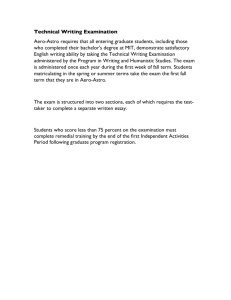
Pelvic examination
advertisement

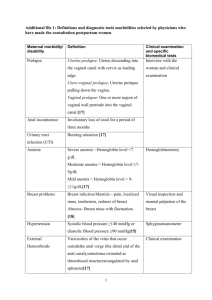
Obstetrics and Gynecological History and Physical examination Chao Gu M.D., Ph.D. Dept of Ob/Gyn OB/GYN Hospital, Fudan University Medical history collecting and writing (30 min) Pelvic examination (15 min) Test (30 min) Good communication is necessary for the assessment of patient's condition and treatment communication technique • concentration • Knowledge • Kindness • Humor? Trust Gynecologic History • • • • • • • • General Item Chief Complaint Present Medical History Past Medical History Menstruation History Marriage History Social History Family History Gynecologic Physical Examination • • • General exam Abdominal exam Pelvic exam-- Gynecology examination Assistant Checkup • • Ordinary test Special test Physical Examination • Symptoms • General check up • Abdomen examination • Pelvic examination –Gynecology exam General Item Name, Gender, age, nationality, marriage, occupation, hometown Address, time of hospitalization, history collecting time, history provider Chief Complaint The main symptoms or The duration of symptoms (Professional term, in 20 words) •12 weeks menopause, vaginal bleeding for two days, abdominal pain for one hour •Uterine fibroids found for one month in Gynecological checkup •G2P0 pregnancy 37 +6 weeks, bloody show for 3 hours History of Present Illness • Chronology of chief complaint from when the patient first felt well until the present • Detailed description of the chief complaint --occur, evolution, diagnosis and treatment procedures History of Present Illness Pain Bleeding • Location • Onset and Duration • Timing (onset, duration and frequency) • Constant or Intermittent • Quality (characteristics) • Character • Quantity or Severity • Intensity • Setting • Alleviating or Precipitating factors History of Present Illness Vaginal Discharge • Duration • Characteristics • Associated Symptoms • Temporally Related Events Past Medical History • Medical illnesses (childhood and adult) • Immunizations • Surgical history • Infectious diseases history • Medications • Allergies • blood transfusion history Menstruation History 5 12 50 28 • Age of menarche, menstrual cycle,volume, associated symptoms, LMP/PMP, amenorrhea, menopausal age date • LMP:Last menstrual period • PMP:Previous menstrual period The female patient, 27 years old, complaint in August menstruation was late, and previous menstrual date was on July 16th. Menarche occurred in junior high, normally 2 days ahead of each period, much volume in first 2 days, less after, accompanied by mild back pain. Marriage History • marriage history (times of marriage, age of marriage) • health condition for husband • history of giving birth: Full-term-Premature birth-Abortion-Survival 2-0-1-2 • G2P1:pregnancy 2, birth 1 • birth control mesures Personal Information History Birth place, previous location bad habits for cigarette and alcohol Family History Parents cousins,sibling Health conditions children • Any inheritable disorders • Special attention to breast, ovarian and colon cancer • Osteoporosis, heart disease and menopause Obstetric History Past obstetric history • Outcome of previous pregnancies in details including the abortions • Any significant antenatal, intrapartum or postpartum events • Previous maternal complications • Mode of delivery • Baby weight • Life & Health of the baby Abdominal exam • Inspection • Ascultation • Palpation • Percussion Discussion 1 Please write a complaint according to the following information: • Female patient, 42 years old, complaint in recent 1 years by the increased amount of menses, accompanying a backache with fatigue • Female patient, 35 years old, lower abdominal pain for 2 days recent one month, and leucorrhea has peculiar smell Discussion 2 Please according to the following data to write present medical condition, to see what is needed for history collection: • At the age of 28, amenorrhea for 2 months, irregular vaginal bleeding • 40 years old, the vulva pruritus, leucorrhea is abnormal • At the age of 26, 7+ months of pregnancy, vaginal bleeding Medical history collecting and writing Pelvic examination Basic Requirements of the Pelvic Examination • Check carefully, gentle movement • Urine evacuated before check ( urine preserved for checkup ) • Replace the one-time pad • Bladder lithotomy position Q: To avoid the menstrual period, what should you do before check, if check is must while bleeding? • Male doctor to check best with female physician presence to avoid unnecessary misunderstanding Step 1 Vulval inspection •Vulva development and its hair distribution •New biological, skin lesion vulva •Vaginal vestibule •Hymen •The vagina mouth •Vaginal wall and uterine prolapse or not Step 2 Check up by speculum • Speculum forbidden without agreement by virgin • replacement and removal Step 3 Vaginal inspection deformity: vaginal septum, double vagina new biological, ulcer, cyst or not Vaginal discharge is normal, if necessary, check leucorrhea routine Step 4 Cervical inspection Size, color, mouth shape bleeding, erosion, gland cyst, polyps Cervical tube has hemorrhages or exudates or not Cervical smear Cervical scraping smear Step 5 Bimanual examination Check with two fingers or one finger into the vagina, while the other hand in the abdomen to help checking Vaginal, cervical, endometrial, attachment, palace and pelvic wall Step 6 Trimanual examination Rectal, vaginal, abdominal examination Rectal - abdominal diagnosis index finger into the rectum, with the other hand in the abdomen helping check Asexual life history, vaginal atresia or other reasons can not be performed bimanual examination. Check up Record The vulva: development, production type. Vaginal: Patency, mucosa, secretions Cervical: size, hardness, erosion, contact bleeding, lifting pain Uterine body: location, size, texture, motion, tenderness Bilateral accessory: mass, size, texture, motion, tenderness, and relationship between uterus and pelvic wall Gynecological examination evaluation standard ( out of 100 points ) 1 Examination of vulva (5 points) 2 Speculum removal (5 points) 3 Speculum with lubricant (5points) 4Speculum two leaf close up (5 pints) 5Along the posterior wall to insert vagina speculum into the vagina, gradually flattening, open two leaves, gentle action ( 10 points) 6 Exposure of the vaginal wall, cervical and fornix ( 10 points) •Examination of the vaginal wall mucosa color, elastic •The amount of vaginal discharge, character, color, smell •Cervical size, mouth shape, erosion and polyps or not Gynecological examination evaluation standard ( out of 100 points ) 7 Speculum removal (5 points) 8 Wearing sterile gloves ( 5 points) 9 The index finger, middle finger stick lubricant ( 5 points) 10 Examination of vaginal, cervical, posterior fornix ( 15 points) 11 Bimanual examination ( 20 points) 12 The finger out of the vagina, disposable gloves, the patient is asked to get dressed ( 10 points) Gynecological examination evaluation standard ( out of 20 points ) The end Thank you !