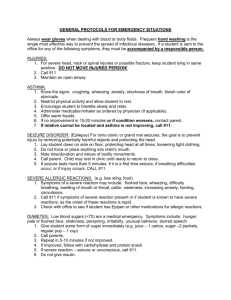
Seizures
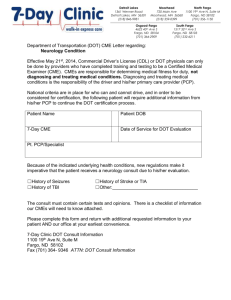
advertisement

CNS Disorders EMS Professions Temple College Pathophysiology of CNS Emergencies Structural Changes Often due to Trauma but not always Circulatory Changes Alterations of ICP Response to insult Toxic Metabolic states Inadequate Perfusion Alteration to blood chemistry or introduction of toxins Psychiatric ‘mimicking’ ICP Review CBF is a factor of CPP & CVR CPP = MAP - ICP If CPP , then CBF If CVR , then CBF most likely MAP = Diastolic + 1/3 PP PP = SBP - DBP PCO2 has greatest effect on CVR Sympathomimetics may CVR ICP Review As PCO2 , CVR Therefore, if PCO2 , CVR Then, as CVR , CBF Normal ICP < 15 mm Hg As ICP , CPP then CBF Compensation for ICP via MAP Cushing’s Reflex (Triad) Cushing’s triad with coma indicates possible herniation Altered Mental Status Coma A decreased state of consciousness from which a patient cannot be aroused Mechanisms Structural lesions Toxic Metabolic states Psychiatric ‘mimicking’ Brain injury Recall that Brain injury is often shown by: Altered Mental Status Seizures Localizing signs Is unconsciousness itself an immediate life threat? YES, IT IS! Loss of airway Vomiting, aspiration Altered Mental State Manage ABC’s Before Investigating Cause! Initial Assessment/Management Airway Breathing Open, clear, maintain If trauma or + history, control C-spine Presence? Adequacy (rate, tidal volume)? High concentration O2 on ALL patients with altered mental status Assist ventilations prn Circulation Pulses? Adequate Perfusion? Investigate Cause DERM D = Depth of Coma E = Eyes R = Respiratory Pattern M = Motor Function D = Depth of Coma What does patient respond to? How does he respond? Avoid use of non-specific terms like “stuporous”, “semi-conscious”, “lethargic”, “obtunded” D = Depth of Coma AVPU Glasgow Scale (later) Describe level of consciousness in terms of reproducible findings E = Eyes Pupils Size - mid, dilated or constricted measurement - e.g. 4 mm Shape - round, oval, pontine Equality - equal in size Symmetry - equal in reaction/response Response to light Yes or No How? R = Respiratory Pattern Depth Unusually deep or shallow? Pattern Regular or Unusual pattern Can you identify the pattern? M = Motor Function Paralysis? Muscle tone? Where? What is it like? Posturing? Rigid or Flaccid Movement? Where? How? Symmetrical Motor Function? Physical Exam Vital Signs Shock? Increased ICP? Hypoxia/Hypercarbia Diagnostics Dysrhythmias? Blood glucose Oxygen saturation Physical Exam Detailed (Head-to-Toe) Exam Injuries causing coma? Injuries caused by coma? Clues to the cause Probable Causes of AMS Not enough Oxygen Not enough Sugar Not enough blood flow to deliver oxygen, sugar Direct brain injury Structural Metabolic Differentiating AMS Causes Structural Asymmetrical deficits Unequal pupils Afebrile History of trauma, structural abnormality Often a rapid onset Metabolic Symmetrical deficits Equal pupils (? altered function) ? Fever History of metabolic disorder or illness Rapid onset less likely Management Maintain ABCs Attempt to identify cause Mainstays of therapy Oxygenation/Ventilation IV fluids appropriate for the patient D50 (if hypoglycemic) Narcan if possibility of opiate OD Flumazenil in known benzo only OD AEIOU TIPS Alcohol Epilepsy Insulin Overdose Uremia (Metabolic causes) Trauma Infection Psychogenic Stroke/Syncope Cerebrovascular Accident AEIOU TIPS Cerebrovascular Accident Any disease process that disrupts blood flow to a distinct region of the brain Transient Ischemic Attack (TIA) S/S less than 24 hours without permanent neuro deficits Cerebrovascular Accident 500,000/yr in US 25% die Survivors often socially, financially devastated $20 billion in medical costs, lost wages Cerebrovascular Accident (CVA) Pathophysiology Thrombosis (brain itself) Embolus (head, neck or heart) Hemorrhage (within brain) Ischemia (systemic blood flow) Predisposing Factors: Modifiable Hypertension Chronic atrial fibrillation Cigarette smoking Diabetes Mellitus Sickle cell disease Polycythemia Heart disease Hypercoagulability Hyperlipidemia Birth control pill use Cardiovascular disease Cocaine use Predisposing Factors: Unmodifiable Age Gender Race Prior stroke Heredity CVA Mechanisms Ischemic stroke--80 to 85% Hemorrhagic stroke--15 to 20% CVA Origin Thrombus Embolus Aneurysm Arrhythmia Hypovolemia Ischemic Stroke Blood vessel occlusion Thrombosis Embolism Plaque fragments from carotids Chronic atrial fibrillation Fat particles IV substance abuse particulates Systemic hypoperfusion Pump failure Hypovolemia Ischemic Stroke Syndromes Transient Ischemic Attack (TIA) Neurological deficits that resolve in 24 hours or less (most in 30 minutes) Commonly result from carotid artery disease Same symptoms as CVA Often warning sign of impeding CVA 5% risk of stroke per year Ischemic Stroke Syndromes Dominant Hemisphere Infarction Contralateral weakness, numbness Contralateral blurring of vision of half the visual field in both eyes Difficulty pronouncing words (dysarthria) Difficulty speaking or understanding speech (dysphasia or aphasia) Ischemic Stroke Syndromes Nondominant Hemisphere Infarction Contralateral weakness, numbness Contralateral visual field cut Neglect of contralateral extremities Constructional apraxia (difficulty drawing figures like a clock face) Dysarthria Usually NOT dysphasic or aphasic Ischemic Stroke Syndromes Vertebrobasilar Syndrome Involves blood flow to brainstem, cerebellum, and visual cortex Dizziness, vertigo Diplopia Dysphagia Ataxia, bilateral limb weakness Hemorrhagic Stroke 30 to 50% 30-day mortality Younger patient population Two subtypes: Intracerebral, usually 2o to hypertension Subarachnoid, usually from berry aneurysms Hemorrhagic Stroke Syndromes Intracerebral Hemorrhage Headache, nausea, vomiting precede deficits Patients commonly have decreased LOC with extreme hypertension Contralateral hemiplegia, hemianesthesia Possible aphasia, extremity neglect depending on hemisphere involved Hemorrhagic Stroke Syndromes Subarachnoid Hemorrhage Grade I Grade II Grade III Grade IV Grade V Asymptomatic or mild headache and mild nuchal rigidity Moderate to severe headache, nuchal rigidity, cranial nerve dysfunction but no other deficits Drowsiness, confusion, mild focal deficits Stupor, moderate to severe hemiparesis, possibly early decerebrate rigidity, vegetative response Deep coma, decerebrate rigidity, moribund appearance CVA Assessment Presentation of CVA varies with area(s) of brain involved and type of CVA CVA Presentation Brain can show injury in only three ways: Decreased LOC Seizures Localizing signs Hemiparesis or hemiplegia Dysphasia (Receptive or expressive) Visual disturbances Gait disturbances Inappropriate affect Bizarre behavior Incontinence Cincinnati Prehospital Stroke Scale Have patient smile (“Facial Droop”) Have patient close eyes and hold arms out (“Arm Drift”) Normal: Both sides of face move equally well Abnormal: One side does not move as well as other Normal: Both arms drift same amount or do not drift Abnormal: One arm does not drift or one drifts down compared to other or can’t move arms Have patient say, “You can’t teach an old dog new tricks.” (“Speech”) Normal: Correct words, no slurring Abnormal: Slurs words, uses inappropriate words, or unable to speak Assessment Signs & Symptoms Ischemic S&S usually of slower onset Hemiparesis or hemiplegia Numbness or decreased sensation of face or unilateral Altered LOC or coma Convulsions Visual disturbances Slurred or inappropriate speech Headache or dizziness Assessment Signs & Symptoms Cerebral Embolus with rapid onset Emboli from valvular HD or Afib rapid onset Often with an identifiable cause (e.g. Afib, Valvular heart disease, recent long bone fracture) Assessment Signs & Symptoms Cerebral hemorrhage associated with rapid onset high mortality rate Often with severe HA (“Worst headache ever”) N/V Rapid decrease in LOC or seizure Coma, Cushing’s and Herniation History Associated Altered LOC or Seizure? Onset/Precipitating factors? Initial symptoms and progression? Assessment Dizziness, Severe HA, N/V Previous CVA or TIA? Previous neuro deficits? Concomitant illnesses? Sickle Cell Disease Atrial fibrillation Risk factors for stroke & thrombus formation? BCP, Smoking HTN, CVD Assessment Physical Exam Mental Status & Behavior Extremity Motor & Sensory Gait Pupils & Vision Cincinnati Prehospital Stroke Scale Evidence of Cushing’s or Herniation Blood glucose level CVA Management Basic Objective Improve cerebral blood flow and oxygenation CVA Management Airway If no gag reflex, intubate Otherwise, position to ensure drainage of secretions Suction prn Breathing Oxygen via NRB Ventilate with BVM and O2 if rate or tidal volume inadequate Intubate if herniating CVA Management Controlled hyperventilation if intracranial hemorrhage suspected with increased ICP and neurologic deterioration Indicators Sudden onset Headache Rapid loss of consciousness Seizures Unequal pupils CVA Management Circulation Check blood glucose level Hypoglycemia may mimic CVA Treat hypoglycemia with D50 Establish IV Access Draw blood samples TKO avoid solutions with glucose Monitor ECG 10% of CVAs are associated with cardiac event 12 Lead ECG if suspected ischemia CVA Management Do not assume patient cannot understand because they cannot talk Position appropriately: If hypertensive, semireclined (head slightly elevated) If normotensive, on affected side If hypotensive, supine CVA Management Increased Blood pressure treated ONLY if strongly suggestive of ischemic stroke If systolic >220 or diastolic >120 consider gradual blood pressure reduction Labetalol Nitropaste Nitroprusside Controlled reduction Return to pre-CVA levels, NOT to “normal” CVA Management Thrombolytic agents Consider for all patients with ischemic CVA presenting within 3 hours of onset Early recognition of ischemic stroke and administration of thrombolytics can prevent/limit loss of neurologic function Requires CT scan!!! CVA Management Think like AMI of the Brain Time is tissue Therapy Mainstays Oxygenation/Ventilation IV Access Rapid assessment & differential Treat associated conditions (hypoglycemia, hypoxia, hypotension) Rapid Transport to appropriate facility CT Scan & Thrombolytics vs. CT Scan & Neurosurgery Syncope AEIOU TIPS Syncope aka Fainting Pathophysiology Brief loss of consciousness caused by transient cerebral hypoxia May be caused by lack of glucose or seizure activity in the brain Syncope Types Postural Inadequate blood flow to brain due to position Vasovagal Excessive vagal stimulation Carotid Sinus stimulation/pressure Cardiogenic Dysrhythmia, usually bradycardia Stokes-Adams Syndrome Syncope Types Tussive “coughing spell” resulting in intrathoracic pressure causing venous return to the heart most often in overweight male smokers with chronic bronchitis Micturation associated with urination, usually in patients who have consumed EtOH and compounded by increased vagal stimulation Syncope Assessment History of the event Often preceded by sensation of light-headedness Rapid return of consciousness is most common Past History History of vertigo Similar past episodes Many possible causes Syncope Management Manage ABCs Clear airway and Assist ventilations as needed Oxygen NRB (initially) Calm & Reassure Assess for underlying cause ECG Blood glucose History (present and past) Physical Exam Treatment based on underlying cause Seizures AEIOU TIPS Seizures Alteration in behavior/consciousness 2° unstable, uncoordinated electrical activity in the brain Often a result of altered membrane permeability Manifested by sudden, brief episodes of: altered consciousness altered motor activity altered sensory phenomena unusual behavior Seizure Categories Generalized Tonic-Clonic (grand mal) AKA Absence (petit mal) Partial Convulsions Simple partial Complex partial Hysterical Seizure Etiology CVA Hypoxia Infection/Fever Drug/alcohol withdrawal Poisoning/OD Thyrotoxicosis Head trauma Hypoglycemia Brain neoplasms Psychiatric disorders Eclampsia Hypocalcemia Seizures Etiology Most epileptic seizures are idiopathic in origin Generalized Seizures Petit Mal Absence Sz Children No LOC Grand mal aka Convulsions Common Often w/Aura Sudden LOC Tonic / Clonic Postictal phase Status epilepticus Generalized Seizures Symmetrical No local onset Irritable focus difficult to identify Near simultaneous activation of entire cortex Focus may begin deep in brain and spread outward Generalized Seizures Tonic-Clonic Seizures (Grand Mal) Aura (preictal phase) Loss of consciousness/postural tone Tonic phase Hypertonic (tetanic) phase Clonic phase Post-ictal phase May experience transient neurologic deficits (Todd’s paralysis) Generalized Seizures Absence Seizure (Petit Mal) Brief loss of awareness (10 - 30 seconds) Usually no loss of postural tone May occur 100+ times a day Primarily pediatric problem Often described as “daydreaming”, not paying attention Usually disappear as child matures Partial Seizures Seizure begins locally May remain localized or spread to entire cortex Result from focal structural lesion in brain Partial Seizures Simple Localized clonic activity Abnormal sensory symptoms Usually no LOC May progress Jacksonian (Seizure) March Complex Change in behavior Preceded by aura Repetitive motor behavior No recall May progress Partial Seizures Simple partial seizures (No loss of consciousness) Focal motor seizures Local clonic activity May display Jacksonian march Sensory seizures Autonomic seizures Partial Seizures Complex partial seizure (psychomotor or temporal lobe seizures) Distinctive aura Loss of consciousness Automatisms May be mistaken for drunks or psychotics May experience episodes of rage Hysterical “Seizures” Usually in front of audience Usually follow interpersonal stress Movements asymmetrical or purposeful Does not fall, hit head, bite tongue Incontinence rare Recalls things said, done during “seizure” Assessment Seizure Assessment Duration Seizure Postictal phase Typical for the patient? Onset Events before HA Aura Trauma Vision Disturbances Assessment Recent History Trauma to the head/brain HA / Neck Pain Pregnancy Brain tumor Recent Infection/Illness CVA Symptoms Introduction of Poisons into body Assessment Past History Diabetes Mellitus Seizure Disorder Tumor CVA Medications Recreational Drug Use Alcohol abuse Assessment Physical Exam Evidence of trauma Evidence of alcohol, drug abuse Rash, stiff neck Pregnant CVA Signs Incontinence Status Epilepticus Two or more seizures without intervening conscious period Usually due to medication noncompliance Management same as for other Seizures just more aggressive Seizure Management Patient actively seizing Do NOT restrain Do NOT put anything in mouth Oxygen NRB if possible ECG Monitor when possible IV Access Lg Bore, NS Assess blood glucose Seizure Management Patient actively seizing If hypoglycemic: Assess IV patency FIRST!! Dextrose 50% 12.5 - 25 grams IV push Consider Thiamine 100 mg slow IV push Diazepam, slow IV administration until seizure stops or until ~ 10 mg Usually aimed at 2.5 mg doses, one after another Phenobarbital, 100 mg/min IV push to a total ~390 mg or seizure stops Barbiturate coma NMB & Intubation Seizure Management Current Mainstays of Therapy for Actively Seizing Patient “New” Therapy Diazepam Lorazepam Phenobarbital Phosphenytoin Other Considerations Glucose MgSO4 Paraldehyde Dilantin (phenytoin) 18mg/kg at 25 mg/min Seizure Management After seizure stops: Open -Clear- Maintain airway O2 via NRB Assist ventilations if needed Roll patient onto side protecting head Reassess ABCDs Assess blood glucose Physical Exam and History Most seizure deaths are due to anoxia Seizure Management If the patient is epileptic, do these seizures match what is “normal” for him? Just because the patient is epileptic, he does NOT have to be having an epileptic seizure! Mandatory Transports First time seizures Seizure patient off medications Change in seizure pattern Associated with trauma Pregnant patient Status epilepticus Associated with increased body temperature Not always; Seldom in young children Has infection been diagnosed and treatment initiated? Insulin: Hypo/Hyperglycemia AEIOU TIPS Insulin Hypoglycemia Hyperglycemia DKA HHNC Insulin Assessment Medical Alert Tag/Bracelet Evidence of DM Medications Fruity breath odor Signs of repeated SQ injections Blood glucose level (See Endocrine for further assessment) Insulin Management Hypoglycemia Management ABCs: Oxygen/IV/ECG Dextrose 50% (adult), 12.5 - 25 grams IV push via patent line Consider Thiamine 100 mg slow IV push Dextrose 25% (children), 0.5 - 1 grams IV push (2-4 cc/kg) via patent line Carbohydrate meal Assess for underlying cause Consider transport Insulin Management DKA/HHNC Management ABCs: Oxygen/IV/ECG Ventilate/Intubate prn Fluid administration titrated to signs of shock 250 cc boluses and reassess Consider administration of Regular Insulin (consult medical control) Assess for underlying cause Transport Alcohol AEIOU TIPS Alcohol EtOH present in up to 40% of AMS patients “Dead drunk” Mixed overdose May be associated with Head trauma Hypoglycemia Alcohol Is it alcohol or is it something else? A patient is never “Just Drunk” Alcohol Management Manage ABCs Clear airway and ventilate as needed Oxygen IV access prn Assess for other causes of AMS ECG Monitor Blood glucose level History of mixed poisoning or EtOH poisoning Physical exam Treat other causes Overdose/Poisoning AEIOU TIPS Overdose/Poisoning Possible Overdose/Poisonings resulting in AMS Alcohol: Ethanol/Methanol Narcotics Sedative-hypnotics Solvent inhalation Stimulants Overdose Assessment Needle marks? Pupil responses? Slow respirations? Associated hypotension Odd behavior? Breath odors? Color of oral mucosa, vomitus? History of Recent Drug/Poison use? Uremia/Metabolic Causes AEIOU TIPS Uremia (Metabolic Causes) Uremia/Renal Failure Hyperthyroidism Hypothyroidism Addisonian Crisis Hepatic Coma/Encephalopathy Uremia (Metabolic Causes) Assessment Med Alert? Patient medications? Physical findings? The Physical Exam and History (recent and past) are most useful Trauma AEIOU TIPS Trauma Concussion Cerebral contusion Intracranial hematoma Hypovolemia Hypoxia Trauma Assessment Physical findings? Evidence of brain injury History of recent or remote trauma? Trauma Altered Mental Status = Head Injury Until Proven Otherwise Trauma Head injury severity cannot be evaluated accurately in presence of shock Trauma Management Manage ABCs Spinal motion restriction if indicated Clear airway and secure prn Ventilate prn Oxygen Establish IV access, NS Fluid to titrate BP to ~ 90 mm Hg systolic Assess for other causes: ECG, Blood glucose Transport to trauma center Infection/Fever AEIOU TIPS Infection Meningitis Encephalitis Brain abscess Sepsis Fever Infection Assessment Headache? Fever? Sore throat? Stiff neck (nuchal rigidity)? Rash? Associated symptoms of systemic infection Infection Management Infection Control Measures Manage ABCs clear airway and ventilate prn oxygen IV access prn Consider acetaminophen for fever fluid / rehydration Psychogenic AEIOU TIPS Psychogenic Hysterical faking Catatonia “psychomotor disturbances characterized by physical rigidity, negativism, or stupor” may occur in schizophrenia, mood disorders or organic mental disorders Psychogenic Assessment Circumstances? Events Prior behavior? Similar leading up to this point past episodes Medications & PMHx Assessment & Management of AMS Primary Assessment Onset Level of Consciousness Mechanism (Kinematics) Preceding S/S AVPU GCS (later) Airway obstruction or compromise Fluid Unprotected airway (e.g. coma) Primary Assessment Ventilatory ability Adequate Ventilatory rate and depth? Respiratory Insufficiency 2° to ICP? (e.g. irregular patterns) Cardiovascular compromise Shock /hypotension /hypovolemia Hypertension Primary Assessment Neuro Exam (motor & sensory) Posturing? Muscle Tone? Pupillary Reflexes? Extraocular Movements? Symmetry History Present and Recent Past Management of AMS Goals: Airway control/ maintenance Avoid Cardiovascular stabilization Avoid hypotension/shock Interruption of cerebral injury Fix hypoxia the root cause problem Protection from further harm Avoid secondary brain injury Other Neurologic Conditions Headache Common complaint Characteristics Many persons experience regularly ~ 1/3 due to migraine HA May be associated with significant pathology Sudden vs Constant vs Recurring Generalized vs Localized Mild to Moderate to Severe Intensity of Pain Cause is often unknown Headache Vascular Migraines Last minutes to hours to days Usually very intense, throbbing pain Photosensitivity N/V Often unilateral May be preceded by aura (not common) Occur commonly in women Headache Vascular Cluster Series of headaches Usually last for a few minutes or a few hours Sudden, intense pain Usually unilateral May be accompanied by nasal congestion, irritated or watery eye (same side) Occur commonly in men Headache Tension Most common headache Occur regularly Often awake in a.m. and worsens throughout the day Dull, ache Feels like pressure on neck and/or head Headache Organic Not very common Due to some specific cause (illness/injury) in the body Tumor Infection Meningitis Hypoglycemia etc. Headache Potentially Serious Pathologies Complaint “Worst headache ever” “It hurts right here” May localize at posterior neck at base of skull Possible subarachnoid hemorrhage Concern for possible intracranial hemorrhage Neoplasms Less common neoplasm Risk factors genetic exposure to radiation tobacco use occupational exposure to toxins medications/drugs/poisons diet Neoplasms Pathophysiology Most often a result of metastasis from another cancer (malignant) Assessment focused on the detailed neuro exam not a diagnosis diagnosis BUT should be included in the differential dx Muscular Dystrophy Genetic disorder Results in degeneration of muscle fibers Types Duchenne Fascioscapulohumeral Limb Girdle Myotonic Muscular Dystrophy Duchenne dystrophy most common childhood muscular dystrophy onset usually by age 6 symmetrical weakness and wasting of first the pelvic and leg muscles then pectoral and proximal upper extremities progresses and results in early death usually in adolescence Multiple Sclerosis Common demyelinating disorder of the CNS Results in patches of sclerosis (patches) in brain and SC Occurs primarily in young adults Typical S/S visual loss, diplopia nystagmus weakness, paresthesias symptoms may have periods of exacerbation and remission Parkinson’s Disease Degenerative changes in the basal ganglia result in deficiency of dopamine Characterized by rhythmical muscular tremors, rigidity of movement, and droopy posture Usually occurs after 40 years of age Leading cause of neuro disability > 60 years Estimated 500,000 in US Central Pain Syndrome Known as Trigeminal Neuralgia paroxysmal bursts of pain in one or more branches of the trigeminal nerve Often induced by touching trigger points in or about the mouth Causes tumor some medications (phenothiazines) Bell’s Palsy Paresis or paralysis of the facial muscles usually unilateral Occurs in 23 of 100,000 persons Caused by dysfunction of the 7th cranial nerve cause is usually a viral infection other causes post trauma herpes simplex lyme disease idiopathic Amyotrophic Lateral Sclerosis Progressive motor neuron disease aka ALS or Lou Gehrig disease disease of the motor tracts of the lateral columns and anterior horns of the SC results in progressive muscular atrophy, increased reflexes, and spastic irritability of muscles Spina Bifida An embryolgic failure of fusion of one or more vertebral arches results in spinal cord exposure spinal cord may protrude outward various types based upon type of deformity Child requires frequent surgeries increased risk of latex allergies Poliomyelitis An inflammatory process of the Spinal Cord’s gray matter May be caused by the poliomyelitis virus Enters bloodstream and nervous system results in paralysis of the limbs Uncommon today in the US due to polio vaccine