Digestion notes (updated 12/2)
advertisement

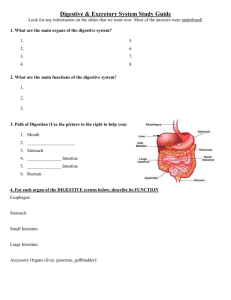
Human Physiology: Digestion Topic 6.1, 11.3 Option H2, H3, H4 3 Dietary Categories Herbivores – Cattle, gorillas, snails, and sea urchins, – eat autotrophs (plants and algae) Carnivores – Lions, hawks, spiders, and snakes – Ingest other animals Omnivores – Crows, cockroaches, raccoons, and humans – Ingest both plants and animals How do animals obtain and ingest their food? Suspension feeders – Extract food particles suspended in the surrounding water – Ex. Clams and oysters Substrate feeders – Live on or in their food source and eat their way through it. Ex. Caterpillars and earthworms Fluid feeders – Obtain food by sucking nutrient nutrient-rich fluids from a living host, either a plant or an animal. Ex. Mosquitoes and ticks Bulk feeders – Ingest relatively large pieces of food – Ex. most animals Overview: Food processing 1. Four stages Ingestion 2. Digestion 3. Absorption 4. Elimination undigested material passes out of the digestive tract The act of eating The breaking down of food into molecules small enough for the body to absorb. Two phases: 1. Breaking food down mechanically (teethchewing) into smaller pieces 2. hydrolysis, chemical breakdown, catalyzed by enzymes Cells lining the digestive tract take up (absorb) the products of digestion—small molecules such as amino acids and simple sugars Nutrients travel through blood to cells, where they are made into macromolecules or further broken down for energy General compartments for digestion Food vacuoles are the simplest digestive compartments. – Phagocytosis: cell engulfs food particle, which then fuses with a lysosome. Most animals have an alimentary canal, a digestive tube with two openings, a mouth and an anus. – Allows food to move in one direction, with specialized regions in the digestive tube that carry out digestion and absorption of nutrients in sequence General compartments for digestion Food entering the mouth usually passes into: – A pharynx, or throat – Then passes into the esophagus – Passed to stomach, muscular and churns and grinds food – Chemical digestion and nutrient absorption occur mainly in the intestine – Undigested materials are expelled though the anus. Human Digestive Tract Main parts of human alimentary canal: – Mouth, oral cavity, tongue, pharynx, esophagus, stomach, small intestine, large intestine, rectum, and anus. Main digestive glands – Salivary glands, pancreas, and liver – Secrete digestive juices that enter the alimentary canal through ducts. – Secretions from liver are stored in gallbladder before they are released into the intestine. Human Digestive Tract Peristalsis – Rhythmic waves of contractions of smooth muscles in the walls of the digestive tract – Once food is swallowed, peristalsis propels it through the alimentary canal. – In only 5-10 seconds, food passes from the pharynx down the esophagus and into the stomach. – Pyloric sphincter, a muscular ringlike valve, keeps food in the stomach by regulating the pass of food into the small intestive. Works like a drawstring, closing off the tube and keeping food in the stomach long enough for stomach acids and enzymes to begin digestion. http://nutrition.jbpub.com/resources/animations.cfm?id=1&d ebug=0 Human Digestive Tract Final steps of digestion and nutrient absorption occur in the small intestine over a period of 5-6 hours. Undigested material moves slowly through the large intestine (taking 12-24 hours), and feces are expelled through the anus. Digestion Begins in the Oral Cavity Saliva is produced by the salivary glands through ducts to the oral cavity even before you eat; it’s a response to presence of food Sight or smell of food causes nerve stimulation In a typical day, salivary glands secrete more than a liter of saliva Digestion Begins in the Oral Cavity Saliva contains several substances necessary for food processing – Slippery glycoproteins Protects the soft lining of the mouth and lubricates food for easier swallowing – Buffers Neutralize food acids, helping prevent tooth decay. – Antibacterial agents Kill many of the bacteria that enter the mouth with food. – Salivary amylase Digestive enzyme that begins hydrolyzing food Digestion Begins in the Oral Cavity Oral Cavity – Mechanical and chemical digestion begins in the oral cavity. – Chewing cuts, smashes, and grinds food, making it easier to swallow and exposing more food surface to digestive enzymes – Teeth and tongue are prominent Teeth grind and crush food Tongue, muscular organ with taste buds, allows you to taste your meal and manipulates food and helps shape it into a ball called a bolus. – In swallowing, it pushed the bolus to the back of the oral cavity and into the pharynx. PharynxSwallowing Pharynx has openings for both the esophagus and the trachea (wind-pipe) Most of the time, esophageal opening is closed and air enters the trachea and proceeds to the lungs. When you eat: – a bolus of food enters the pharynx, triggering the swallowing reflex – The esophageal sphincter relaxes and allows the bolus to enter the esophagus – Larynx (voice box) moves upwards and tips the epliglottis over the tracheal opening. – Epiglottis prevents food from passing into the trachea. – After the bolus enters the esophagus, the larynx moves downward, the epiglottis moves up again, and breathing passage reopens – Esphogas sphincter contracts above the bolus. Esophagus: Peristalsis Esophagus is a muscular tube that conveys food boluses from the pharynx to the stomach. Muscles at the very top of esophagus are under voluntary control; thus, the act of swallowing begins voluntarily. Then, Involuntary waves of contraction by smooth muscles in the rest of the esophagus take over. Esophagus: Peristalsis As food is swallowed, muscles above the bolus contract, pushing the bolus downward Simultaneously, muscles around the bolus relax, allowing the passageway to open. Muscle contractions continue in waves until the bolus enters the stomach. Waves of smooth muscle contraction also move materials through small and large intestine Stomach: stores and breaks down food Stomachs are the main reason we do not have to eat constantly Highly elastic and can stretch to accommodate about 2 Liters of food and drink, usually enough to satisfy our body’s needs for many hours. Some digestion occurs in the stomach. The stomach secrete gastric juice: – made up of mucus, enzymes, and strong acid. – Functions to break apart the cells in food – Also kills most bacteria and other microbes that are swallowed with food. Stomach: stores and breaks down food Stomach wall is highly folded, and has pits that lead to tubular gastric glands. Three types of cells that secrete different components of the gastric juice: – Mucous cells: secrete mucous, which lubricates and protects the cells lining the stomach – Parietal cells: secrete HCl acid – Chief cells: secrete pepsinogen, an inactive form of the enzyme pepsin Stomach: stores and breaks down food Pepsinogen, HCl, and pepsin: – 1. Pepsinogen and HCl are secreted into the lumen (cavity) of the stomach. – 2. HCl converts pepsinogen to pepsin. – 3.Pepsin then activates more pepsinogen, starting a chain reaction. Pepsin begins the chemical digestion of proteins. Proteins will be further digested in small intestine. Stomach: stores and breaks down food Prevention of gastric juice from digesting away stomach lining: – Secreting pepsin in the inactive form of pepsinogen helps protect the cells of the gastric glands – mucus helps protect the stomach lining from both pepsin and acid. – Still, epithelium is constantly eroded; enough new cells are generated by mitosis to replace the stomach lining completely about every three days. Stomach: stores and breaks down food Gastric glands are regulated by a combination of nerve signals and hormones: – When you see, smell, or taste food, a signal from your brain to your stomach stimulates your gastric glands to secrete gastric juice. – Once food is in your stomach, substances in the food stimulate cells in the stomach wall to release the hormone gastrin in the circulatory system. – Gastrin circulates in the blood stream, returning to the stomach wall, stimulating further secretion of gastric juice. – As much as 3L of gastric juice may be secreted a day. – A negative-feedback mechanism inhibits secretion of gastric juice when the stomach contents become too acidic. Acid inhibits the release of gastrin, and with less gastrin in the blood, the gastric glands secrete less gastric juice. Stomach: stores and breaks down food About every 20 seconds, the stomach contents are mixed by the churning action of muscle in the stomach wall and result in acid chyme. Opening between the esophagus and the stomach is usually closed until a bolus arrives. Backflow of acid chyme causes heartburn (which should be called esophagus-burn) – Can also cause acid-reflux (gastroesophageal reflux disease; GERD) Stomach: stores and breaks down food Pyloric sphincter helps regulate the passage of acid chyme from the stomach into the small intestine. The stomach takes about 2-6 hours to empty after a meal; acid chyme leaves stomach only a squirt at a time. Acid chyme rich in fats stimulates the small intestine to release a hormone that slows the emptying of the stomach, providing more time for digestion. Other hormones secreted by the small intestine influence the release of digestive juices from the pancreas and gall bladder. Gastric Ulcers Gastric Ulcers: – Open sores that form when mucus, which normally protects the stomach wall from the corrosive effect of digestive juice, fails to protect it. Small intestine and esophagus are also susceptible to ulcers – Symptoms are usually gnawing pain in the upper abdomen, which may occur a few hours after eating. – Were formerly thought to result from the production of too much pepsin/and or acid or too little mucus: For years, the blame was put on factors that cause these effects, such as aspirin, ibuprofen, smoking, alcohol, coffee, and stress However, strong evidence now points to… H. pylori – – – – – – – – – Gastric Ulcers A spiral-shaped bacteria Low pH of the stomach kills most microbes, but not this one! Burrows beneath mucus and releases harmful chemicals Growth seems to result in a localized loss of protective mucus and damage to the cells lining the stomach WBC fight infection, causing mild inflammation of the stomach, called gastritis. Gastric ulcers form when pepsin and HCl destroy cells faster than the cell can regenerate from the H. pylori attack. Eventually, stomach will erode to the pint where it actually has a hole in it, which can lead to a life threatening infection in abdomen or internal bleeding. 70-90% of ulcer and gastritis sufferers have this bacterial infection Also found in 30% of healthy people. linked to certain kinds of stomach cancer Gastric Ulcers Treatment – Usually respond to a combination of antibiotics and bismuth (the active ingredients of Pepto-Bismol) which eliminates bacteria and promotes healing. – Drugs that reduce stomach acidity may also help, and researchers are working on preventitive treatment for H.Pylori. Small Intestine Once at the S.I., food has been mechanically reduced to smaller pieces and mixed with juices; it now resembles a thick soup. Starch digestion began in the mouth, and protein breakdown began in the stomach. All other chemical digestion occurs in the s.i. Nutrients are also absorbed into the blood from the s.i. Length of over 6m, making it the longest organ of the alimentary canal. Diameter is only about 2cm, which is why it’s called the “small” intestine. Small Intestine Contributing to digestion in s.i. are two large glandular organs: pancreas and liver. Pancreas: – Produces pancreatic juice a mixture of digestive enzymes and an alkaline solution rich in bicarbonate Alkaline solution neutralizes acid chyme as it enters the small intestine Small Intestine Liver – Performs a wide variety of functions, including the production of bile: Contains bile salts that emulsify fats, making them more susceptible to attack by digestive enzymes. Gall bladder stores bile until it is needed in the small intestine. Small Intestine First 25 cm or so of the s.i. is called the duodenum. – Where acid chyme squirted from the stomach mixes with bile from the gall bladder, pancreatic juice from the pancreas, and digestive enzymes from gland cells in the in the intestinal wall. Small Intestine All four types of macromolecules (carbohydrates, proteins, nucleic acids, and fats) are digested. Refer to table 21.11 on pg. 438 Small Intestine Carbohydrate digestion: – Begins in the oral cavity and is completed in the s.i. – Pancreatic amylase hydrolyzes starch (a polysaccharide) into the disaccharide maltose – Maltose is then hydrolyzed into glucose via maltase. – Sucrase hydrolyzes table sugar and lactase digests milk sugar (lactose) Small Intestine Protein digestion: – S.i. completes protein digestion from the stomach – Pancreas and duodenum secrete hydrolytic enzymes that completely dismantle polypeptides into amino acids. dipeptidase – Hydrolyzes fragments only two or three amino acids long. trypsin and chymotripsin – Break polypeptides into smaller polypeptides – Trypsinogen (in pancreas) is converted into trypsin by the action of enteropeptidase (the enzyme that is bound to the membranes of the small intestine). aminopeptidase and carboxypeptidase – Split off one amino acid at a time, working from both ends of a polypeptide. Small Intestine Nucleic acid digestion: – Nucleases hydrolyzes the nucleic acids in food. From the pancreas Split DNA and RNA (which are present in the cells of food items) into their component nucleotides, which are then broken down into nitrogenous bases, sugars, and phosphates by other enzymes produced by the duodenal cells. Small Intestine Fat digestion: – Most fat remains undigested until it reaches the duodenum. – Hydrolysis of fats is problematic due to fats insolubility in water. Emulsification= Problem Solved!!! Bile salts in bile cause fat globules to be physically broken up into smaller fat droplets, a process called emulsification. Many small droplets allows for a larger surface area of fat exposed to lipase, an enzyme that breaks fat molecules down into fatty acids and glycerol. Small Intestine Problems with lipid digestion in a hydrophillic medium: – Lipids tend to coalesce (lump together) and are only accessible to lipase at the lipid-water interface. – Bile molecules have a hydrophobic end and a hydrophilic end which emulsifies (prevents from coalescing) the lipids – Lipase must be water-soluble and has a hydrophobic active site (for its substrate, lipids) – The increased surface area allows lipase greater access to its substrate Small Intestine By the time persistalsis has moved the mixture of chyme and digestive juices through the duodenum, chemical digestion of your meal is just about complete. Main function of the rest of the small intestine is the absorption of nutrients and water. Small Intestine Structurally, great for nutrient absorption. – Lining has a huge surface area– roughly 300 m2, about the size of a tennis court – Extensive surface area results from several kinds of folds and projections. Villi: large circular folds with numerous, small fingerlike projections around the inner wall of the s.i. Microvilli: many tiny surface projections found on epithelial cells lining a villus. – extend into the lumen of the intestine and greatly increase the surface area across which nutrients are absorbed. Small Intestine Some nutrients are absorbed via simple diffusion; other nutrients are pumped against concentration gradients into the epithelial cells The core of each villus is penetrated by a small lymph vessel and a network of capillaries. – After fatty acids and glycerol are absorbed by an epithelial cell, these building blocks are recombined into fats and are transported into the lymph vessel. – Amino acids and sugars pass out of the intestinal epithelium and then across the thin walls of the capillaries into the blood. Small Intestine Capillaries that drain nutrients away from the villi converge into larger veins and eventually into a main vessel, the hepatic portal vein, that leads directly to the liver: – Liver gets first access to nutrients absorbed from a meal – Converts many nutrients into new substances that the body needs. – One of its main functions is to remove excess glucose from the blood and convert it to glycogen, which is stored in liver cells. – From the liver, blood travels to the heart, which pumps the blood and the nutrients it contains to all parts of the body. Small Intestine Structural features of an epithelial cell of a villus: Villi – provide a huge surface area for absorption Epithelium cells – single layer of small cells, packed with mitochondria – the source of ATP (metabolic energy) for active uptake across the plasma membrane Pump proteins in the plasma membrane of epithelium cells – actively transport nutrients across the plasma membrane into the villi Network of capillaries – large surface area for uptake of amino acids, monosaccharides, and fatty acids and glycerol into blood circulation Lacteal – branch of the lymphatic system into which triglycerides (combined with protein) pass for transport to body cells Mucus from goblet cells in epithelium – lubricates movement of digested food among the villi and protects plasma membrane of epithelial cells Microvilli – these tiny, finger-like infoldings of the cell surface facing the lumen of the gut greatly increase the surface area in contact with material to be absorbed. Mitochondria – these organelles are present in large numbers, suggesting a significant demand for ATP in these cells. Pinocytotic vesicles – these are the site of pinocytosis by which fluid is taken up or released in tiny vesicles, across the plasma membrane of a cell. Tight junctions – these bind together the individual epithelial cells, so that the only way into the tissues of the body is through the epithelium. Small Intestine Small Intestine Mechanisms used by Ileum to absorb and transport food: Facilitated diffusion. Some substances need a little assistance to enter and exit cells. The transmembrane protein helps out by changing shape. Active transport. Some substances need a lot of assistance to enter cells. Similar to swimming upstream, energy is needed for the substance to penetrate against an unfavorable concentration gradient. Endocytosis. Cells can use their cell membranes to engulf a particle and bring it inside the cell. The engulfing portion of the membrane separates from the cell wall and encases the particle in a vesicle. Small Intestine Material not absorbed and are egested: – cellulose and lignin from plant matter – the remains of intestinal epithelial cells – bile pigments – bacteria Small Intestine Absorption vs. Assimilation: – Absorption involves the passage of digested nutrients into the blood from the gastro-intestinal tract, glucose, fructose and amino acids go straight to the blood capillaries, whereas fatty acids and monoglycerides so first into the lymphatic system and then the blood system. Assimilation involves the integration of these absorbed molecules into the living processes of the organism that ingested them, using them to build new molecules that are necessary for its normal functioning and survival. Or using them to produce energy Large Intestine Also known as the colon 1.5 m long and 5 cm in diameter It joins the small intestine at a T-shaped junction, where a sphincter controls the passage of unabsorbed food material out of the small intestine. – One arm of the T is a blind pouch called the cecum. A small, fingerlike extension of the cecum is the appendix: contains a mass of w.b.c’s that make a minor contribution to immunity. Large Intestine Main function is to absorb water from the alimentary canal. About 7L of fluid enters the lumen of the digestive tract each day as the solvent of the various digestive juices. About 90% of this water is absorbed back into the blood and tissue fluids, with the small intestine reclaiming most of it and the colon finishing the job. Large Intestine As water gets absorbed, remains of the digested food become more solid as they are moved along the colon via peristalsis. Remains make feces, the waste products of digestion, which consist mainly of indigestible plant fibers Large Intestine Surprise, surprise! – Bacteria, such as E.coli, live in your colon! – Produce important vitamins (biotin, folic acid, B vitamins, and Vitamin K) that are absorbed into the bloodstream through the colon Large Intestine Rectum: terminal portion of the colon where feces are stored until they can be eliminated. Strong contractions of the colon create the urge to defecate. Two rectal sphincters, one voluntary and one involuntary, regulate the opening of the anus. Diarrhea Large Intestine – If the lining of the colon is irritated by a viral or bacterial infection, the colon is less effective in reclaiming water Constipation – Peristalsis moves the feces along too slowly; the colon reabsorbs too much water, and the feces become too compacted. – Usually caused by a diet with not enough fiber or from a lack of exercise. Digestion Animation http://highered.mcgrawhill.com/sites/0072495855/student_view0/ chapter26/animation__organs_of_digestio n.html Digestion Exocrine Gland Cells Exocrine glands are responsible for the release of digestive fluids. Exocrine glands secrete into ducts. Exocrine gland has a duct portion and a glandular portion. – At the end of each branch is an acinus (tube) formed at secretory cells of two types: serous cells (which secrete proteins such as enzymes), ex. chief cells mucous cells (which secrete mucus). Digestion Exocrine Gland Cells Excretion! Now that you’ve learned about digestion, it’s time to check out excretion. Main excretory organs: – Liver – Kidneys Liver The liver is a large organ, weighing about 1.4 kg, making up 3-5% of body weight. It carries out several hundred different functions : – a pivotal role in the maintenance of homeostasis. – Production of bile – Storage and processing of nutrients – Detoxification of poisons and metabolic wastes. Liver Liver We will be looking at… – 1. Blood circulation through liver tissue (The Hepatic Portal System) – 2. Role of liver in regulating levels of nutrients in the blood. – 3.Role of liver in storage of nutrients – 4.Liver synthesis of plasma proteins and cholesterol – 5. Role of liver in detoxification – 6. Process of erythrocyte and hemoglobin breakdown – 7. Effects of excessive alcohol consumption Liver Liver tissue and cells – Relatively simple when compared to its function. – Liver tissue is made up of many lobules, each one comprising cords of liver cells (hepatocytes) radiating from a central vein, and surrounded by branches of the hepatic artery, hepatic portal vein, and bile ductile. – Hepatocytes produce bile and also process nutrients entering the liver via the hepatic portal system Liver 1. The Hepatic Portal System – Refers to all the blood flow from the digestive organs that passes through the liver before returning to the heart. – Hepatic portal blood is rich in nutrients: the liver monitors and processes this load before the blood passes into general circulation. Liver 1. The Hepatic Portal System (continued) – provides a unique double blood supply – Up to 20% of the total blood volume flows through the liver it any one time. – The rich vascularization makes it the central organ for regulating activities associated with the blood and circulatory system. – The liver obtains oxygenated blood from the hepatic artery, but it also receives deoxygenated blood containing newly absorbed nutrients via the hepatic portal vein. Liver 1. The Hepatic Portal System (continued): – Hepatic portal vein: The blood is deoxygenated with lots of nutrients. Inside the liver, it divides up into vessels called sinusoids. Sinusoids are vessels wider than normal capillaries and have more porous walls, consisting of a single layer of very thin cells, with many pores or gaps between the cells and no basement membrane. Blood flowing along the sinusoids is therefore in close contact with the surrounding hepatocytes. The sinusoids drain into wider vessels that are branches of the hepatic vein. Blood from the liver is carried by the hepatic vein to the right side of the heart via the inferior vena cava. Liver Liver 1. The Hepatic Portal System (continued): – The hepatic artery: Carries oxygenated blood from the left side of the heart via the aorta. Branches of the hepatic artery join the sinusoids at various points along their length, providing the hepatocytes with oxygen that they need for aerobic cell respiration. Liver 2. Role of liver in regulation nutrients in blood: – Nutrient: Glucose On arrival in the liver sinusoids, excess glucose is withdrawn from the plasma solution and used in metabolism or stored as glycogen. Glycogen reserves are also stored elsewhere in the body, particularly in the skeletal muscles. Respiring tissues of the body receive glucose supplies from the blood circulation. As the blood glucose levels fall due to respiration in tissues, glycogen reserves in the liver are converted back to gluce to maintain the normal plasma concentration Liver 2. Role of liver in regulation nutrients in blood: – Nutrient: amino acids The liver cells also adjust the level of a.a. as the blood passes along the liver sinusoids. A pool of a.a. is maintained in the plasma, in the liver, and in other tissues undergoing rapid protein synthesis. A.a. are constantly built into up into proteins, which then function as enzymes., components of membranes, and structural components (e.g. collagen fibers, keratin) The demand for new proteins on a daily basis is very high; most proteins are short-lived, but the body cannot store a.a. Instead, excess a.a. are deaminated in the liver. – The organic part of each a.a. is removed and respired, or converted to a fat or carbohydrate. – By this process, the liver ensures that soluble ammonia is not formed and released in the tissues. – Urea is removed from the blood in the kidneys. Liver 2. Role of liver in regulation nutrients in blood: – Nutrient: Fat The fatty acids (and glycerol) that reach the liver are combined to form triglycerides. – These are combined with proteins in the liver, and may be stored there. – Alternatively, they are transported in the blood plasma, mostly as low-density lipoprotein (LDLs) to the tissues. Here lipids may be stored as food reserves (fat) or immediately broken down and respired as a source of energy. Liver 3.Role of liver in storage of nutrients When certain nutrients are in excess in the blood, hepatocytes absorb and store them, releasing them when they are at too low a level. For example, when the blood glucose level is too high, insulin stimulates hepatocytes to absorb glucose and convert it to glycogen for storage. When the blood glucose is too low, glucagon stimulates hepatocytes to break down glycogen and release glucose into the blood. Iron, reinal (vitamin A) and calciferol (vitamin D) are also stored in the liver. Liver 4. Liver synthesis of plasma proteins and cholesterol Liver is the site of synthesis of all the blood proteins, including globulins, albumin, prothrombin, and fibrinogen. Also, most of the cholesterol required by the body on a daily basis is manufactured in the liver. (the remainder is taken in as part of the diet). Liver 5. Role of liver in detoxification *The liver detoxifies harmful substances such as alcohol, or renders drugs and toxins that have entered the blood stream into harmless forms for excretion from the blood circulation in the kidneys. *drugs such as the antibiotics penicillin and erythromycin are handled in this way, as are sulphonamides. *Hormones such as thyroid hormone, and steroid hormones such as estrogen, testosterone, and aldosterone are similarly inactivated, ready for removal from the blood. Liver 6. Process of erythrocyte and hemoglobin breakdown: *Erythrocytes, also called red blood cells, have a fairly short lifespan of about 120 days. *The plasma membrane becomes fragile and eventually ruptures, releasing the hemoglobin into the blood plasma. *The hemoglobin is absorbed by phagocytosis, chiefly in the liver. *Some of the cells in the walls of the sinusoids are phagocytic. They are called Kupffer cells. Inside Kupffer cells the hemoglobin split into heme groups and globins. *The globins are hydrolysed to amino acids, which are released into the blood. Iron is removed from the heme groups, to leave a yellow-colored substance called bile pigment or bilirubin. *The iron and the bile pigment are released into the blood. *Much of the iron is carried to bone marrow, where it is used in the production of hemoglobin in new red blood cells. *The bile pigment is absorbed by hepatocytes and forms part of the bile. Liver 7. Effects of excessive alcohol consumption Cirrhosis of the liver- a chronic inflammation of the liver in which liver cells are destroyed and replaced by fibrous or adipose (lipid-containing) connective tissue. Kidney Main processing centers of our excretory system are the two kidneys. Each is a compact organ, about the size of your fist, nearly filled with about 80 km of fine tubes (tubules) and an intricate network of blood capillaries Body contains about 5L of blood, which circulates repeatedly, allowing for about 1,100-2,000 L to pass though the capillaries in our kidneys every day. Kidney From this enormous (1,100-2000 L) traffic of blood, our kidneys extract daily about 180L of filtrate. – Filtrate is made of water, urea, and a number of valuable solutes including glucose, amino acids, ions, and vitamins. – If we excreted all the filtrate as urine, we would lose vital nutrients and dehydrate rapidly. – But our kidneys refine the filtrate, concentrating the urea and returning most of the water and solutes to the blood. Kidneys Kidneys In a typical day, we excrete only about 1.5 L of urine. “Plumbing” plan of kidneys: – 1. Blood to be filtered enters each kidney via a renal artery – 2. Blood that has been filtered leaves the kidney in the renal vein – 3. urine leaves each kidney via a duct called a ureter and passes into the urinary bladder. – 4. periodically, the bladder empties during urination via a tube called the urethra, which empties near the female vagina or through the male penis Kidney Has two main regions: – Renal cortex (outer layer) – Renal medulla (inner region) – Urine flows into a chamber called the renal pelvis, and from there into the ureter. Kidney Nephron Kidney – Tiny functional units of the kidney – About a million – Consists of a nephron tubule and its associated blood vessels. – Extracts a tiny amount of filtrate from the blood and then refines the filtrate into a much smaller quantity of urine. – Each nephron starts and ends in the kidney’s cortex; some extend into the medulla Kidney Nephron (continued): – Receiving end of the nephron is a cup-shaped swelling called the Bowman’s capsule. – At the other end of the nephron is the collecting duct, which carries urine to the renal pelvis. – Bowman’s capsule envelops a ball of capillaries called the glomerulus which together make up the blood-filtering unit of the nephron. 1. Here, blood pressure forces water and solutes from the blood in the glomerular capillaries across the wall of Bowman’s capsule and into the nephron tubule. 2. This process creates filtrate, leaving blood cells and large molecules such as plasma proteins behind in the capillaries. Kidney Nephron (continued) – Rest of the nephron refines the filtrate. The tubule has three sections: 1. proximal tubule – in the cortex 2. Loop of Henle – A hairpin loop carrying filtrate toward –in some cases, into—the medula and then back toward the cortex 3. Distal tubule – A. Called distal because it is the most distant from Bowman’s capsule – B. Drains into a collecting duct, which receives filtrate from many nephrons – C. in the kidney’s many collecting ducts, the processed filtrate, urine, passes into the renal pelvis and then into the ureter. Nephron Kidney animation http://www.sumanasinc.com/webcontent/ animations/content/kidney.html Kidney Nephron (continued): – The intricate association between blood vessels and tubules is key to nephron function – Two key networks of capillaries 1.Glomerulus – A finely divided portion of an arteriole that branches from the renal artery. – Leaving the Glomerulus, the arteriole carries blood to: 2.Proximal and distal tubules – This second network functions with the tubules in refining the filtrate; some of the vessels parallel the loop of Henle, with blood flowing down in one vessel and back up through another. Leaving the nephron, the capillaries converge to form a venule leading toward the renal vein. Kidney Kidney Excretory system produces and disposes of urine in four major processes: – Filtration Occurs when water and virtually all other molecules small enough to be forced through the capillary wall enter the nephron tubule from the glomerulus. – Reabsorption Refines filtrate; water and valuable solutes, including glucose, salt, other ions, and amino acids are returned to the blood from the filtrate. – Secretion Kidney Also refines the filtrate; substances in the blood are transported into the filtrate. – For example, when there is an excess of H+ in the blood, these ions are secreted into the filtrate, thus keeping the blood from becoming acidic Eliminates certain drugs and other toxic substances from the blood ***both reabsorption and secretion, water and solutes move between the tubule and capillaries by passing through the interstitial fluid. – Excretion Urine, the product of filtration, reabsorption, and secretion, passes through the kidneys to the outside via the ureters, urinary bladder, and urethra. Kidney Reabsorption and Secretion in a nephron Figure 25.11: – pink arrows show reabsorption , which may occur via active transport, passive diffusion, or osmosis. – Blue arrows show secretion – Colored area shows the interstitial fluid, through which solutes and water move between the tubules and capillaries Intensity of color reflects solute conc.; cortex has lowest conc. and medulla has highest conc. Solute conc. of the interstitial fluid exceeds that of the filtrate water moves by osmosis out of filtrate into interstitial fluid Kidney Reabsorption and Secretion in a nephron Figure 25.11 (continued): – Proximal and distal tubule function: Proximal tubule actively transports nutrients such as glucose and amino acids from the filtrate into the interstitial fluid, to be reabsorbed into the capillaries. NaCl is reabsorbed from both proximal and distal, and water follows by osmosis. Secretion of H+ and reabsorption of HCO3- also occur in both proximal and distal, helping to regulate the blood’s pH. Potassium conc. in blood is regulated by secretion of excess K+ into the distal tubule. Drugs and poisons processed in the liver are secreted into the proximal tubule. Kidney Reabsorption and Secretion in a nephron Figure 25.11 (continued): – Loop of Henle and collecting duct function: Major function is water reabsorption Long loop of Henle carries filtrate deep into the medulla and then back to the cortex Presence of NaCl and some urea in interstitial fluid in the medulla maintains the high conc. gradient that increases water reabsorption by osmosis. As soon as water passes into interstitial fluid, it moves into nearby blood capillaries and is carried away. This prompt removal is essential to avoid diluting the interstitial fluid and destroying the conc. Gradient necessary for water reabsorption. Kidney Reabsorption and Secretion in a nephron Figure 25.11 (continued): – Loop of Henle and collecting duct function: water reabsorption stops at hairpin because the tubule there is impermeable to water. As filtrate moves back toward the cortex, NaCl leaves the filtrate, first passively and then actively as the cells of the tubule pump NaCl into the interstitial fluid. – it is primarily this movement of salt that creates the solute gradient in the interstitial fluid of the medulla. Kidney Reabsorption and Secretion in a nephron Figure 25.11 (continued): – Loop of Henle and collecting duct function: Final refining of the filtrate occurs in the collecting duct. By actively reabsorbing NaCl, the collecting duct is important in determining how much salt is excreted in the urine. In the inner medulla, the collecting duct becomes permeable to urea and some leaks out, adding to the high conc. gradient in the interstitial fluid. As filtrate moves through medulla, more water is reabsorbed before the urine passes into the renal pelvis. Kidney Reabsorption and Secretion in a nephron Figure 25.11 (continued): – In sum, the nephron returns much of the water that filters into it from the blood. – Water conservation is one of the major functions of the kidney – Maintain a precise and essential balance btw water and solutes in our body fluids. Kidney – Antidiuretic hormone (ADH) Increased in the blood by a control center in the brain when the solute concentration rises above a set point. Signals nephrons to step up water reabsorption. When the solute conc. Is diluted below the set point, as when we drink a lot of water, blood levels of ADH drop and water reabsorption is reduced, resulting in an increased discharge of dilute urine. Alcohol inhibits the release of ADH and can cause excessive urinary water loss and dehydration, which may account for the symptoms of a hangover. Kidney Dialysis – A person can survive with only one functioning kidney, but if both kidneys fail, the build up of toxic wastes and the lack of regulation of blood pressure, pH, and ion concentrations will lead to certain death if untreated. – Over 60% of kidney disease cases are caused by hypertension and diabetes, but prolonged use of pain relievers, alcohol, and other drugs are also possible causes Kidney Dialysis– How it works – Dialysis means “separation” in Greek – Like the nephron, the machine sorts small molecules of blood, keeping some and discarding others. – Patient’s blood is pumped from an artery through a series of tubes made of a selectively permeable membrane. – The tubes are immersed in a dialyzing solution much like the interstitial fluid that bathes the nephrons. – As the blood circulates through the tubing, urea and excess ions diffuse out. – Needed substances, such as biocarbonate ions, diffuse from the dialyzing solution into the blood – Machine continually discards the used dialyzing solution as wastes build up. Kidney Dialysis – Although life sustaining, it’s costly and time consuming (three times a week for 4-6 hours at a time) – Also requires severe dietary and lifestyle restrictions – Waiting list for kidney transplants , unfortunately, is quite long.