Anatomy and Physiology of the Eyelids and Adnexa Layers of eyelid

Orbit, Lid and Lacrimal disorders
Dr Mahmood Fauzi Ansari
ASSIST PROF OPHTHALMOLOGY
AL MAAREFA COLLEGE
Objectives
• Review the clinical anatomy and physiology of Eyelids and
Adenexa
• Describe disorders of eyelids (infections, malposition, tumors and congenital conditions)
• Describe disorders of lacrimal system (obstruction ,infection)
• Enumerate causes and management of Epiphora and Dry eye
• Outline Diagnosis and management of orbital infection
• Compare between pre-septal and septal cellulitis
• Develop the Differential diagnoses of Orbital Inflammatory
Disease
Anatomy
The orbit
Function
• protection to the globe
• attachments which stabilize the ocular movement;
• transmission of nerves and blood vessels.
The orbit
The orbit
The orbit
Clinical features of orbital disease
• Eyelid and conjunctival changes
• Reduced visual acuity
• Pain
• Proptosis
• Enophthalmos
• Diplopia
Proptosis (exopthalmos)
• Protrusion of the eye caused by a space-occupying lesion
• Measured with an exophthalmometer.
• 3 mm difference between the two eyes is significant.
• Direction of proptosis
• Transient proptosis (orbital varices)
• Fast onset proptosis (malignant, inflammatory)
• Slow onset proptosis (benign)
• Pain associated with proptosis ( orbital cellulitis)
Thyroid ophthalmopathy
Pathogenesis
• Disorders of the thyroid gland can be associated with an infiltration of the extraocular muscles with lymphocytes and the deposition of
Glycosaminoglycans.
• An immunological process is suspected but not fully determined.
Clinical features
• Proptosis (most common cause in adults)
• Lid retraction
(characteristic stare)
• Lid lag
• Double vision
• Red painful eye
(exposure)
• Reduced visual acuity
(optic nerve)
Grading system for thyroid associated ophthalmopathy
Pneumonic
NO SPECS
N : no signs
O : only sign = upper lid retraction; Dalrymple
S : soft tissue involvement (edema, chemosis, lagophthalmos)
P : proptosis
E : EOM involvement
C : corneal involvement (SPK)
S : sight loss (optic nerve compression)
Thyroid Eye Disease
Thyroid ophthalmopathy
Thyroid ophthalmopathy
• Treatment of associated ocular emergencies
(optic nerve compression and corneal exposure)
1- systemic steroid
2- radiotherapy
3- orbital decompression
4- heavy lubrication
• Long term treatment
Only after stabilization, muscle and lid surgery
Diplopia (Muscle pathology
)
Thyroid ophthalmopathy (Graves’ ophthalmopathy)
Idiopathic Orbital Inflammatory Disease( orbital pseudotumor)
Enophthalmos
• Congenital (small eye)
• After trauma ( blow out fracture)
Orbital tumors
• Lacrimal gland tumors
• Optic nerve gliomas
• Meningiomas
• Lymphomas
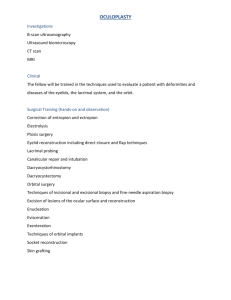
• Rhabdomyosarcoma (most common orbital malignancy in childhood)
• Metastasis from other systemic cancers
(neuroblastomas in children, the breast,
Lung, prostate or gastrointestinal tract in the adult).
The orbital septum
The orbital septum is the fascia behind that portion of the orbicularis muscle that lies between the orbital rim and the tarsus; it serves as a barrier between the lid and the orbit. The superior orbital septum blends with the tendon of the levator palpabrae superioris and the superior tarsus; the inferior orbital septum blends with the inferior tarsus.
Disorders of the Orbit- infections
• Pre-septal Cellulitis (Periorbital cellulitis)
• Post-septal Cellulitis (Orbital cellulitis)
Orbital cellulitis
ORBITAL INFLAMMATORY
DISEASE(OID)
• Idiopathic/non specific orbital inflammatory disease
inflammation of the orbital tissues of unknown cause resulting in orbital pain, diplopia and proptosis
• Orbital myositis inflammation of extraocular muscles, most commonly the superior or lateral rectus, causing orbital pain on movement of affected muscles, diplopia, proptosis
• Dacryoadenitis - inflammation of the lacrimal gland causing painful swollen lacrimal gland and reduced tear production; may be isolated or as part of diffuse idiopathic orbital inflammatory disease
• Wegener's granulomatosis - systemic small-vessel vasculitis characterised by necrotising granulomatous inflammation; c-ANCA positive in most cases; ocular involvement can include conjunctivitis, episcleritis, uveitis, retinal artery occlusion, nasolacrimal duct occlusion and optic nerve vasculitis.
The differential diagnosis of OID includes infection, inflammation, and tumor.
(a) Orbital cellulitis in patient who presented with acute onset orbital inflammation post-foreign body.
(b) Idiopathic OID in patient who presented with acute onset of orbital inflammation.
(c) Thyroid orbitopathy in patient who presented with a several months history of increasing proptosis.
(d) Tumour in region of the lacrimal gland, note S-shaped ptosis.
The main supporting structure of the eyelids is a dense fibrous tissue layer, called the tarsal plate . The palpebral conjunctiva is the mucous membrane which adheres firmly to the tarsal plates and lines the posterior eyelids.
The sensory nerve supply to the eyelids is derived from the first and second divisions of the trigeminal nerve (V).
The blood supply to the lids is derived from the lacrimal and ophthalmic arteries by their lateral and medial palpebral branches.
Anatomy and Physiology of the Eyelids and Adnexa
The eyelids are composed of several layers of tissue which protect the anterior eyeball.
From superficial to deep, they are the skin layer, a layer of striated muscle (orbicularis oculi), areolar tissue, fibrous tissue (tarsal plates), and a layer of mucous membrane
(palpebral conjunctiva).
Layers of eyelid
Muscles of eyelids
The lid margins are divided into the anterior and posterior margins at the mucocutaneous junction.
Glands of Zeis and glands of Moll are both found on the anterior margin.
Glands of Zeis are small, modified sebaceous glands that open into the hair follicles at the base of the eyelashes; whereas glands of Moll are modified sweat glands that open in a row near the base of the eyelashes.
The posterior lid margin is in close contact with the globe, and along this margin are the small orifices of modified sebaceous glands, called meibomian glands.
Summary of Eyelid Pathology
Disorders of the Eyelids
• EYELID INFECTIONS
• Blepharitis: Inflammation of lid margins
Anterior blepharitis
Posterior Blepharitis
•
Involving the meibomian gland orifices (meibomitis)
•
Associated with acne rosacea
•
Symptoms: similiar to anterior blepharitis
•
Signs: thickening and telangiectasia of lid margins, decreased tear break-up time, rosacea
•
Management
•
Lid massage after heat
•
Topical antibiotics/steroids
•
Tear film supplements
•
Systemic tetracyclines in persistent or severe cases
LID LUMPS
Anterior Lamella
•
External hordeolum (stye) - acute abscess within lash follicle and its associated glands of
Moll or Zeis
•
Signs: tender, warm, swollen, red eyelid lump
•
Management warm compression, topical antibiotic; add oral antibiotic in preseptal cellulitis
• Cyst of Moll - translucent cyst arises from blockage of gland of Moll (apocrine sweat gland)
•
Cyst of Zeis - poorly translucent cyst arises from blockage of gland of Zeis (modified sebaceous gland)
•
Xanthelasma - deposition of lipids within perivascular xanthoid cells which may be idiopathic or associated with hyperlipidaemia, hypothyroidism or primary biliary cirrhosis.
Posterior Lamella
•
Internal hordeolum - acute abscess within a meibomian gland resulting in tender lump with inflammation
•
Usually caused by Staphylococcus aureus
•
Management - warm compression, oral antibiotics in preseptal cellulitis
•
Chalazion - chronic lipogranulomatous inflammation of blocked meibomian glands.
•
Often evolving from an internal hordeolum
•
Common in patients with chronic marginal blepharitis, rosacea, seborrhoeic dermatitis.
•
Management - small chalazion tends to resolve itself; persistent and symptomatic chalazion can be surgically removed by incision and curettage.
EYELID MALPOSITION
•
Ectropion Abnormal eversion of eyelid (usually the lower) away from the globe
•
Entropion Abnormal inversion of eyelid (usually lower) towards the globe
•
Ptosis - Abnormally low position of the upper lid
•
Horner's Syndrome
(ptosis+meiosis+anhydrosis+enopthalmos)
Ectropion
• Abnormal eversion of eyelid (usually the lower) away from the globe Congenital - rare
• Paralytic - due to orbicularis weakness secondary to seventh cranial nerve palsy
• Involutional - due to age-related tissue laxity
• Cicatricial - due to shortened anterior lamella resulting from scarring
• Mechanical
• Management
• Lubricants and artificial tears
• Taping lower and upper eyelids together overnight
• Corrective surgery
• Congenital - rare
Entropion
• Acute spastic - caused by sustained eyelid orbicularis contraction secondary to ocular irritation
• Involutional - due to inferior refractor dysfunction/tissue laxity
• Cicatricial - due to shortened posterior lamella resulting from scarring
• Management
• Taping eyelid to the cheek
• Botulinum injection
• Corrective surgery
Ptosis
• Involutional/aponeurotic ptosis –
• most common form of ptosis; arises from disinsertion, dehiscence or attenuation of levator palpebrae superioris
• Neurogenic ptosis third nerve palsy (dilated pupil, inability to elevate and adduct the globe), Horner's syndrome (constricted pupil; partial ptosis due to weakness of Muller's muscle)
• Myasthenic ptosis - Myasthenia gravis (fatiguable ptosis)
• Myopathic ptosis - chronic progressive external ophthalmoplegia, myotonic dystrophy
• Mechanical ptosis - masses, infiltration, oedema of upper lid
• Dermatochalasis (a form of pseudoptosis) - excess skin of upper lids
• Management
• Conservative
• Surgery - depending on the amount and type of ptosis, degree of levator function. There are three main approaches including
• anterior (transcutaneous/external)
• posterior (transconjunctival/internal)
• brow/frontalis suspension surgery
Viral Infections
Varicella zoster –
• Widespread vesicular rash, primarily affecting the head neck and trunk.
• Reactivation of virus gives rise to shingles
Herpes zoster ophthalmicus (shingles)
• Occurring in the first division of the trigeminal nerve
• Characteristic unilateral maculopapular rash,
• Associated with marked pain and systemic malaise (1 week prior to the development of the rash)
• Common in older patient .
• Hutchinson's sign: cutaneous involvement of the tip of the nose suggests an increased likelihood of ocular complications).
• Treatment
• Systemic Antivirals (eg famciclovir )
• Management of lid involves cool compresses and topical lubrication ± topical antibiotics for secondary infections
Herpes simplex
• primary infection is usually not clinically apparent unless occurring in the neonate or when associated with immunodeficiency.
• Secondary infection frequently manifests as a dendritic corneal ulcer
Malignant tumours
Basal cell carcinoma
(rodent ulcer)
• >90% of all neoplastic eye lesions
• Frequently occurs on the lower lid
• Indurated Plaque ± Lid distortion and Lash Abnormalities.
• Treatment is with wide local excision.
Is Basal Cell Carcinoma Serious? …Yes, Basal Cell Carcinoma can kill if left untreated .
Sebaceous Gland Carcinoma
• accounts for 5% of all malignant eyelid tumors. can originate from Meibomian glands, Zeis glands or the sebaceous glands of the caruncle.
• more common in the upper eyelid
Squamous cell carcinoma
• accounts for ~2-5% of lid malignancies
•
The tumour tends to occur on the lower lid at the margin,
• commonly in fair-skinned elderly people with a history of sun exposure.
•
Plaque-like (rough, scaly erythematous patch), nodular or ulcerating with a sharply defined base and everting borders.
•
It can be aggressive: refer early if you suspect this.
Congenital disorders of the lid
•
Epicanthic folds vertical folds of skin extending from the upper eyelids to the side of the nose
These are NORMAL features in
Orientals.
•
Coloboma
uncommon condition of a partial or full thickness defect of the lid
-associated with systemic conditions such as
Treacher Collins' syndrome.
-Treatment is surgical.
•
Cryptophthalmos
–
• failure of lid development
The lacrimal system
The lacrimal drainage system
Disorders of the Lacrimal System
•
CONGENITAL OBSTRUCTION OF THE
NASOLACRIMAL SYSTEM
•
Nasolacrimal duct obstruction
•
Dacryocystocele
•
INFECTIONS OF THE LACRIMAL
SYSTEM
•
Canaliculitis :
•
Acute Dacryocystitis :
NLD obstruction
Congenital NLD obstruction
• 5% of all full-term newborns.
• 90% open spontaneously in the first year of life.
• Tx: massage and antibiotics drops if infected.
• Sometimes need probing and tubing
Adult NLD obstruction
Dacryocystitis
Nasolacrimal duct obstruction, right eye. Note the build-up of tears and mucous along the lower lid margin.
Congenital dacryocystocele of the lacrimal sac in a newborn baby. A dacryocystocele is located just inferior to the medial canthus and presents as a purplish or greyish-blue swelling.
The lacrimal puncta, canaliculi, and sac, and the nasolacrimal duct form the drainage system, ultimately draining into the nose.
The nose is lined by a highly vascular mucosal epithelium; consequently, topically applied medications that pass through this nasolacrimal system have direct access to the systemic circulation.
Valve-like folds of the epithelial lining of the duct, called the valve of
Hasner tend to resist the retrograde flow of tears and air. When the structure is imperforate, it is the most common cause of congenital nasolacrimal duct obstruction, resulting in epiphora and chronic dacryocystitis
The lacrimal apparatus consists of the lacrimal gland, accessory lacrimal gland, lacrimal puncta, lacrimal canaliculi, lacrimal sac and nasolacrimal duct.
These structures are involved in the production and drainage of tears.
The blood supply of the lacrimal gland is derived from the lacrimal artery. The lymphatic drainage drain into the pre-auricular lymph nodes.
The nerve supply of the lacrimal gland is by the lacrimal nerve (sensory), a branch of the trigeminal first division, the great petrosal nerve (parasympathetic secretory), which comes from the superior salivary nucleus and is a branch of the facial nerve; and sympathetic nerves accompanying the lacrimal artery and the lacrimal nerve.
Any abnormality of one of the three layers produces an unstable tear film and the symptoms of dry eyes.
A tear Layer frequently affected is the Aqueous Layer, Resulting in Aqueous Tear Deficiency (ATD) or lacrimal hyposecretion.
Epiphora- watery eyes
A tearing eye may be a nuisance but usually is not a serious
• Common causes of watery eyes include:
• Blepharitis(eyelid inflammation)
• Blocked tear duct
• Common cold
• Ectropion (outwardly turned eyelid)
• Entropion (inwardly turned eyelid)
problem.
Successful management of the tearing patient requires the clinician to determine the underlying cause of the epiphora.
• Foreign object in the eye
• Hay fever
• Infection of the tear duct
• Ingrown eyelash (trichiasis)
• Irritation of the cornea (front of the eye)
• conjunctivitis
• Trachoma
• some times, dry eye can be a contributing factor
Medications that can cause watery eyes include:
• Epinephrine , Chemotherapy drugs, Cholinergic agonists, Eyedrops, especially echothiophate iodide (Phospholine Iodide) and pilocarpine
• Managing the ‘Tearing’ patient
• Dilation,
• punctoplasty,
• silicone intubation
Dry eye
• Dry eye syndrome can occur if your eyes do not produce enough tears or your tears evaporate too quickly
• Symptoms of dry eye :
• Pain ,Light sensitivity, A gritty sensation, A feeling of a foreign body or sand in the eye,Itching,Redness
• Blurring of vision (Without tear film, good vision not possible.)
• What Causes Dry Eyes?
• The natural aging process, especially menopause
• Side effects of certain drugs such as antihistamines and birth control pills
• Diseases that affect the ability to make tears, such as Sjogren's syndrome, rheumatoid arthritis, and collagen vascular diseases
• Structural problems with the eyelids that don't allow them to close properly
• Managing the dry eye
• Artificial tear drops and ointments.
• Temporary punctal occlusion
• Lipiflow. use heat and pressure on the eyelids to unclog blocked glands.
• Restasis.
(Cyclosporine Ophthalmic Emulsion) 0.05% increases eyes’ natural ability to produce tears, in Chronic Dry Eye. RESTASIS® did not increase tear production in patients using anti-inflammatory eye drops or tear duct plugs
Useful Resources
• Diagnosis and Management of Eyelids and
Lacrimal Abnormalities. http://www.optometry.co.uk/uploads/articles/a9a941
1f4103e999dd58c633a30329bd_Wearne1991105.pdf
• External Eye Overview - Lashes, eyelids and lacrimal system. http://www.patient.co.uk/doctor/External-Eye-
Lashes-Eyelids-and-Lacrimal-System.htm
• Eyelids, Orbit and Lacrimal System. http://www.slideshare.net/sectionbmd/lecture2eyelidorbitlacrimal
• http://quizlet.com/37218591/flashcards