresholds have been changed so that red is greater than 6% from the target and Amber is less than 5% from the target. The two red indicators are: Consent to treatment (S58): There was one patient out of 18 where consent could not be located in the records. This has since been addressed. Completion of one year checks by 14 months: The April position is under target by 27.3% (357 out of 527). High risk children are being targeted. The five amber indicators are: Carer details recorded on RiO – under target by 4.1%. 48 hour follow up for patients admitted following self-harm/suicide attempt – one patient out of 33 was not seen within 48 hours. This has since been addressed. Patients detained provided with information (S132) – there were three CTO patients where evidence of discussion could not be found. Care plans on RiO for community teams – under target by 4%. Care plans on RiO for District Nursing teams - under target by 5%. Pressure ulcers – April 2014 There were 22 pressure ulcers in 21 people. Two Grade 3 pressure ulcers have been classified as avoidable. One patient was on a palliative care pathway and the second did not follow advice. SJ – Is there a consequence to missing the consent to treatment target? IO – I write to the consultant and monitor performance. JK – At what point would a doctor be referred to the GMC? IO – If the error were made consistently. Clinical Effectiveness Group Care Planning and Engagement: A good start has been made. There is clarity on the objectives of the project but a change of culture is required. Clinical Audit: A new NICE repository has been made available. From July 2014, DatixWeb will be used to track action plans from audits. Outcome measures: The CEG has agreed four measures which will be piloted in Crisis and Home Treatment Teams. These are patient reported outcome measures; patient reported experience measures, clinically reported outcome measures and functioning. JK – Will there be measures for non-mental health teams? IO – We will learn lessons from the pilot indicators. Page 3 of 9 Noted Action DM – NED involvement on the Quality Board is to be increased. PW and SJ will attend the Quality Board and SC will continue to attend the CEG. 10 Compliance Report Mental Health Act visits Since the last report to the Board, the Trust has received six new reports from recent CQC Mental Health Act Commissioners visits. Key themes are access to and completion of T2 and T3 documentation, Care planning and discharge planning. In relation to Heath Ward, the Seclusion Policy does allow for use of a seclusion gown to maintain patient safety as a last resort but this is to be reviewed. Seclusion gowns will not be used whilst this review is taking place. CQC concerns raised There have been two enquires from the CQC, both of which are being followed up. One relates to the care of a patient on Camden Ward and the other to a medication incident at North House. MHA data The use of s136 is increasing, both in terms of numbers and as a percentage of all sections. Patient Safety The Central Alerting System have issued two patient safety alerts, with a number of high level actions due for completion by 19 September 2014. The Director of Nursing will be the Board level lead for medical devices and the Medical Director the Board level lead for medicines error reporting. Ten serious incidents were reported in April 2014. The current Level 5 homicide inquiry will be report to the Board in July. The independent inquiry into the homicide committed by NE has been delayed. The latest NRLS Organisation Patient Safety Incident Report shows that the Trust is now the second highest reporter of all trusts in the same cluster. We are an outlier in the “infrastructure” category, due to the high level of reporting sleepovers. The criteria for reporting these are to be reviewed. Complaints Clinical care remains the most frequently raised complaints issue. There were no new referrals to the Ombudsman in March and April 2014. Ten cases were referred in 2013/14 and eight of these were not upheld. Of the two upheld cases, one related to the Step-up, Step-down Unit and the second the Greenwich District Nursing Service. SJ – How often is seclusion used and why? SF – Burgess Clinic and Heath Clinic are the only wards that have a seclusion suite. WB – Use of seclusion is not routine. It would only be used to ensure patient safety when managing highly disturbed behaviour. All incidences of seclusion are clinically reviewed. SC – Is ‘time out’ an issue? AR – This has been checked and we have found that people understand that ‘time out’ is de facto seclusion and must not be used. DM – We need to do further work on ensuring there is access to activities at the weekends. This to be on the agenda for the Board of Directors meeting in September 2014. AT – Some of the serious incidents clearly occurred in the patient’s home, but others are not clear. WB – This will be made clearer for future reports. DM – The report should also include a comment on why it is a Level 4 as opposed to a Level 5. SF – The judgment is based on whether there has been a significant failing or there is likely to be significant public interest. PW – Does the increase in sections indicate an increase in risk level? WB – It is a reflection of higher levels of occupancy and demand. IO – There is a higher level of acuity on our wards. Monitoring incidents on the wards is one way of measuring this. DM – In the future, a full complaints report is to be presented when Michael Witney attends to present the Patient Experience Report. In the intervening meetings, report by exception only. Noted 11 Carers Survey The Trust commissioned the Carers Survey in October 2013. The survey was sent to 1000 carers of whom 400 responded. The report was published in February 2014. The results show that we need to make improvements in providing support to carers and sharing information. An action plan has been developed and directorates have been asked to respond to areas of concern. Noted Page 4 of 9 WB/IO WB WB/MW Action National Carers week is 9 to 15 June 2014 and the Trust is working to partners to run events in each borough. AH – Half the respondents said that they did not have or were not sure if they had a care plan. It needs to be clearly communicated that the Standard CPA Care Plan is in the form of a letter. AT – Why is the Friends and Family Test score zero? WB – The methodology used only counts the most positive score. SJ – Are these results a consequence of the increase in demand? WB – This is a cultural issue. There needs to be more focus on carers. DM – An update on progress is to be included in the quarterly patient experience report. WB/MW 12 Business Committee update Noted There are two bids in progress; Bromley Older Peoples Services and Bromley Community Wellbeing Service for Children and Young People. The Committee noted the strategic importance of growing our presence in Bromley. The Committee noted the new Trust Communications Strategy. The Business Committee agreed a proposal to strengthen oversight of the Trust’s charitable funds. The Business Committee will act as a sub-committee to the Trustees and will receive a detailed report every six months prior to a formal report being presented to the Trustees. A letter setting out the proposals for mental health bed reconfiguration will be sent to the Council of Governors in advance of the June meeting. The contract for the refurbishment of Reeves and Chislehurst wards at Queen Mary’s Hospital is currently being tendered. The Business Committee approved that the contract for mattress and pressure relieving equipment is awarded to Westmeria. Open RiO has been selected as the new clinical system to replace the current version of RiO by October 2015. A saving of £1.0m has been negotiated. 13 NED report – Board visits DM – Bromley Home Treatment Team: Staff raised some concerns about transfers to the Short Term Intervention Team and the allocation of Care Co-ordinators. The s136 suite is in need of improvements. Avery Ward: An impressive amount of work around physical health. Staff said that having a consultant on the ward was valuable. Some concerns about parking were raised. Bexley Home Treatment Team: There is a reduced demand for beds. PW – Shenton School: There is an increase in demand. Staff commented that they are not always able to influence decisions. There was a high level of satisfaction with the service. QMS paediatric service: The integration work is paying dividends. AT – Older Persons Community Team: Staff commented that they would like more clinical space. Completing panel paperwork requires a MDT approach. Estelle Frost to raise this with the LA. AH – Greenwich Community Learning Disability Team: Integration works well. Positive feedback was given. SJ – The Source: This is small team which is highly valued by the community it serves but does appear to be vulnerable. SC – HMPs Blantyre, Sutton Park, Maidstone and Elmley: The teams work well in a difficult environment. Increased use of ‘lockdown’ by prison staff means that it is more difficult for the teams to gain access to patients. The triage and reception arrangements for new prisoners could be improved. There is no access to RiO. Some concerns about the safety of staff were raised. JK – Bromley Recovery East: This is a strong team dealing with a complex patient group. Staff were mainly positive. Bexley Recovery: Demand is increasing. Staff were critical of primary care. Two patients spoken to complemented the team. Action points will be picked up by the directorate. 14 Council of Governors update The next meeting will be held on 19 June 2014. The main items are the Nominations Committee and NED succession planning. The process for appointing the Chair will commence in June 2014. The new appointee will shadow the current Chair for four months and will be involved in the appointment of two non-executive directors. It has been proposed that the Constitution should be changed to allow candidates from beyond Bexley, Bromley and Greenwich to apply. Noted 15 Finance Report As at the end of Month 1, the Trust delivered a surplus of £0.2m which is £0.1m higher than plan. Noted Page 5 of 9 Action Under the new Monitor Risk Assessment Framework, the Trust scored 4 (no evident concerns) which is in line with plan. Bank and agency spend is increasing. Some of this is due to the mobilisation of new services, but this trend will be kept under review. Overall debt levels are £9.5m but debts of over 90 days have decreased to £1m. The Memorial fraud trial is due to commence on 14 July 2014. This is estimated to last for four to six weeks and some publicity is expected. Support has been provided for staff called as witnesses. 16 Safe Staffing Report Noted This is the first formal report to the Board. Whilst there is some further work to do, the overall conclusion is that staffing levels are safe. In-patient nursing data for May must be uploaded to the Unify system by 10 June 2014. Data for this has been collated manually using the information displayed on ward noticeboards. Establishments are being reviewed. There is no validated tool for mental health services, but ratios of between 1:5 and 1:8 have been recommended by NICE and the RCN. The financial ledger, Health Roster and ESR have been used to generate establishment data. There are some discrepancies with the baseline data which need to be resolved. There are super-numerary roles in some services and we will need to consider how this is captured. The Safe Staffing Group has recommended the percentage adjustments to take account of headroom, is allowance for sickness absence and leave. The following recommendations have been made by the Safe Staffing Group:1. Agree escalation process to ensure availability of nursing staff when required. 2. Review the Health Roster wards templates to ensure accurate reflection of shift requirements. 3. Consider augmenting the functionality of Health Roster to support capacity planning and monthly reporting. 4. Review vacancies across all directorates and agree recruitment. 5. Agree headroom allowances and apply to establishments. 6. Further review utilisation of temporary staffing; absence and sickness management. 7. To reconcile discrepancies between Finance/ESR and Health Roster. 8. To pilot the use of Professional Judgement model when guidance becomes available to conduct an establishment review in bed based services. JK – Are there cost implications? SH – Yes. There are some areas where is it difficult to recruit HCAs. PW – We need to model the financial consequences. WB – Temporary staff are being used to cover vacancies, sickness absence and high levels of acuity. Where acuity is a regular reason for needing additional staff, we will need to review the establishment. AR – Have NHS Choices given any guidance on how the data will be rated? WB – They will note trusts that do not contribute. NHS England will also check. This is being linked to the ‘Sign up to Safety’ initiative dashboard. SH – Vacancies are actively being recruited to and are not being held to save costs. 17 Workforce Report Sickness absence in April 2014 was 4.58%, an increase from the March figure of 4.43%. The majority of this is long term absence. Vacancy rates are 10.34% but there is variation across directorates. Adult Community Services has an overall vacancy rate of 19% with significant vacancy rates for qualified nursing staff and AHPs. The overall number of recruitment campaigns stands at 349. The average time from requisition to start date is 16.6 weeks and ways to reduce this further are being considered. There was a positive response to the recent marketing campaign but there was less interest from AHPs. PDR completion stands at 84%. All mandatory and essential skills training is above 80% with the exception of patient handling. There are 13 live disciplinary cases. There are four members of staff suspended from duty and three tribunal claims against the Trust. There have been fewer dismissals compared to last year. A full equality impact assessment is undertaken annually. The new Supervision Policy has been launched. All staff must receive a 1:1 supervision session every six to eight weeks and record this on NHS Learn. A trajectory approach will be used to monitor this. An update on supervision will be brought to the next Board. IO – Clinicians have expressed concerns about how supervision documentation will be used. Page 6 of 9 Noted SH Action SH – The onus is on managers to document actions to address performance concerns. Both parties are able to review the record. SJ – How many new staff have we recruited from the recent marketing campaign? SH – It is too soon to say. SJ – Why is there so much recruitment activity? SH – Some are re-advertisements and some are related to mobilisation for new contracts. 18 5 Year Strategic Plan Agreed The Trust has a three year Service Development Strategy and a two year operational plan. The five year strategic plan will focus on the final three years from 2016/17 to 2018/19. Monitor have asked all FTs to review their assumptions in the two year operational plan. The Trust is recommending that our plans are realistic and are forecasting a break even by year five. The Plan must be submitted to Monitor by 30 June 2014. The Board of Directors was asked to agree that final approval is delegated to the Business Committee meeting on 17 June 2014. AH – Some trusts are considering moving away from Agenda for Change terms, is this something Oxleas would consider? PW – This would have to be balanced against paying the market rate. SF – The issues and options will be discussed at a future Informal Board meeting. Representatives of the Council of Governors will be invited to attend. AH – We need to consider how we can use our properties to expand the scope of our activities. DM – We are certain about the next two years. We need to be conservative and explore all possibilities before considering changes to terms and conditions. Agreed: The Board of Directors agreed that final approval is delegated to the Business Committee. 19 Chief Executive Update The Trust has been invited by NHS England to be one of the twelve ‘trailblazer’ organisations in the Sign Up to Safety campaign. A launch event will be held on 24 June 2014. The Director of Nursing and Head of Patient Safety attended an introductory workshop on 29 May 2014. We have been asked to respond to make five pledges, respond to six key questions and develop our own implementation plan. The responses to the six questions will be circulated to the Board and agreed by SF and JK. An update will be brought to the July Board meeting. Noted 20 Any Other Business None raised Noted 19 Written questions from the public Noted Will the new version of RiO have the functionality to record an alert for those deemed to be at high risk of suicide? WB – This has been included in the specification for Open RiO. Next meeting of the Board of Directors Thursday 3rd July 2014 Room 4, Memorial Hospital I confirm that the minutes of the Board of Directors meeting of 5th June 2014 are a true record Signed Dave Mellish, Chair Date: Page 7 of 9 WB Jargon buster This jargon buster is a glossary of acronyms and abbreviations. It is intended that we will update this on a regular basis but we will also agree standards to reduce jargon usage. If you feel there are more that should be included on the list please email anne.rozier@oxleas.nhs.uk ACS – Adult Community Services DN – District Nurse CDM – Chronic Disease Management DNA – Did Not Attend ADHD – Attention Deficit Hyperactivity Disorder CEG – Clinical Effectiveness Group ECR – Electronic Care Records ADL – Assessments of Daily Living or Activities of Daily Living CIP – Cost Improvement Programme ECT – Electro Convulsive Therapy IMHER – Integrated Mental Health Electronic Record IM&T – Information Management and Technology EI – Early Implementer ISA – Information Sharing Agreement ESR – Electronic Staff Records KPI – Key Performance Indicators ETP – Electronic Transfer of Prescriptions KSF – Knowledge and Skills Framework LAS – London Ambulance Service CPC – Cost Per Case FCPN – Forensic Community Psychiatric Nurse FOI – Freedom of Information CPN – Community Psychiatric Nurse HCA – Health Care Assistant LGBT – Lesbian, Gay, Bisexual, and Transgender CRB – Criminal Records Bureau HEE – Health Education England LHC – Local Health Community ASBO – Anti-Social Behaviour Order CRE – Cash Releasing Efficiency HID – Hospital Integrated Discharge Team LSP – Local Service Provider ASD – Autistic Spectrum Disorder CRHTT – Crisis and Home Treatment Team ASW – Approved Social Worker C&YPS – Children and Young People’s Service BMs – Business Managers AfC – Agenda for Change AHP – Allied Health Professional ALBs – Arms Lengths Bodies ALD – Adult Learning Disabilities AMH – Adult Mental Health AMHP – Approved Mental Health Professional CLDT – Community Learning Disability Team CNST – Clinical Negligence Scheme Trust CPA – Care Programme Approach HIMP – Her Majesty’s Inspectorate of Prisons LD – Learning Disability LTC – Long Term Condition HR – Human Resources MAPP – Multi Agency Protection Panel CQC – Care Quality Commission HTT – Home Treatment Team MCA – Mental Capacity Act CAMHS – Child and Adolescent Mental Health Services CQUIN – Commissioning for quality and innovation HV – Health Visitor MDA – Multi-disciplinary Assessment CAPA – Choice and Partnership approach (a new way of managing referrals into CAMHS) DADL – Domestic Activities of Daily Living CAS – Central Alerts System CBT – Cognitive Behavioural Therapy CCG – Clinical Commissioning Group DESMOND – Diabetes education and self management programme for ongoing and newly diagnosed DH – Department of Health ICP – Integrated Care Pathway ICT – Information Communication Technology MDO – Mentally disordered offender MDT – Multidisciplinary team iFox – Trust Business Information System MEWS – Modified Early Warning Score Tool IGG – Information Governance Group MH – Mental Health IGT – Information Governance Toolkit Page 8 of 9 MHA – Mental Health Act MH MDS – Mental Health Minimum Dataset MHRA – Medicines Healthcare and products Regulatory Agency PEG – Patient Experience Group PD – Personality Disorder PDR– Personal Development Review MSK – Musculo-skeletal Services PDS – Patient Demographic Service (national repository holding demographic information) NCC – National Consortium of Colleges NEDs – Non Executive Directors NHSLA – NHS Litigation Authority NICHE – National Institute for Health and Care Excellence RPST – Risk Pooling Scheme Trust PDP – Personal Development Plan MHRN – Mental Health Research Network NAC – Nursing Advisory Committee RMN – Registered Mental Nurse RMO – Responsible Medical Officer SAP – Single Assessment Process SCG – Specialist Commissioning group SDS – Service Development Strategy SLaM – South London & Maudsley NHS Trust PEAT – Patient Environment Action Team SLR – Service Line Reporting PFI – Private Finance Initiative SMs – Service Managers PICU – Psychiatric Intensive Care Unit SN – School Nurse POMH – Prescribing Observatory for Mental Health NIHR - National Institute for Health Research PRUH – Princess Royal University Hospital NPSA – National Patient Safety Agency PSA – Personal Safety Awareness NSF – National Service Framework QEH – Queen Elizabeth Hospital OOHs – Out of Hours QMS – Queen Mary’s Hospital Sidcup OPD – Outpatients Department OPM – Office for Public Management OPMH – Older Peoples’ Mental Health PEEP – Personal Emergency Evacuation Plan PQQ - Pre Qualification Questionnaire PADL – Personal Activities of Daily Living PALS - Patient Advice and Liaison Service QRP – CQC Quality and Risk Profile SPD – Safety, Privacy and Dignity SUI – Serious Untoward Incidents TDA – NHS Trust Development Authority TSA – Trust Special Administrator TUPED – Transfer Under Present Employment UEAs – Uncontracted Emergency Admissions VTE – Venous thromboembolis QSIP – Quality and Safety Improvement Plan RAG – Red/Amber/Green RC – Responsible Clinician RCA – Root Cause Analysis RGN – Registered General Nurse RM – Risk Management Page 9 of 9