PARAPLEGIA & SPINAL CORD SYNDROMES II
advertisement

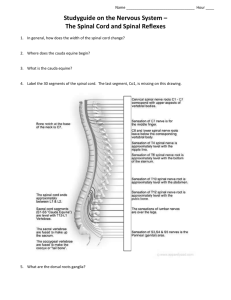
Dr. M. Sofi MD;FRCP(London); FRCPEdin; FRCSEdin Overview of Spinal Cord Information highway between brain and body Extends through vertebral canal from foramen magnum to L1 Each pair of spinal nerves receives sensory information and issues motor signals to muscles and glands Spinal cord is a component of the Central Nervous System while the spinal nerves are part of the Peripheral Nervous System Functions of the Spinal Cord • The spinal cord has two major functions: Carrying information: Spinal cord transmit information from body organs and external stimuli to the brain and send information from the brain to other areas of the body • Coordinating reflexes: coordinates reflexes without the involvement of the brain, thus, the spinal cord has both communicative and integrative functions. Reflex actions are automatic, unlearned, involuntary, and inborn responses. These actions are sudden in nature and have a purpose of protecting the individual or his organs from sudden danger Somato-sensory Organization Somatosensory organization Pyramidal tracts Lateral Coticospinal Tract Anterior Corticospinal Tract Extrapyramidal Tracts Rubrospinal Reticulaospinal Olivospinal Vestibulospinal Descending Tracts Somato-sensory Organization Sensory & Ascending Pathways Dorsal Column Medial Lemniscus Gracile fasciculus Cuneate fasciculus Spinocerebellar Tracts Posteriors pinocerebellar Anterior spinocerebellar Anterolateral System Lateral spinothalmic tract Anterior spinothalmic tract Spino-olivary tract Ascending tracts BLOOD SUPPLY SPINAL CORD Paraplegia & Spinal cord syndromes Spinal shock is a loss of sensation accompanied by motor paralysis with initial loss but gradual recovery of reflexes, following a spinal cord injury (SCI) – most often a complete transaction. Reflexes in the spinal cord caudal to the SCI are depressed hyporeflexia/areflexia), while those rostral to the SCI remain unaffected. ‘Shock' in spinal shock does not refer to circulatory collapse, and should not be confused with neurogenic shock. Phase Time Physical exam finding Underlying physiological event 1 0-1d Areflexia/Hyporeflexia Loss of descending facilitation 2 1-3d Initial reflex return Denervation supersensitivity 3 1-4w Hyperreflexia (initial) Axon-supported synapse growth 4 1-12m Hyperreflexia, Spasticity Soma-supported synapse growth Paraplegia & Spinal cord syndromes Classification of etiology LMN type/Flaccid paraplegia UMN type/ Spastic paraplegia Spinal cord lesion Cortical lesion Tumor Falx Cerebri Superior Sagital Sinus Thrombosis Compressive Myelopathy Non-compressive Myelopathy Paraplegia & Spinal cord syndromes Classification of etiology COMPRESSIVE MYELOPATHY EXTRAMEDULLARY EXTRADURAL DISC INTRAMEDULLARY INTRADURAL VERTEBRAL Meningoma, Neurofibroma, Arachnoditis Syringomyelia, Ependymymoa, Glioma, Astrocytoma Paraplegia & Spinal cord syndromes Classification of etiology Non-compressive myelopathies INFAMMATORY INFECTIOUS: VIRAL, BACTERIAL ,FUNGAL PARASTIC AUTOIMMUNE: SLE, SJOGREN, SARCOIDOSIS, BECHET S, MCTD DEMYELINATING: MS,NMO, ADEM, POST VIRAL POST VACCINIAL PARANEOPLASTIC NONINLAMMATORY INHERITED: HSP, INHERITED METABOLIC DISORDERS METABOLIC: VIT B12,COPPER,FOLATE ,AIDS ASSOCIATED, VIT E DEFICIENCY TOXIC: CASSAVA, LATHYRISM,FLUOROSIS, SMON, NITROUS OXIDE VASCULAR: ANT SPINAL ARTERY THROMBOSIS, AVM, DURAL AV FISTULA Paraplegia & Spinal cord syndromes Differences between extradural and intradural lesions Extradural Mnemonic – (3 Ps) Pain present - (root pain & spinal tenderness) Pyramidal involvement – early Protein in CSF high Intradural Dissociated anesthesia Bladder involvement early Not so high protein Symmetrical involvement Trophic ulcers common Determining level of lesion in cord compression Sensory level Motor level Reflex level Root pain – dermatome Type of bladder involvement Sensory level – below that level, sensory impairment of loss Motor level – Beevor’s sign indicates T10 lesion Reflex level – Inverted supinator C5 lesion Paraplegia & Spinal cord syndromes Vascular disorders of spinal cord Ischemic disorders of spinal cord Primary ischemia: atherosclerosis/vasculitis Secondary ischemia: SOL, disorders of aorta Decompression sickness Spinal hemorrhage: SAH, SDH, EDH, hematomyelia Spinal AVM/Dural AV fistula Inflammatory disorders spinal cord Acute TM: viral, bacterial, fungal, post-infectious Myelitis of chronic disorders: MS Myelitis of systemic disorders: Behcet’s Medulary compression: Epidural abscess Subdural abscess Spondilodiscitis Paraplegia & Spinal cord syndromes Non-inflamatory spinal space occupying lesions Disc prolapse Neoplasms Non-spinal disorders Acute poliradiculitis Guillain Barre Hyper/Hypokalemic paralysis Parasigital cortical syndromes: Bilateral infarctions Toxic or allergic disorders of spinal cord Subacute-myelo-opticoneuropahty (SMON) caused by clioquinol Late myelopathy after chemonucleolysis Elsberg phenomena: In cervical myelopathy there is first weakness ipsilateral arm, then ipsilateral leg then contralateral leg and lastly contralateral arm. Clinical approach to Spinal cord syndromes What is the onset of paraplegia Is it acute within minutes or hours? Sub-acute within days or weeks? Is it chronic within months or years? Was there a history of trauma? Fall from a Height? Road traffic accident? Direct injury to spine? Clinical approach to Spinal cord syndromes Symmetry of symptoms? Is motor weakness symmetrical? Is sensory symptoms symmetrical? Or they are asymmetrical? Any wasting or fasciculations? Anywhere in the body? Small muscles of the hand? Thigh and gluteal muscles? Clinical approach to Spinal cord syndromes Is there a history of root pains? Is it unilateral or bilateral? Does it radiate to Limbs? Does it aggravate with coughing? Any pyramidal tract involvement? Buckling of knees while walking? Slipping of foot Wear? Tipping on small Objects? Clinical approach to Spinal cord syndromes History of vaccinations? Anti Rabies Vaccination? Polio vaccination? Others? History of increased ICT Fever and headache? Projectile vomiting? Seizures or loss of consciousness? Clinical approach to Spinal cord syndromes What is the nature of neurological deficit? Is it a? Paraplegia? Tetraplegia? Brain stem lesion? Cerebral diplgia? Consider and exclude Guillian Barre Syndrome Clinical approach to Spinal cord What is the mode of onset of paraplegia syndromes Acute within days Transverse myelitis Anterior spinal artery syndrome Traumatic paraplegia Sub-acute 2- 6 weeks Pott’s paraplegia Spinal epidural abscess Spinal cord tumors Chronic ˃ 6weeks Familial spastic paraplegia Amyotrophic lateral sclerosis Cranio-vertebral junction anomalies Legend First-order neuron Lesion Pain stimulus Light touch stimulus Function intact Function lost Second-order neuron Third-order neuron Sensory impairment Lesion of the right dorsal column at L1 produces what impairment? R L Damage to the right dorsal column at L1 causes the absence of light touch, vibration, and position sensation in the right leg. Only fasciculus gracilis exists below T6. R Lesion of the right fasciculus cuneatus at C3 produces what impairment? Damage to the right fasciculus cuneatus at C3 causes the absence of light touch, vibration, and position sensation in the right arm and upper trunk. L Right Fasciculus Cuneatus Lesion DRG R L C3 Fasciculus cuneatus lesion Common causes include MS, penetrating injuries, and compression from tumors. Ipsilateral loss of light touch, vibration, and position sense In the right arm and upper trunk R L Lesion of the right lateral corticospinal tract at L1 produces what impairment? Damage to the right lateral corticospinal tract at L1 causes upper motor neurons signs (weakness or paralysis, hyperreflexia, and hypertonia) in the right leg. Right Lateral Corticospinal Tract Lesion R UMN L L1 Lateral corticospinal tract lesion Common causes include penetrating injuries, lateral compression from tumors, and MS. Ipsilateral UMN signs below the lesion level Weakness (Spastic paralysis) Hyperreflexia (+ Babinski, clonus) Hypertonia Lesion of the right lateral spinothalamic tract at L1 produces what impairment? R L Damage to the right lateral spinothalamic tract at L1 causes the absence of pain and temperature sensation in the left leg. Right Lateral Spinothalamic Tract Lesion DRG R L L1 Common causes include MS, penetrating injuries, and compression from tumors. Lateral spinothalamic tract lesion Contralateral loss of pain and temperature sense Lesion of the anterior gray and white commissures (central cord syndrome) at C5-C6 produces what impairment? R Damage to the anterior gray and white commissures at C5-C6 causes the absence of pain and temperature sensation in the C5 and C6 dermatomes in both upper extremities. L Central Cord Syndrome DRG R L DRG C5-C6 Common causes include posttraumatic contusion and syringomyelia, and intrinsic spinal cord tumors. Lateral Spinothalamic Tract Impaired pain and temperature sensation, C5-C6 dermatomes, bilaterally Postraumatic central cord syndrome MRI of the cervical spine focal posterior disc protrusion at C3/4 level causing spinal stenosis obliterating CSF space and impressing onto the spinal cord. There is increased intramedullary T2 signal without abnormal T1 signal noted Complete transection of the right half the spinal cord (Hemicord or Brown-Sequard syndrome) at L1 produces what impairments? R Damage to the right dorsal columns at L1 causes the absence of light touch, vibration, and position sense in the right leg. Damage to the lateral corticospinal tract causes upper motor neuron signs in the right leg (Monoplegia), and damage to the lateral spinothalamic tract causes the absence of pain and temperature sensation in the left leg. L Hemicord Lesion (Brown-Sequard Syndrome) R L L1 Hemicord lesion Common causes include penetrating injuries, lateral compression from tumors, and MS. Dorsal column lesion Ipsilateral loss of light touch, vibration, and position sense Lateral corticospinal tract lesion Ipsilateral upper motor neurons signs Lateral spinothalamic tract lesion Contralateral loss of pain and temperature sense Hemicord Lesion (Brown-Sequard Syndrome) Cervical spine MRI showing a T2 hyperintense enhancing lesion at C2-3 Complete transection of the spinal cord (Transverse cord lesion) at L1 would produce what impairments? R L Damage to the dorsal columns, bilaterally, causes the absence of light touch, vibration, and position sense in the both legs. Damage to the lateral corticospinal tracts, bilaterally, cause upper motor neuron signs in the both legs (Paraplegia), and damage to the lateral spinothalamic tracts, bilaterally, cause the absence of pain and temperature sensation in the both legs. Transverse Cord Lesion R L Transverse cord lesion Common causes include trauma, tumors, transverse myelitis, and MS. Dorsal column lesion Bilateral loss of light touch, vibration, and position sense Lateral corticospinal tract lesion Bilateral upper motor neurons signs Lateral spinothalamic tract lesion Bilateral loss of pain and temperature sense An MRI showing a Transverse myelitis lesion (the lesion is the lighter, oval shape at center-right), this MRI was taken 3 months after patient recovered Clinical approach to Spinal cord syndromes Clinical features anterior, central, BrownSéquard syndrome Anterior spinal cord syndrome is usually seen as a result of compression of the ASA. Sensory loss is incomplete. Sensitivity to pain and temperature are lost while sensitivity to vibration and position are preserved. Central cord syndrome is results impairment in the arms and hands and to a lesser extent in the legs. Loss of fine control of movements in the arms and hands, relatively less impairment of leg movements. Loss of bladder control may also occur, as well as painful parethesia. Brown-Séquard syndrome is a loss of sensation and motor function (paralysis and anesthesia) that is caused by the lateral hemisection (cutting) of the spinal cord. Complete transection of the lateral corticospinal and lateral spinothalamic tracts with sparing of the dorsal columns, bilaterally, (anterior cord syndrome) in the cervical region would produce what impairments? R Damage to the lateral corticospinal tracts cause upper motor neuron signs, bilaterally, below the lesion level. Damage to lower motor neurons in the ventral horns cause lower motor neuron signs, bilaterally, at the lesion level. Damage to the lateral spinothalamic tracts cause absence of pain and temperature sensation, bilaterally, below the lesion level. Sparing of the dorsal columns leaves light touch, vibration, and position sense intact throughout. L Anterior Cord Syndrome UMN UMN DRG DRG R L Anterior cord lesion Common causes include anterior spinal artery infarct, trauma, and MS. Lateral corticospinal tract lesion Ipsilateral upper motor neurons signs Lateral spinothalamic tract lesion Contralateral loss of pain and temperature sense Anterior Cord Syndrome Left: hyperintense intramedullary lesion in T2 at the level C3-C7 (arrows), indicate acute cervical spinal cord infarction. Right: MR sagittal T2: myelomalacia cavity C3-C7 in control after a month. Posterior Cord Syndrome DRG DRG R Common causes include trauma, compression from posteriorly located tumors, and MS. L Dorsal column lesion (bilateral) Bilateral loss of light touch, vibration, and position sense, generalized below lesion level Posterior Cord Syndrome Complete transection of the dorsal columns, bilaterally, (posterior cord syndrome) in the cervical region would produce what impairments? R L Damage to the dorsal columns (fasciculus gracilis and cuneatus), bilaterally, causes the absence of light touch, vibration, and position sense, bilaterally, from the neck down (below the lesion level).