Supraventricular Tachycardia in Infancy and Childhood
advertisement

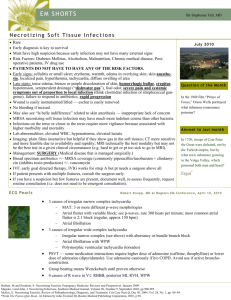
Supraventricular Tachycardia in Infancy and Childhood Terrence Chun, MD Pediatric Electrophysiology and Pacing Cardiac electrical anatomy SVT - Overview Rapid rhythm that involves or is driven by structures in the upper heart Incidence up to 1:250 children Generally well-tolerated, even fast rates Risk of life-threatening arrhythmias is uncommon Narrow vs. Wide QRS Not all narrow QRS complex tachycardia is supraventricular tachycardia Not all wide QRS complex tachycardia is ventricular tachycardia SVT Mechanisms - Overview Reentrant rhythms Automatic rhythms SVT mechanisms – Automatic Rhythms Originate from a particular focus “Warm-up” and “cool-down” behavior Respond to drugs and maneuvers that affect myocardial automaticity May be suppressed by faster rates Usually do not respond to cardioversion (typically pause, then restart) SVT mechanisms – Automatic Rhythms Left atrial focus 2:1 AVN conduction SVT mechanisms – Reentrant rhythms Requires a “circuit” of tissue to create repetitive activation Must have appropriate conditions to perpetuate reentrant rhythm Usually abrupt onset and termination Regular, with little variation in rate Often will respond to cardioversion SVT mechanisms – Reentrant rhythms Diagnostic methods 12-lead electrocardiogram ! ! ! Post-op atrial/ventricular pacing wires Esophageal pacing leads Adenosine can be diagnostic Invasive electrophysiology study Diagnostic methods Always Always Always record a rhythm strip during any intervention (adenosine, cardioversion, Valsalva, etc.) Diagnostic methods Record a rhythm strip ECG clues to diagnosis Wide vs. narrow complex Regular vs. irregular Abrupt vs. gradual P wave relationship to QRS Parade of Rhythms Automatic Arrhythmias Automatic rhythms – Sinus Tachycardia Sinus node – fish-shaped structure with “head” at SVC-RA junction and “tail” extending along RA wall S-tach usually due to increased sympathetic discharge, fever, anemia, hypovolemia, hyperthyroidism, etc. Inappropriate sinus tachycardia - rare Automatic rhythms – Sinus Tachycardia Dx Rate greater than normal range, but usually less than 200 P wave axis normal (0 ~ +90°) PR interval normal Tx Treat the cause Automatic rhythms – Automatic Atrial Tachycardia Originates from a focus in either the right or left atrium, or atrial septum Commonly from atrial appendages, crista terminalis, pulmonary veins Can also be due to central lines, etc. Also called “ectopic atrial tachycardia” although any automatic rhythm other than sinus rhythm is technically “ectopic” Automatic rhythms – Automatic Atrial Tachycardia Dx Speeds-up and slows-down, rates vary P wave axis abnormal PR interval may be abnormal (it is a function of distance from focus to AVN) May see 2° AV block (e.g. Wenckebach or 2:1 at higher atrial rates) Adenosine P waves “march through” despite AV block Automatic rhythms – Automatic Atrial Tachycardia Automatic rhythms – Automatic Atrial Tachycardia Tx Remove source (check CXR and pull back PICC) Beta-blockers Esmolol infusion in ICU setting propranolol, atenolol Amiodarone, others Catheter ablation Automatic rhythms – Junctional Tachycardia Originates from around the AV junction Also called “JET” (Junctional Ectopic Tachycardia), because it sounds cool Rate 170-200+ Most commonly seen post-operatively, usually self-limited Congenital forms, more persistent Automatic rhythms – Junctional Tachycardia Dx AV dissynchrony Sinus P wave at different rate than narrow QRS Atrial wire ECG (in post-op with pacing wires) “Cannon a-waves” on CVP monitor Retrograde P waves (abnormal Pw axis) May be on top, before, or after QRS Automatic rhythms – Junctional Tachycardia Cannon a-waves Automatic rhythms – Junctional Tachycardia Tx Reduce catecholamines Decrease inotropic drips Pain control and sedation Cooling/hypothermia Drugs (amiodarone) ECMO Catheter ablation(?) Parade of Rhythms Reentrant Arrhythmias Reentrant rhythms – Pathway Mediated Tachycardia Bypass tract of conductive tissue connects atrium to ventricle Most common mechanism of SVT in children Rate 180-240 May be “manifest” (e.g. WPW) or concealed (no preexcitation) Pathway can be anywhere on mitral or tricuspid annuli, usually left-sided Reentrant rhythms – Pathway Mediated Tachycardia Orthodromic reciprocating tachycardia “Runs correctly” with normal conduction Down AV node (narrow QRS) Up accessory pathway (retrograde) Retrograde P waves may be visible after QRS Antidromic reciprocating tachycardia “Runs against” normal conduction Down accessory pathway (wide QRS) Up AV node (retrograde) Less common Reentrant rhythms – Pathway Mediated Tachycardia Dx Electrocardiogram Rhythm strips of start and stop of SVT Reentrant rhythms – Pathway Mediated Tachycardia Tx Valsalva maneuvers, Ice to face Adenosine (technique matters!) Antiarrhythmic drugs Beta blockers (watch blood glucose in infants!) Digoxin (limited value; digitalization only in difficult situations) Others (Verapamil, Flecainide, Sotolol, etc.) Catheter ablation Reentrant rhythms – Wolff-Parkinson-White Syndrome Electrocardiogram findings Short PR interval Wide QRS complex Delta wave Reentrant rhythms – Wolff-Parkinson-White Syndrome Reentrant rhythms – Wolff-Parkinson-White Syndrome Clinical symptoms Palpitations SVT Note narrow QRS and lack of delta wave! Reentrant rhythms – Wolff-Parkinson-White Syndrome Sudden death(!) Atrial fibrillation Rapid conduction over bypass tract Ventricular fibrillation Risk 0.1-0.6% per year Reentrant rhythms – Wolff-Parkinson-White Syndrome Tx Tachycardia control Risk stratification Recognition ±Drugs (patient/family choice) Digoxin generally contraindicated Holter Exercise testing Invasive electrophysiology testing Catheter ablation Reentrant rhythms – AV Node Reentry Tachycardia More common in teens and adults Tachycardia circuit contained within atrioventricular node Activates atria at the “top” of the circuit, ventricles at “bottom” of circuit, nearly simultaneously Rate 200-250 Usually cannot see retrograde P waves Reentrant rhythms – AV Node Reentry Tachycardia Reentrant rhythms – AV Node Reentry Tachycardia Tx Adenosine Cardioversion ±Pharmacotherapy Beta blockers Digoxin Others Catheter ablation Reentrant rhythms – Atrial Flutter “Flutter” circuit around anatomic structures in atrium Eustachian valve Crista terminalis Fossa ovalis Surgical incisions Reentrant rhythms – Atrial Flutter Atrial rate ~300 (higher in neonates) Ventricular rate depends on AV node conduction 1:1 300/min 2:1 150/min 3:1 100/min May be 3:1 then 2:1 then… Reentrant rhythms – Atrial Flutter Sawtooth “flutter” waves (may or may not be helpful) Reentrant rhythms – Atrial Flutter Dx Electrocardiogram Adenosine blocks AV node; flutter waves continue Tx Rate control – digoxin, beta blockers, etc. Overdrive pacing DC cardioversion Catheter ablation Threatening Rhythms Atrial fibrillation in high-risk WPW Persistent prolonged SVT Danger of ventricular fibrillation Tachycardia induced cardiomyopathy (reversible) SVT in compromised cardiac status Syncope or cardiovascular collapse Treatment Pearls Adenosine 0.1-0.4 mg/kg/dose Very short half-life (seconds) Central administration can be helpful, but not necessary Rapid saline bolus (5-10 ml) essential Stopcock on venous access is helpful DC Cardioversion Dose Cardioversion 0.25-1 J/kg Defibrillation 1-2 J/kg Synchronized (avoids making worse) Paddles – front+apex Patches Front+apex Front+back Catheter Ablation Multiple catheters Size limitations Ideally > 15 kg, but can be done in infants if necessary Can be curative ~95% success rate in children Record a Rhythm Strip! Especially during interventions Most SVT in infants and children is hemodynamically well-tolerated Proper diagnosis can guide appropriate therapy RA/LA/RL/LL limb leads give 6 electrograms (I, II, III, aVL, aVR, aVF)