Differential Diagnosis of Secondary Headache
advertisement

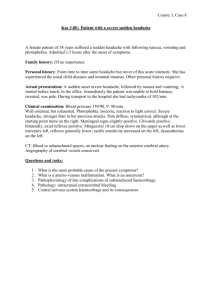
Headache Emergencies Adam Quick, MD Assistant Professor of Neurology adam.quick@osumc.edu Learning Objectives Recognize the clinical presentation and describe the acute management of subarachnoid hemorrhage. Recognize the clinical presentation and describe the acute management of meningitis/encephalitis. Recognize the clinical presentation and describe the acute management of temporal arteritis. Describe the pathophysiology, clinical presentation, differential, diagnostic considerations, and basic management of headache. Describe the pathophysiology, clinical presentation, differential, diagnostic considerations, and basic management of central nervous system infection. Describe the pathophysiology, clinical presentation, differential, diagnostic considerations, and basic management of brain tumors. Differentiate among the clinical syndromes associated with headache, and the methods of evaluation for further work up the diagnosis. Recognize acute hemorrhage and ischemic stroke on CT of the brain. Learning Resources Headache Articulate module from Part 1 Finseth Review Neurology Blueprints USMLE World Overview Basic Concepts Approach to headache Distinguishing primary from secondary headaches Patient history Physical exam Diagnostic testing Differential diagnosis of common and emergency headaches Treatment approaches to common headache scenarios Basic Concepts Headaches are an extremely common problem Most people will experience a headache of some sort during their lifetime Perhaps over 300 causes – most are benign Primary headache disorders are headache syndrome that are not caused by another medical problem – the headache syndrome IS the disorder Headache accounts for 3.3 million ER visits/year 4th most common reason adults seek care Vast majority of patients presenting to the ER with headache are going to have one of the primary headache disorders such as: Migraine Tension Cluster About 10% will have a secondary headache (these are the ones you don’t want to miss!) First purpose of history and examination is to distinguish benign recurrent or primary headaches from secondary headaches that suggest the possibility of a life-threatening event or condition Initial Evaluation Key Decision Point Primary Headache Disorder Secondary Headache Disorder History Taking Age of onset Frequency – single vs recurrent Onset, rate of progression Character of pain: pressure, stabbing, throbbing, pounding Location of pain Severity of pain Duration Additional Headache history Premonitory symptoms - auras Associated symptoms Nausea, vomiting Photophobia, phonophobia Tearing, rhinorhea Ataxia Visual disturbances Numbness, weakness, other focal neurologic symptoms Neck pain/stiffness Provocative and ameliorative measures Important medications: oral contraceptives, analgesic medications, anti-platelet agents and anticoagulants Mood or sleep disturbances Symptoms Suggestive of Primary HA Disorder Stable pattern of headache over time…even if the current headache is a little atypical Follows pattern of a defined primary headache Positive family history Most common with migraine Headache improves with sleep Headache worsened during or just prior to menses in women Normal physical and neurological examinations Headache Warning Signs First or worst headache of life Abrupt new headache symptoms or clear change in headache pattern New onset headache after age 50 Headache that disrupts sleep or is present upon awakening Headache brought on by exertion or coughing Headache with a significant positional component New headache following head trauma Signs/symptoms of systemic illness: fever, night sweats, weight loss Neck stiffness Alterations in personality, behavior or consciousness Abnormal neurologic exam Physical Exam and Headache Vital signs HEENT: assess temporal artery pulse, look for conjunctival erythema and ptosis, occipital tenderness Neck: check range of motion, tenderness, muscle spasm (remember that neck pain is present in approx. 75% of migraine patients) Neurological Exam: Extraocular movements, fundiscopic exam, facial sensation, coordination, Romberg testing Diagnostic Testing Labs that may be useful include CBC to assess for infection ESR screens for malignancy, collagen vascular disease and may help establish the diagnosis of temporal arteritis TSH may be useful in screening for thyroid disorders which may sometimes exacerbate headaches Toxicology if drug use is suspected Lumbar Puncture Crucial in several clinical situations First or worst headache of the patient’s life Headache associated with altered mental status or fever Progressively worsening headache Postural headache An atypical chronic and intractable headache Generally in a patient presenting with headache it is reasonable to get imaging (CT) prior to LP Indications for Neuroimaging Any unexplained objective abnormality on neurological exam Rapidly increasing headache frequency History of being awakened by headache New headache in patients with cancer or immune deficiency H/O IV drug use Recent head trauma or history of falls (especially in elderly) New-onset HA after age 50 HA precipitated by coughing, sexual activity, exercise Fever, personality changes or altered level of consciousness Strongly consider MRI imaging in the setting of trigeminal neuralgia or other cranial neuralgia syndrome Head CT has about a 95% chance of finding sub-arachnoid hemorrhage within the first 24 hours Differential Diagnosis of Secondary Headache Infection: meningitis, sinusitis, encephalitis Structural abnormality Cerebrovascular ischemia Intracranial hemorrhage: subarachnoid or parenchymal Head trauma Venous sinus thrombosis Malignant hypertension Vasculitis Altered intracranial pressure Carotid/vertebral dissection AV malformation or aneurysm Intraocular disease TMJ disorders Dental disease Cervical spine disease Congenital malformations: Chiari Type-1, arachnoid cysts Metabolic and toxic causes: noxious and poisonous gases Cranial/upper cervical neuralgias Clinical Presentations of Several Important Acute Emergencies Sudden Onset Severe Headache “Thunderclap Headache” Subarachnoid hemorrhage Cerebral Venous Thrombosis Cervical Arterial Dissection Spontaneous Intracranial Hypotension Pituitary Apoplexy Benign Exertional Headache Ischemic Stroke Hypertensive Crisis Third Ventricle Colloid Cyst Call-Fleming Syndrome [reversible cerebral vasoconstriction syndrome] Primary Thunderclap Headache Benign Orgasmic Headache Subarachnoid Hemorrhage Sudden onset first or worst headache. HA usually generalized and associated with neck stiffness, loss of consciousness, nausea, vomiting, photophobia. Blood pressure often rises significantly Fever may result from meningeal irritation 1/3 of patients may have early symptoms of more mild HA, neck stiffness, nausea, vomiting, syncope or visual change often attributed to “sentinel bleeds/headaches” Usually results from ruptured aneurysm or arterial-venous malformation (80%) Risk factors for rupture: size, smoking, evidence of cranial nerve compression, ETOH use, female gender, hypertension and exposure to sympathomimetics, increasing age Focal neurologic signs are uncommon and suggest AVM or parenchymal hemorrhage Diagnosis is usually with non-contrast head CT Lumbar puncture (if CT (-) but clinical suspicion high) demonstrates elevated pressure, gross blood, xanthochromia Intraparenchymal Hemorrhage Sudden onset headache pain that is often similar in quality to that seen in SAH Differentiating factors: focal neurologic signs, and more localized head pain Etiology most commonly is uncontrolled hypertension which produces structural changes to the walls of penetrating arteries- lipohyalinosis Most common sites include: putamen, thalamus, pons, cerebellum and lobar Other potential etiologies include vascular malformations, tumor, amyloid angiopathy Intraparenchymal Hemorrhage Intraparenchymal hemorrhage originating in the basal ganglia of a 57 year old man with poorly controlled hypertension The scan on the left shows bleeding from an AVM in a woman in her 20’s. On the right is a post-op scan Acute Subdural Hematoma Elderly and alcoholic patients with cerebral atrophy Usually there is a history of prior head trauma (although this may not clearly be present in elderly) Venous source with blood filling the potential space between the dura and arachnoid membranes Location: lateral cerebral convexities, around tentorial membrane, under the temporal lobes, posterior fossa Presenting signs: headache, confusion, drowsiness, focal neurologic signs (sometimes false localizing signs), seizures Acute Subdural Hematoma Internal Carotid or Vertebral Dissections Headache associated with these may be gradual or sudden in onset It is usually ipsilateral to the site of dissection and may involve the face and periorbital area Often there are focal neurologic signs (usually related to stroke or TIA) but these may be delayed in onset In carotid dissections Horner’s syndrome may be present Pulsatile tinnitus is also a classic symptom Often there is a history of recent head or neck trauma (including chiropractic manipulation) Diagnosis is via MRA or CTA On fat-suppressed T1 MRI carotid dissection may be seen as a crescent shaped signal abnormality when mural thrombus is present MRA showing the presence of internal carotid artery dissection Bacterial Meningitis Classically presents with headache, fever, stiff neck and subacute alterations in consciousness without focal neurologic signs Kernig and Brudzinski signs have very low sensitivity LP should be done in any patient with new onset headache associated with fever Clinically may be differentiated from encephalitis patients by the absence of seizure or focal neurological deficit Cerebral Venous Thrombosis Requires a high index of suspicion Predisposing conditions: pregnancy/peripartum, OCPs, obesity, dehydration, hypercoagulable states, infection Symptoms: headache, seizures, stupor, papilledema, vision loss, hemiplegia Oculomotor and abducens palsies may be present Diagnosis is usually by MR venogram Arrows showing filling defects due to superior sagittal thrombosis on MRV CSF Hypotension The classic presentation of this is postural related HA that worsens in the upright position and disappears within about 30 minutes when supine Often bifrontal or holocephalic with associated nausea, vomiting, tinnitus and sometimes cranial nerve palsies Most common cause is persistent CSF leak following lumbar puncture MRI may show slit like ventricles, prominent dural sinuses, subdural collections, downward displacement of the pons and cerebellar tonsils and diffuse dural enhancement Lumbar puncture shows low CSF pressure and high protein Treatment: fluid replacement, IV caffeine infusion, epidural blood patch Spontaneous Intracranial Hypotension Subdural fluid collections Diffuse Dural Enhancement Brain Tumors It is rare for brain tumors to present with headache in isolation Usually there are seizures, focal deficits, cognitive or speech impairments Classically the headaches associated with intracranial masses will wake patients from sleep or are present in the mornings Bending or straining may worsen or produce the headache Temporal Arteritis Consider in any patient over 50 with new onset headache Usually there are some associated symptoms of jaw claudication, transient vision loss or disturbance, fevers, fatigue or polymyalgia rheumatica There may be a tender, erythematous, nodular temporal artery ESR is usually greater than 60 Diagnosis is by temporal artery biopsy Idiopathic Intracranial Hypertension Typical symptoms are transient visual obscurations or sometimes complete vision loss caused by papilledema from increased intracranial pressure Diplopia from CN6 palsy sometimes occurs Headache is usually generalized frontal but may be unilateral. Most commonly affects obese women of childbearing age Diagnosis is confirmed by lumbar puncture with CSF pressures usually >25cm H2O Primary Headaches in the ER Reasons Migraineurs Come to the ER Unusual sudden onset of headache Associated intractable vomiting and dehydration Onset of headache during unusual circumstances: exertion, sexual intercourse Headache is refractory to usual measures Unusual features such as hemiplegic migraine, migrainous vertigo Drug seeking Treatment General measures Dehydration should be assess and treated as a first step Placement in dark quiet rooms Anti-emetics are often useful both for the nausea and sometimes the headache Avoidance of opioid medications Foster drug dependence Less effective than migraine-specific treatments Higher risk of rebound and analgesic overuse effect Antidopaminergic Agents Initially thought to only be useful for nausea/vomiting associated with migraine Have evidence for efficacy in aborting migraine pain Side effects Somnolence Akathisia Acute dystonia Prolonged QT interval- needs EKG Options include metaclopramide, prochlorperazine or chlorpromazine mgIV DHE Available in multiple formulations Signficant vasoconstrictive effects Contraindicated in pregnant patients Peripheral vascular disease Coronary artery disease Cerebrovascular disease Uncontrolled hypertension Typical dose is 1 mg IV preceded by antiemetic such as prochlorperazine or metaclopramide +/diphenhydramine Lower potential for headache recurrence than many other treatments NSAIDS and Steroids IV ketorolac given alone or in combination with antidopaminergic medications may be effective in patients failing triptans Randomized trials of steroids have had mixed results Meta-analyses have indicated modest benefit when steroids added to other abortive agents May be most effective in reducing HA recurrence rates at 24-72 hours Valproate and Magnesium Both have limited evidence for significant efficacy IV depacon (500 – 1000 mg) via rapid infusion Lack of cardiovascular effects No interaction with triptans No sedation Lack of dependence IV magnesium 2 grams Minimal side effects Safe in pregnancy Thank you for completing this module Questions? Contact me at: adam.quick@osumc.edu Survey We would appreciate your feedback on this module. Click on the button below to complete a brief survey. Your responses and comments will be shared with the module’s author, the LSI EdTech team, and LSI curriculum leaders. We will use your feedback to improve future versions of the module. The survey is both optional and anonymous and should take less than 5 minutes to complete. Survey