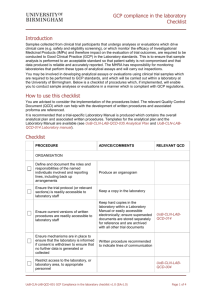
Procedure - University of Birmingham Intranet
advertisement

Procedures for GCP compliance in the laboratory UoB QMS reference number: UoB-CLN-LAB-SOP-001 Purpose: The analysis or evaluation of samples collected from subjects participating in clinical trials forms a key part of the clinical trials process. The purpose of this SOP is to describe procedures which will ensure that sample analyses or evaluations which drive clinical care (e.g. safety and eligibility screening), or which monitor the efficacy of Investigational Medicinal Products and therefore impact on the evaluation of trial outcomes, are performed to an acceptable standard which will ensure that patient safety is not compromised, that data is reliable and accurately reported, and in accordance with accepted principles of GCP, with applicable law, and with established policies of the University of Birmingham. Scope: This SOP applies to all laboratories within the University of Birmingham that undertake clinical trial sample analyses or evaluations which drive clinical care (e.g. safety and eligibility screening), or which monitor the efficacy of Investigational Medicinal Products and therefore impact on the evaluation of trial outcomes. Implementation plan: This template will be implemented directly after the implementation date. Date of implementation: 01-Mar-2016 Property of the University of Birmingham, Vincent Drive, Edgbaston, Birmingham, B15 2TT, United Kingdom. Not to be printed, copied or distributed without authorisation Copies are only valid for 14 days and may be subject to amendment at any time. Refer to the electronic document management system for the latest version. Document code: UoB-CLN-LAB-SOP-001 Version no: 2.0 Print Date: 12-Mar-16 Page: 1 of 7 Procedures for GCP compliance in the laboratory Responsibilities: Individual clinical trials must identify named individual(s) who assume responsibility for conducting the scientific analyses, for reporting the results of the analysis or evaluation, for assessing risks to sample and data integrity following adverse events, for reporting any deviations from written procedures or the clinical protocol and for reporting serious breaches in GCP. They must also identify the personnel responsible for laboratory and equipment management and for monitoring GCP compliance. Responsibilities and reporting lines will be established and documented prior to the initiation of analytical work, for example, by the production of an organogram. Procedure: Develop and implement written procedures and the appropriate documents for record keeping (see below). Consider using the QCDs developed as part of the UoB Laboratory QMS in order to produce these. The QCDs include checklists, guidelines, templates, and example proforma. They are listed at the end of this SOP. The GCP in the laboratory checklist (see UoB-CLN-LAB-QCD-001) lists the relevant tools against specific tasks. Consider developing a version-controlled Laboratory Manual which contains the overall analytical plan and all trial-specific procedures pertaining to the analytical process (see UoB-CLN-LAB-QCD-014 Laboratory Manual). Prior to the start of clinical trial sample analysis Define and document the roles and responsibilities of the named individuals involved (see ‘Responsibilities’ section above). Ensure that reporting lines are clear. Properly validate analytical assays with defined acceptance criteria. Document the assay validation process. Ensure that laboratory staff are appropriately trained on procedures, on relevant policies and SOPs, on current relevant MHRA guidelines, and on GCP. Record training and competencies. Ensure that the appropriate laboratory risk assessments are in place. Throughout clinical trial sample analysis Ensure there is a mechanism in place to ensure that the laboratory is informed in a timely manner if consent is withdrawn so that no further data is generated or collected. Ensure that a copy of the trial protocol, or as a minimum, the sections of the clinical protocol which are relevant to the activities undertaken in the laboratory (and amendments relevant to the laboratory analyses), is always available to laboratory staff. Ensure that current versions of the trial-specific written procedures and associated documentation (e.g. proforma) relevant to the analytical procedures are readily available to laboratory staff. Restrict access to the laboratory, or laboratory area, to appropriate personnel as far as possible. Maintain and document laboratory housekeeping regimes. Ensure that all equipment is monitored, maintained and calibrated. Ensure that records of this are maintained and stored safely and securely. These records should be archived appropriately at the end of the clinical trial. Ensure that equipment which is shared with other researchers analysing non-clinical trial samples is maintained to a standard that will not compromise the integrity of clinical trial data. Store and manage key reagents, controls and standards involved in the analysis according to trial-specific procedures. If it is necessary to use batches (or lots) of key reagents, controls and standards different to those used during the initial validation, consider re-validation of the assay and document this as an amendment to the original validation report. Maintain accurate records associated with sampling kits sent to sites for the purposes of sample collection to enable traceability of all components. Document code: UoB-CLN-LAB-SOP-001 Version no: 2.0 Print Date: 12-Mar-16 Page: 2 of 7 Procedures for GCP compliance in the laboratory Ensure clinical trial samples received into the laboratory are processed, stored and analysed according to trial-specific procedures and remain traceable throughout their life cycle. Ensure that records are kept which evidence that samples have been processed, stored and analysed according to the trial-specific procedures. Maintain raw analytical data produced safely and securely, either electronic or hard copy. Review and report analytical results according to trial-specific procedures. Ensure that the circumstances under which an analysis may be repeated for a particular sample, for example if an out of range or aberrant result is obtained, are clearly defined and implemented. Ensure electronic data is stored securely and backed up. Carry out internal audits/quality checks as and when appropriate. Document the results and any corrective and preventative actions (which may require updating written procedures). Laboratory adverse events Ensure that laboratory adverse events are dealt with and reported in a timely manner according to trial-specific procedures. Always assess the risk of the adverse event on patient safety, sample and data integrity and document this. Document and implement any corrective and preventative actions (which may require updating written procedures). Related documents: University of Birmingham Good Clinical Practice in the Laboratory Quality Manual UoB-CLN-LAB-QCD-001 GCP compliance in the laboratory checklist UoB-CLN-LAB-QCD-002 Equipment maintenance and calibration checks UoB-CLN-LAB-QCD-003 Temperature monitoring UoB-CLN-LAB-QCD-004 Laboratory access UoB-CLN-LAB-QCD-005 Laboratory housekeeping UoB-CLN-LAB-QCD-006 Management of shared equipment UoB-CLN-LAB-QCD-007 Receipt and traceability of trial participant samples UoB-CLN-LAB-QCD-008 Analytical assay validation UoB-CLN-LAB-QCD-009 Analytical assay failure UoB-CLN-LAB-QCD-010 Impact assessment of equipment failure or equipment calibration failure UoB-CLN-LAB-QCD-011 Handling and maintaining raw data UoB-CLN-LAB-QCD-012 Receipt, labelling and storage of reagents UoB-CLN-LAB-QCD-013 Management and storage of analytical standards UoB-CLN-LAB-QCD-014 Laboratory Manual UoB-CLN-LAB-QCD-015 Review and release of results UoB-CLN-LAB-QCD-016 Adverse events in the analytical laboratory UoB-CLN-LAB-QCD-017 Laboratory audit and quality checks UoB-CLN-LAB-QCD-018 Repeat analysis UoB-CLN-LAB-QCD-019 Procedures following failure of storage unit Document code: UoB-CLN-LAB-SOP-001 Version no: 2.0 Print Date: 12-Mar-16 Page: 3 of 7 Procedures for GCP compliance in the laboratory UoB-CLN-LAB-QCD-020 Laboratory training record UoB-CLN-LAB-QCD-021 Equipment maintenance record UoB-CLN-LAB-QCD-022 Single channel pipette calibration check record UoB-CLN-LAB-QCD-023 Multi channel pipette calibration check record UoB-CLN-LAB-QCD-024 Thermometer and temperature probe calibration check record UoB-CLN-LAB-QCD-025 Balance calibration check record UoB-CLN-LAB-QCD-026 Housekeeping record UoB-CLN-LAB-QCD-027 Training record for shared equipment UoB-CLN-LAB-QCD-028 Analytical failure report UoB-CLN-LAB-QCD-029 Impact assessment of equipment failure or equipment calibration failure report UoB-CLN-LAB-QCD-030 Reagent receipt and storage record UoB-CLN-LAB-QCD-031 Temperature monitoring record UoB-CLN-LAB-QCD-032 Adverse event report UoB-CLN-LAB-QCD-033 Analytical assay validation plan UoB-CLN-LAB-QCD-034 Analytical assay validation report UoB-CLN-LAB-QCD-035 Analytical plan UoB-CLN-LAB-QCD-036 Self-assessment of GCP compliance in the laboratory UoB-CLN-LAB-QCD-037 Samples collected during clinical trial UoB-CLN-LAB-QCD-038 Laboratory Good Clinical Practice UoB-CLN-LAB-QCD-039 Blood processing record UoB-CLN-LAB-QCD-040 Record of sampling kit References: European Medicines Agency (EMA): Reflection paper for laboratories that perform the analysis or evaluation of clinical trial samples Guidance on the maintenance of regulatory compliance in laboratories that perform the analysis or evaluation of clinical trial samples (2012): http://www.ema.europa.eu/docs/en_GB/document_library/Regulatory_and_procedural_guideli ne/2012/05/WC500127124.pdf Good Clinical Laboratory Practice. A quality system for laboratories that undertake the analyses of samples from clinical trials v2 2012. BARQA: http://www.therqa.com/assets/js/tiny_mce/plugins/filemanager/files/Publications/Booklet_Dow nloads/Good_Clinical_Laboratory_Practice_GCLP.pdf Document code: UoB-CLN-LAB-SOP-001 Version no: 2.0 Print Date: 12-Mar-16 Page: 4 of 7 Procedures for GCP compliance in the laboratory Abbreviations and Definitions: Term Description GCP Good Clinical Practice guidelines Laboratory A facility that conducts manipulation, analysis or evaluation of samples collected as part of a clinical trial; such analysis or evaluation may include the generation of pharmacokinetic or pharmacodynamic data, safety data, primary efficacy data, histopathology data or data used to support any other stated primary or secondary end point. Laboratory adverse events A laboratory adverse event refers to any event which may compromise patient safety, sample or data integrity. Examples include security breaches, equipment failure or calibration failure, analytical failures, or the production of aberrant or out of range results. Policies Policies are developed to describe the approach of the UoB on areas that heavily regulated. Policies may also be developed when there is ambiguity in how regulatory requirements should be implemented in the QMS or when procedures to be captured in the QMS address areas controversial within the UoB at the time of implementation. Policies explain why the UoB has its procedures, especially when they seem to deviate from the regulatory requirements. Policies should be read in conjunction with the relevant SOP. Policies that are not part of a Quality Manual are coded up as ‘POL’. QCD See “Quality Control Documents” QMS Quality Management System Quality Control Documents Quality Control Documents can be instructions, forms, templates or checklists. They are developed to share best practices, promote standardisation to guarantee quality standards are maintained and reduce resources otherwise needed to develop similar documents. Unless indicated otherwise in the relevant SOP, QCDs are not mandatory and are designed to be an optional aid to UoB staff. Quality Management System A Quality Management System (QMS) is a system that includes procedures and policies to describe how certain tasks should be performed and that encapsulate any standards and/or regulatory requirements that may apply to those tasks. By adhering to the Quality Management System, the user and the UoB will be assured that applicable regulations are adhered to. SOP See “Standard Operating Procedures” Standard Operating Procedures Standard Operating Procedures are detailed written instructions to achieve uniformity in the performance of a specific function. They define tasks, allocate responsibilities, detail processes, indicate documents and templates to be used and cross-reference to other work instructions and guidance or policy documents. They are standards to which the UoB may be audited or inspected. UoB University of Birmingham See Glossary of Terms Document code: UoB-CLN-LAB-SOP-001 Version no: 2.0 Print Date: 12-Mar-16 Page: 5 of 7 Procedures for GCP compliance in the laboratory Development summary: Author: Name: Jane Steele Function: Director, Advanced Therapies Facility Date: See original copy Reviewed by: Clinical Trials Oversight Committee Signature: See original copy Signature: See original copy Signature: See original copy Authorised by: Name: Wilma van Riel Function: Head of Clinical Research Compliance Date: See original copy Name: Professor Julian Bion Function: Chair of the Clinical Trials Oversight Committee Date: See original copy Issue date: Supersedes: Procedures for GCP compliance in the laboratory v1.0 (EAv1.0) Reason for update: Findings and recommendations following MHRA inspection 23rd – 25th June 2015; clarification included regarding record keeping in relation to samples and assays. Review of final version: Date: Reviewed by: Document code: UoB-CLN-LAB-SOP-001 Version no: 2.0 Signature: Outcome: Print Date: 12-Mar-16 Page: 6 of 7 Procedures for GCP compliance in the laboratory Editorial Amendments Tick box if not applicable Reason for update: Date of amendment: Supersedes: Editor: Name: Signature: Function: Date: Authoriser: Name: Signature: Function: Date: Document code: UoB-CLN-LAB-SOP-001 Version no: 2.0 Print Date: 12-Mar-16 Page: 7 of 7