Where to take the biopsy for IMF?
Immunofluorescence and skin biopsies
Dr Claire Murray
Normal Skin
Perilesional skin
Lesion
Procedure for biopsy
Ellipse incisional biopsy helps preserve an intact blister. Punch biopsies are more likely to disrupt the roof
For histology
For IMF
Direct Immunoflorescence
• Performed on lesional or perilesional tissue from skin, mucosa or conjunctiva
• Detects in vivo deposition of:
– Immunoglobulins (IgA, IgG, IgM)
– Complement proteins (C1, C3)
– Fibrinogen
• Used for
– Autoimmune blistering disorders
– Connective tissue disease (SLE, DM)
– Vasculitis
Direct Immunoflorescence
• Uses single primary antibody chemically linked to a fluorophore
• Fluorophore = a fluorsecent chemical compound that can re-emit light upon light excitation.
• Antibodies are directly applied to the lesional/perilesional tissue
Indirect Immunofluorescence
• Patient’s serum is tested for antibodies directed towards a defined antigen
• A double layer technique
– Primary antibody (within serum) binds to the target antigen on tissue (monkey oesophagus or similar)
– Secondary antibody carrying the fluorophore binds to the primary antibody as fluorescent label
• Multiple secondary antibodies can bind to single primary antibody providing signal amplification
Where to take the biopsy for DIMF?
• Blistering disorders – perilesional skin
– Perilesional skin = normal skin immediately adjacent to a lesion
– Immune deposits are degraded in inflamed or blistered skin which can result in false negative DIF
– avoid an ulcer or an area where the epidermis is disrupted
– Avoid active lesions
• Connective tissue diseases – lesional skin
– For SLE lupus band test x 2 biopsies of lesional and non-sun exposed normal skin (buttock or inner thigh)
– Avoid old lesions and facial lesions
• Vasculitis – lesional skin
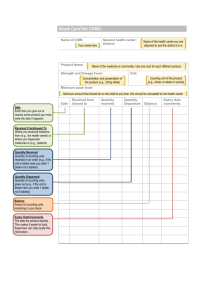
How to transport the biopsy material?
• Rinse biopsy in saline
• Place in saline soaked gauze
• Send unfixed in Michels transport medium
– does not fix the tissue
– maintains isotonticity and pH of the tissue for around
2 days
– stabilises proteins in tissues to allow preservation of antigenicity and use of immunofluroescence.
• Keep in fridge overnight (do not freeze in uncontrolled manner)
Fluorescent
Microscopy
• Tissue sample acts as light source
• Microscope emits high intensity,
excitation light
• Fluorophores illuminated by the excitation light (UV light)
• Flurophores emit longer lower energy wavelength light
(fluorescent light)
• Fluorescent light is separated from surrounding radiation by filters
• Filters only allow light with same wavelength as fluorescing material through
• The low energy light can be seen against a dark background
• Slides stored in fridge to reduce degradation of immunofluorescence
• Photobleaching (fading) of slides occurs when over exposed to the high intensity light
• Photobleaching can be reduced by reducing the insity of the light or the duration of time the tissue is exposed to the light
Bullous pemphigoid
• Most common subepidermal autoimmune bullous disorder
• Typically affects elderly
• Common sites are lower abdomen, groins, legs and arms
Bullous pemphigoid
• Unilocular, subepidermal blister
• Roof attenuated or normal in early lesions.
May become necrotic in large or older lesions
• Blister contents: fibrin, inflammatory cells
Bullous pemphigoid
• Inflammatory (cell rich) blister
– Predominant eosinophils
– Variable neutrophils and lymphocytes
• Non-inflammatory (cell poor) blister
– Sparse inflammatory cells
– Can be appearance in very early lesions
Bullous pemphigoid
• Festooning of dermal papillae = preservation of outline dermal papillae
• Severe dermal oedema
• Perivascular eosinophils and histiocytes
• Eosinophilic spongiosis in adjacent epidermis
Bullous pemphigoid
Homogenous, linear deposition of IgG and/or C3 along the dermoepidermal junction
Direct IMF
Differential Diagnosis of BP
Bullous
Pemphigoid
Epidermolysis
Bullosa
Bullous SLE
Linear IgG and C3 Linear IgG and C3 Linear IgG and C3
Indirect IML
Salt-split skin
IgG antibodies
75 – 80%
Roof
IgG antibodies
25 – 50%
Floor
IgG antibodies
60%
Floor
Split skin immunofluorescence
• A modified indirect IMF technique
• Normal skin is split to create artificial blister cavity
• Split achieved by immersing in saline
• serum applied to split skin
• Antibodies localised to roof or floor of blister
IgG localised to roof in bullous pemphigoid
Epidermolysis Bullosa
• Group of non-inflammatory skin disorders characterised by development of blisters following minor trauma
• Autosomal dominant or recessive inheritance
• Presentation varies depending on the class of the disease
Epidermolysis Bullosa Acquisita
• Non-inherited variant
• Onset in mid-life
• Development of noninflammatory bullae after minor trauma
• Extensor surfaces of limbs most affected
Epidermolysis Bullosa Acquisita
• Sub-epidermal bulla with fibrin
• Scanty inflammatory cells
• Intact roof of blister
• Variable inflammatory infiltrate in dermis
• PAS stain demonstrates the level of split within the BM with most in the roof
Epidermolysis Bullosa Acquisita
Direct IMF: intense deposition of IgG and faint C3 along dermoepidermal junction
Epidermolysis Bullosa Acquisita
Salt-split skin IMF: antibodies bind to the floor of the blister
Lupus Band Test for Lupus erythematosus
• Direct IMF performed on lesional and nonlesional sun-protected skin
• Band-like deposition of
IgG, IgM & C3 at dermoepidermal junction in lesional skin
• Epidermal nuclear IgG in small percentage
Lupus Band Test for Lupus erythematosus
• False positive lupus band test in 30% of sunexposed skin biopsies from unaffected patients
• Negative IMF can occur in early lesions, treated lesions, lesions from the trunk, when in remission.
Bullous SLE
• A rare variant of SLE
• Subepidermal blisters
• Neutrophils in the papillary dermis
• Lymphocytes around vessels in the superficial plexus
• Linear or mixed linear/granular deposition of IgG and less commonly
IgA and/or IgM along dermoepidermal junction
Bullous SLE
• Linear or mixed linear/granular deposition of IgG and less commonly IgA and/or IgM along dermoepidermal junction
• Salt-split IDIMF shows deposition along floor of blister
Porphyria Cutanea Tarda
• Rare inherited or acquired disease (liver disease
• Defect in enzyme uroprophyrinogen
decarboxylase involved in synthesis of haem pathway resulting in accumulation of porphyrins
• Blisters arise on sunexposed sites
Porphyria Cutanea Tarda
• Subepidermal blister
• Cell-poor
• Festooning of dermal papillae
• Deposition of hyaline material in BM and around dermal vessels
• ‘caterpillar bodies’ – hyaline material within epidermis that stains with
PAS
Porphyria Cutanea Tarda: DIMF
• IgG, IgM and C3 outline vessels in the papillary dermis ‘doughnut’ distribution
• Linear deposition of
IgG, IgM and C3 at the dermoepidermal junction.
Dermatitis Herpetiformis
• Associated with coeliac disease
• Affect all ages
• Lesions on posterior scalp, back, buttocks, backs of arms and legs
• Intensely pruritis, widespread, papulovesicular erruption
Dermatitis Herpetiformis
• Neutrophilic abscesses within the dermal papillae in early lesions
• Multiloculated subepidermal bullae develop
• Intense neutrophilic inflammatory infiltrate within the blister cavity
Dermatitis Herpetiformis
• Perilesional skin should be sampled
• Granular deposits of IgA seen in papillary dermis
• Granular-linear pattern may also be seen
Pemphigus
• Pemphigus vulgaris
• Pemphigus vegetans
• Pemphigus foliaceous
• Paraneoplastic pemphigus
• IgA pemphigus
Pemphigus Vulgaris
• Most common (80% cases)
• Middle age onset
• Begins in mouth (50%)
• Spreads to involve the skin within weeks/months
• Bullae and large and flacid and rupture easily
• Autoantibodies to desmoglein 3
Pemphigus Vulgaris
• Suprabasal bullae
• Acantholysis
• Dermal papillae project into cavity like villi
• ‘Tombstone’ pattern – layer of basal cells remain attached to dermis
Pemphigus Vulgaris
• Acantholytic cells round, eosinophilic & pyknotic nuclei
• Occasional eosinophils
& neutrophils
• Dermal perivascular infiltrate composed of eoinophils and neutrophils
Pemphigus IMF (perilesional skin)
• Intercellular deposition of IgG and C3
• Individual keratinocytes outlined like chicken wire
• Serum antibodies can be demonstrated with indirect IMF using monkey oesophagus
Lichen Planus
• ‘Sawtooth’ epidermal hyperplasia
• Wedge shaped hypergranulosis
• Civatte and colloid bodies
• Basal vacuolar degeneration
• Band-like lymphocytic infiltrate in papillary dermis
Lichen planus IMF
• Helps exclude SLE and other bullous disease in difficult cases
• Direct IMF highlights colloid bodies in papillary dermis
• Colloid bodies can stain for IgM and C3
• Irregular band of fibrinogen along basal layer
Lichen planus pemphigoides
• LP associated with pemphgoid like blisters
• More in common in men, 4-5 th decade
• Usually preceded by typical LP
• Blisters more common on extremities
Lichen planus pemphigoides
• Lichenoid lesions are typical
• Bullous lesions show subepidermal blister
• Cell rich or poor variants both occur
Lichen planus pemphigoides IMF
Direct IMF Linear deposition of IgG and C3 along dermoepidermal junction
Salt-split skin indirect IMF • Serum contains IgG basement membrane antibody in 50-60%
• IgG labels roof of blister
Leukocytoclastic Vasculitis
• Biopsy lesional skin
• Early lesions < 6 hours old more commonly positive
• Deposition of fibrinogen, C3 and IgM all seen in vessel walls
Henoch-Schonlien Purpura
(leukocytoclastic Vasculitis)
• Represents 10% of all cutaneous vasculitis
• Purpuric rash on lower legs
• Histology indistinguishable from other LCV
• Deposition of IgA in vessel walls in involved and uninvolved skin