Anaphylaxis
advertisement

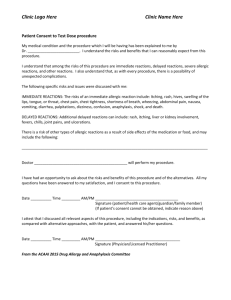
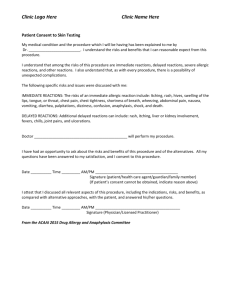
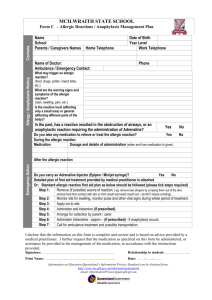
Allergic Reactions & Anaphylaxis MARCH 30, 2012 PCP Adapted From EMS Professions Temple College Anaphylaxis is an immediate, systemic, life-threatening allergic reaction. Prompt recognition and appropriate drug therapy in the prehospital phase are crucial to patient survival. Today’s Objectives Epidemiology Review the patho of an Allergy & Anaphylaxis Review the mechanism injury Review the sign & symptoms Review the Principles of Management PCP Anaphylaxis Protocol Recall the use of Epinephrine Recall the procedure for administering SC injection Other Protocols that may used in conjunction with the Anaphylaxis protocol Demonstrate the assessment & management of an Anaphylaxis Practice Simulations Incidence In North America- 400 to 800 deaths/year Parenterally administered penicillin accounts for 100 to 500 deaths per year Insect stings (bees) account for 40 to 100 deaths per year Risk factors: beta-blockers, adrenal insufficiency Causes of Deaths Laryngeal edema and acute bronchospasm with respiratory failure account for >70% Circulatory collapse accounts for 25% Other <5% - ?brain ?MI Allergic Reaction Physiologic response to antigens – Oversensitive response = allergic – Occurs after sensitization to antigen Antigen binds with Antibody – Less severe result in inflammatory response – Type I reaction involves antibodies attached to mast cells or basophils = most severe form Anaphylaxis Systemic reaction of multiple organ systems to antigen-induced IgE-mediated immunulogic mediator release in previously sensitized individual An event that can lead to death Allergic Rx – Induces Antibody Formation Anaphylaxis Antigens enter body by: – – – – Injection Ingestion Inhalation Absorption Anaphylaxis Pathophysiology Antigen enters body & Antibodies produced Attach to surface of mast or basophil cells Mast cells become sensitized Anaphylaxis Pathophysiology Mast cells – In all subcutaneous/submucosal tissues, – Including conjunctiva, upper/lower respiratory tracts, and gut Basophils – Circulate in blood Mast Cells Blasting Anaphylaxis Pathophysiology Antigen reenters body Attaches to antibodies on mast or basophil cells Mast cell degranulates, releases – – – – Histamine Leukotrienes Slow reacting substance of anaphylaxis (SRS-A) Eosinophil chemotactic factor (ECF) Where Do Things Go Histamine Three histamine receptor types: – H1 – H2 – H3 Histamine Acts on H1 receptors to cause – Smooth muscle contraction – Increased vascular permeability – Prostaglandin generation Histamine Acts on H2 receptors to cause – – – – – Increased vascular permeability Gastric acid secretion Stimulation of suppressor lymphocytes Decreased PMN enzyme release Release of more histamine from mast cells and basophils Histamine Acts on H3 receptors to cause – Inhibition of central, peripheral nervous system neurotransmitter release – Inhibition of further histamine formation, release Vasodilation Decreased peripheral vascular resistance Hypotension Tachycardia Peripheral hypoperfusion Increased Capillary Permeability Tissue edema, urticaria (hives), itching Laryngeal edema – Airway obstruction – Respiratory distress – Stridor Fluid leakage from vascular space – Hypovolemic shock Urticaria Describe What You See Describe What You See Describe What You See Describe What You See Describe What You See Smooth Muscle Spasm Bronchospasm – Respiratory distress – “Tight Chest” – Wheezing GI Tract Spasm – Nausea, vomiting – Cramping, diarrhea Bladder Spasm – Urinary urgency – Urinary incontinence Anaphylactic Reaction Leukotrienes – Potent bronchoconstrictors, vascular permeability & possibly coronary vasoconstriction – Slower onset than histamine – Effects last longer than histamine Allergic Reactions Generally classified into 3 groups: – Mild allergic reaction – Moderate allergic reaction – Severe allergic reaction (anaphylaxis) Mild Allergic Reaction Characteristics – – – – – – Urticaria (hives), itchy Erythema (redness) Rhinitis Conjunctivitis Mild bronchoconstriction Usually localized (look on abdomen, chest, back) No SOB or hypotension/hypoperfusion Often self-treated at home Moderate Allergic Reaction Characteristics – Mild signs/symptoms with any of following: » Dyspnea, possibly with wheezes » Angioneurotic edema » Systemic, not localized No hypotension/hypoperfusion Severe Allergic Reaction (Anaphylaxis) Characteristics – Mild and/or moderate signs/symptoms plus – Shock / hypoperfusion Clinical Manifestation Dependent on: – – – – Degree of hypersensitivity Quantity, route, rate of antigen exposure Pattern of mediator release Target organ sensitivity and responsiveness Clinical Manifestation Severity varies from mild to fatal Most reactions are respiratory, dermatologic Less severe early findings may progress to lifethreatening over a short time Initial signs/symptoms do NOT necessarily correlate with severity, progression, duration of response Generally, quicker symptoms = more severe reactions Clinical Manifestation First manifestations involve skin – Warmth and tingling of the face, mouth, upper chest, palms and/or soles, or site of exposure – Erythema – Pruritus is universal feature, erythema – May be accompanied by generalized flushing, urticaria, nonpruritic angioedema Clinical Manifestation May progress to involvement of respiratory system – – – – – – – cough chest tightness dyspnea wheezing throat tightness dysphagia hoarseness Clinical Manifestation Other Signs and Symptoms – lightheadedness or syncope caused by hypotension or dysrhythmia – nasal congestion and sneezing – ocular itching and tearing – cramping abdominal pain with nausea,vomiting, or diarrhea – bowel or bladder incontinence – decreased level of consciousness Clinical Manifestation Physical Exam findings may include – urticaria, angioedema, rhinitis, conjunctivitis – tachypnea, tachycardia, hypotension – laryngeal stridor, hypersalivation, hoarseness, angioedema Insect Sting Hypersensitivity Hymenoptera - yellow jackets, honeybees, hornets, wasps, bumble bees 90%: Local hives, pruritus 10%: Massive local reaction, including swelling beyond two joints of extremity 1%: Systemic reaction 10%: have worse reaction on second sting 28%: have recurrent systemic reaction Management Treatment depends upon severity of reaction and signs/symptoms of its presentation Epinephrine Treatment of Choice for Anaphylaxis – No absolute contraindications in anaphylaxis Route IM, SC, IV – – – – – – Sympathomimetic Relaxes smooth muscle in the airways (Beta) Peripheral vascular constricting (Alpha) Counteracts histamine and other cytokines Raises blood sugar level Raises heart rate, blood pressure, and myocardial oxygen demand S/A – Tremors, anxiety, headache, palpitations Peak 1 to 2 minutes to a duration of 5 to 10 min Benadryl Second Treatment of Choice for Anaphylaxis – Route PO, IM, IV – – – – – Antihistine H1 receptor antagonist Counteracts histamine and other cytokines Blocks histamine activity at receptor site Raises heart rate, blood pressure, and myocardial oxygen demand S/A – Drowsiness, dizziness, dryness of mouth, nervousness, nausea Peak < 1 hour ½ life 2.4 to 9.3 hours Management Optimal management requires – – – – – High index of suspicion (suspect, treat within minutes) Early diagnosis Pharmaceutical intervention Observation Disposition Patient Self-Management Benadryl (Diphenhydramine ) 50 mg PO At any sign of anaphylaxis, self-administer subcutaneous epinephrine (Epi-Pen®, AnaKit®) Mild Allergic Reaction Often self-treated at home High Flow Oxygen Base line vitals Diphenhydramine 25 - 50mg PO or IM – IV is reasonable but should include transport If stinger present, flick it away with credit card or fingernail Anticipate crisis Moderate to Severe Allergic or Anaphylaxis Reaction High flow oxygen Base line vitals IV NS ( Patient > 12 yrs – Maintenance Rate – Bolus BP < 90 mm Hg ECG monitor Diphenhydramine 25-50 mg PO* Transport Contact EP if unstable *6-11 years 25 mg Diphenhydramine *2-5 years 12.5 mg Diphenhydramine Differential DX Presentation Differential diagnosis Hypotension Septic shock Vasovagal reaction Cardiogenic shock Hypovolemic shock Respiratory distress with wheezing or stridor Airway foreign body Asthma and chronic obstructive pulmonary disease exacerbation Vocal chord dysfunction syndrome Differential Dx Postprandial collapse Airway foreign body Monosodium glutamate ingestion Sulfite ingestion Scombroid fish poisoning Flush syndrome Carcinoid Postmenopausal hot flushes Red man syndrome (vancomycin [Vancocin]) Miscellaneous Panic attacks Systemic mastocytosis Hereditary angioedema Leukemia with excess histamine production Case Presentation #1 You are dispatched to an electronics manufacturing plant to see a 28-year-old woman. The woman believes she is having an allergic reaction. Security officers will meet you at the front gate and escort you to the patient. What specific information would you like at this point? Case Presentation #1 You find this patient in an office area sitting at her desk. From a distance, you notice she is awake and speaking clearly. She does not appear to have any breathing difficulty. She states she had just returned from lunch and began to feel hot and light headed. Her friend pointed out that the patient’s arms and neck are very red, and that her face appears “puffy”. Case Presentation #1 The patient states she is allergic to peanuts but has not eaten any. She went to a health food café where she had grilled chicken and steamed vegetables. She has no other past history and takes no medications. Her last allergic rx was similar to this. Vitals are: BP-116/70; Pulse-100; RR-20; Lung sounds-clear and equal. No difficulty swallowing, redness to her arms, chest, neck and face. Would you like to perform any other procedures/exams/testing or obtain other history before treating? Case Presentation #1 So, what is your complete treatment plan for this patient?