Corrosive injury
advertisement

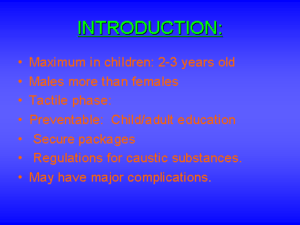
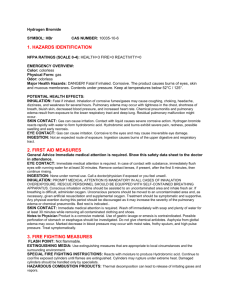
Corrosive injury 報告人: R3 張淳翔 Introduction 1. 2. Two groups: Pediatric: <5 y/o, accidental ingestion In Taiwan: alkaline oil Adult: Suicidal attempts, intentional More serious corrosive properties In Taiwan: 無煙鹽酸及通樂(Alkalis)、魔術靈、漂白水… Outcome: Caustic properties Amount, concentration, and physical form Duration of contact Treatment modalities Substances 1. 2. Alkalis: Most cases of caustic injury in western countries Cleaning agents (NaOH), drain openers, bleaches, toilet bowel cleaners, and detergents… Acids Less frequently in western countries; more common in countries like India (glacial acetic acid) Toilet bowel cleaners ( sulfuric, hydrochloric ), anti rust compounds ( hydrochloric, oxalic, hydrofluoric ), swimming pool cleaners ( hydrofluoric ) Alkalis V.S Acid Alkalis Acid PH > 7 Tasteless, odorless →larger amounts liquefaction necrosis => direct extension, deeper injuries Solid form : limited quantities, oropharyngal and supraglottic injuries Liquid form: significant quantities, esophageal injury, extensive, circumferential burns PH < 7 Pungent odor and noxious taste coagulation necrosis => formation of a coagulum layer : limit the depth of injury Less esophageal injury More gastric injury Pathophysiology Alkali-induced injury: 1. Liquefactive necrosis 1-2 days: Thrombosis of small vessels 2-4 days : Newly forming blood vessels , fibroblasts migration 4-7 days: Mucosal sloughing, bacterial invasion, inflammatory response, and development of granulation tissue > 2 weeks: Collagen deposition > 3 weeks: Scar retraction => may continue for several months Acid-induced injury: 2. Superficial coagulation necrosis Thromboses the underlying mucosal blood vessels and consolidates the connective tissue => Protective eschar Pathologic severity of injury 1. First-degree: 2. Second-degree 3. Superficial mucosal damage Focal or diffuse erythema, edema, hemorrhage Without scar formation Mucosal and sub-mucosal damage Ulcerations, exudates, vesicle formation, granulation, fibroblastic reaction Scar formation Third-degree Trans-mural Deep ulcers and black discoloration and perforation of the wall Pathologic severity of injury Clinical presentation Vary widely 1. 2. 3. Hoarseness, stridor, dyspnea => Airway evaluation Perforation: (During first 2 weeks) Retro-sternal or back pain Localized abdominal tenderness, rebound, rigidity, Psoas sign, obturator sign Massive hematemesis Dysphagia, odynophagia, drooling, nausea, vomiting Early signs and symptoms may not correlate with the severity and extent of tissue injury Oropharyngeal burns (-):10-30% esophageal burns(+) Oropharyngeal burns (+): 70% esophageal burns(-) Diagnosis and staging Upper gastrointestinal endoscopy Endoscopic grading system 1. 2. Grade 0: Normal Grade 1: Mucosal edema and hyperemia Grade 2A: Superficial ulcers, bleeding, exudates => Excellent prognosis Grade 2B: Deep focal or circumferential ulcers Grade 3A: Focal necrosis => Develop strictures: 70-100% Grade 3B: Extensive necrosis => Early mortality rate: 65% Late sequelae Stricture formation 1. Primarily in those with grade 2B or 3 injury Peak incidence: two months Occur as early as two weeks or as late as years after ingestion Gastric outlet obstruction 2. Early satiety , weight loss Less frequently 5-6 weeks ~ several years Usually acid ingestion Late sequelae Esophageal carcinoma 3. Incidence: 1000 to 3000-fold increase 3% have history of caustic ingestion Mean latency: 41 years (13-71years) Scar carcinoma: Less distensible => dysphagia presents earlier Lymphatic spread and direct extension Surveillance Begin 15-20 years after ingestion The time interval : No more than every 1-3 years Gastric carcinoma 4. rare occurrence Management – General management First aid 1. Identify the swallowed toxic agents Avoid: The use of emetics: re-exposes Neutralizing agents: thermal injury Gastric lavage: lead to perforation Transfer to hospital immediately 2. Keep NPO Insert NG tube ? R/O perforation Plain films of chest and abdomen Esophagogram: Water-soluble agent For ENT doctor Airway evaluation Oropharyngeal burns Management - Endoscopy Timing: 1. No later than 48 hours Usually avoided from 5-15 days Purpose: 2. Grading, manage appropriately Risk of perforation: 3. Low, under adequate sedation Extent: 4. Advance until a circumferential second-degree or third degree burn is seen To first part of duodenum Management - Oral intake NPO before PES Grade 1 or 2A injury: 1. 2. A liquid diet may be initiated Advance to a regular diet in 24 - 48 hours Grade 2B or 3 injury: 3. Controversial NG feeding, initiated after 24 hours => oral liquids are allowed after the first 48 hours if the patient is able to swallow saliva TPN use with delayed oral feeding (7 days) => Avoid food irritation Management - Prevention of strictures Steroids 1. In animal studies: incidence of stricture formation In human studies: Inconclusive so far NEJM. 1990: Prospective study over an 18-year period No benefit Related only to the severity of the corrosive injury Toxicol Rev. 2005: 1991-2004 in the English, German, French, Spanish No benefit Management - Prevention of strictures Antibiotics 2. Decreased bacterial counts, reduction in inflammation Mask the sign of more severe infection A prophylactic antibiotic, in the absence of steroid therapy, is not advocated Nasogastric tube 3. Feeding and stenting Contribute to the development of long strictures Routine use is not warranted Management - Prevention of strictures Total parental nutrition: 4. No human randomized study NPO allowing the re-epithelialization Intraluminal stent: 5. Controversial Prevents opposite raw surfaces contact and decreases stricture formation (Gastrointest Endosc. 2004) Management - Prevention of strictures Early dilataion: 6. Less than one week Controversial, most study: not recommended Start during the 1st week => The stricture can resolve more easily (Pediatr Surg Int. 2005 ) Anti-reflux treatment and Sucralfate: 7. Empirically use ; PPI, H2 blockers Prevention of injured esophageal mucosa from gastric acid reflux Management – Treatment of strictures Endoscopic dilatation 1. The goal: dilate the esophageal lumen to 15 mm Perforation rate: 0.5% Special consideration: Long, eccentric strictures: risk of perforation increased Thick-walled strictures: recur rapidly Multiple sessions: elective esophageal resection Intraluminal stent 2. Temporary placement of a self-expanding plastic stent Successful in case reports Surgery 3. Esophagectomy with colonic interposition Gastric transposition: high leak rate Perform 6 months later Proposal for management Conclusion 1. Signs and symptoms alone are an unreliable guide to injury 2. Early endoscopy has a crucial role 3. Grading, manage appropriately Reference 1. Ramasamy K, Gumaste VV. Corrosive ingestion in adults. J Clin Gastroenterol. 2003;37:119-24. 2. Huang YC, Ni YH, Lai HS, Chang MH. Corrosive esophagitis in children. Pediatr Surg Int. 2004;20:207-10. 3. Pelclova D, Navratil T. Do corticosteroids prevent oesophageal stricture after corrosive ingestion? Toxicol Rev. 2005;24:125-9. 4. Baskin D, Urganci N, Abbasoglu L, et al. A standardised protocol for the acute management of corrosive ingestion in children. Pediatr Surg Int. 2004;20:824-8. 5. Anderson KD, Rouse TM, Randolph JG. A controlled trial of corticosteroids in children with corrosive injury of the esophagus. N Engl J Med. 1990;323:637-40. 6. Poley JW, Steyerberg EW, Kuipers EJ, et al. Ingestion of acid and alkaline agents: outcome and prognostic value of early upper endoscopy. Gastrointest Endosc. 2004;60:372-7. 7. Tiryaki T, Livanelioglu Z, Atayurt H. Early bougienage for relief of stricture formation following caustic esophageal burns. Pediatr Surg Int. 2005;21:78-80. 8. Evrard S, Le Moine O, Lazaraki G, et al. Self-expanding plastic stents for benign esophageal lesions. Gastrointest Endosc. 2004;60:894-900. Thanks for your attention