venepuncture 2014
advertisement

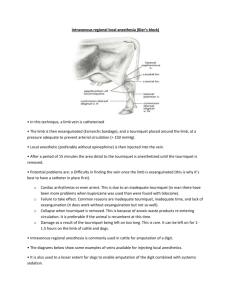
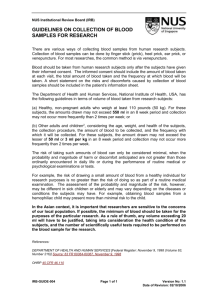
Venepuncture Aims of the day Understand the legislation, policy and practice used when obtaining a venous blood sample Be able to recognize the anatomy and physiology relevant to obtaining a venous blood sample. From the ante-cubital fossa of adults and children over 12 years Understand patient care while taking a venous blood sample. Demonstrate an understanding of possible adverse effects and how to manage them should they occur while taking a venous blood sample Demonstrate and understanding of safe waste disposal. Demonstrate an understanding of infection control especially hand hygiene. Recognize the procedure, technique, materials and equipment for obtaining venous blood samples. Recognise how to report, record and document venous blood samples. Safely perform venepuncture. Accountability, competence & consent Lynne Powell RN. MSc. PgCEd Objectives Discuss the health care support worker code of conduct Briefly define accountability, competence & consent Briefly identify the issues and your responsibilities surrounding accountability, competence & consent Define consent Discuss the legal issues surrounding accountability, competence & consent Code of Conduct for Healthcare Support Workers in Wales (2011) & Code of Conduct for Employers in Wales (2011) Codes of Conduct (2011) Code of Conduct for Healthcare Support Workers in Wales Code of Conduct for Employers in Wales The purpose of both codes is to ensure a high quality service that focuses on the needs & experiences of individuals The basic principle is service user safety and public protection 7 Standards As a health care support worker in Wales you must; 1. Be accountable for your actions & omissions 2. Promote and uphold privacy, dignity, rights and wellbeing of service users 3. Work in collaboration with colleagues and as part of a team 4. Communicate in an open and effective way 5. Respect a person’s right to confidentiality 6. Improve quality of care by updating your knowledge, skills and experience through personal & professional development 7. Promote equality What is accountability? To be responsible and answerable for actions Code of conduct for HCSWs in Wales 2011 Accountability Nurse/HCSW NMC Law Employer Patient Competence Having the necessary ability, knowledge or skill to do something successfully Code of conduct for HCSWs in Wales 2011 Competency Assessment Scale 1. I do not know the knowledge and skills required 2. I know the knowledge and skills required but I don’t have them. 3. I know and I am developing the knowledge and skills 4. I have the knowledge and skills, but I don’t use them. 5. I have the knowledge and skills, and I use them regularly There are National standards to describe the performance level expected of someone doing a particular task. To find out more access NHS Careers http://www.nhscareers.nhs.uk/explore-by-career/widerhealthcare-team/careers-in-the-wider-healthcare-team/clinical-supportstaff/phlebotomist/ RCN http://www.rcn.org.uk/development/general_practice_nursing_career_framew ork/the_gpn_career_framework/level_2__sample_competences_for_a_health_care_assistant Skills for health https://tools.skillsforhealth.org.uk/competence/show/html/code/CHS132/ Consent Permission for something to happen or agreement to do something Consent The voluntary and continuing permission of the patient to receive a particular treatment based on an adequate knowledge of the purpose, nature and risk of the treatment, including the likelihood of success and any available alternatives Informed consent Informed consent is based on a clear appreciation and understanding of the facts, implications and future consequences of an action Patients have the right to make decisions about their own health and medical care Balance of risks and benefits of treatment Consent must be voluntary Failure to obtain consent can be viewed as assault Implied consent Capacity to consent • • • • Mental capacity Act (2005) Over 16yrs Presumption of capacity S1(2) If patient has capacity – bound by decision however irrationa • Record advice given • Get patient to sign – record any refusal to do so • countersignatory Code of Conduct for Employers in Wales (2011) • Employers have to provide mentoring, supervision, monitoring and assessment for the HCSW • HCWS should have a named mentor Employers must: 1. Employ suitable individuals who understand their roles, accountability & responsibilities 2. Ensure HCSW are able to meet the requirements of the Code of Conduct (2011) 3. Provide education and training 4. Promote the HCSW Code of Conduct Employers Employers are legally responsible for the actions you carry out during the course of your employment. This is known as vicarious liability, and your employer will have insurance for this purpose. Vicarious liability is not optional and employers cannot choose to opt in or out. (RCN) Vicarious Liability – (English Law) imposes a strict liability on employers for the wrongdoing of their employees while conducting their duties Lister v Romford Ice and Cold Storage Co[81] created a controversial principle at common law that entitled an employer to recover the indemnity from the employee Negligence The law of negligence This allows a civil action to be taken to financially compensate the person who has suffered unwarranted harm, or damage at the hands of another. Negligence has been defined as : The omission to do something which any reasonable man would do, or to do something which a reasonable man would not do For a case of negligence to be proved by the claimant, three elements must be satisfied. The defendant owed a duty of care to the claimant There was a breach of that duty of care Harm occurred as a direct result of that breach in duty of care Material Contribution – Bailey v. Ministry of Defence (2008) ‘but for’ Duty of Care All healthcare professionals treating a patient owe a duty of care to them The test of when that duty is breached is a peer test. The law will judge your practice against that of a responsible body of practitioners with your qualification (Bolam v Friern Management Committee [1957]) Sources of breach of duty Incorrect act An omission A consent issue Record-keeping Examples of breach of duty MMR given instead of Hib Excessive pain following flu vacc Pt given follow up treatment for only 1 month rather than a year (breach of duty - record keeping) Long term steroids for atopic eczema led to glaucoma Script for atropine given to wrong patient-glaucoma Personal Development Plan (PDPs) Up to date job description Personal development plans Helps identify own training and development needs Demonstrates personal development and career progression Can be used as a tool for annual performance review/appraisal Assists employers and managers to identify areas that need improvement in the practice http://www.wales.nhs.uk/sites3/home.cfm?orgid=739 Infection control and safe waste disposal Infection control Taking blood is the most common intervention that breaches the circulatory system. Therefore compliance with policies and procedures is important to prevent infection Phlebotomy for Health Care Support Workers Lynne Powell RN. MSc. IP Why hand washing is so important? Good hand hygiene is one of the single most effective measures for preventing the spread of infection Our hands move germs from one place to another By hand washing, we remove transient micro- organisms acquired by recent contact with infected patients, or with the environment Hand washing protects both patients, and staff What Lives on our hands? Transient flora – acquired by contact these micro-organisms survive on the skin for less than 25 hours and can be removed by hand washing. Resident flora – part of our normal skin flora these micro-organisms survive and multiply on the skin, they rarely cause infections (other than skin infections) except when introduced into the body through invasive procedures When to decontaminate hands. Every healthcare worker should conduct a risk assessment to determine when to decontaminate Before contact with a patient After completing tasks where hands may have become contaminated with micro-organisms When hands are visibly dirty or soiled Between different types of cleaning procedures Types of Hand Washing Social Hygienic (aseptic) Surgical scrub Social Hand Washing Soap and Water Reduces the numbers of transient micro- organisms upon hands. Renders hands socially clean Sufficient for most daily activities Social Hand Hygiene with Alcohol Gel • • • • • Visibly Clean Hands Utilise approx 3 mls Allow hands to dry prior to patient contact. NOT in cases of D&V Hands must be dry prior to patient contact Hand Drying Micro-organisms transfer most effectively from wet surfaces so always dry hands thoroughly with disposable paper towels. Skin Care Frequent hand washing can cause long term changes in the skin. • Always put soap onto wet hands. • Apply hand cream regularly to protect skin • Report any skin irritation/ abnormality to occupational health advisor. Other Measures • Wear Short Sleeves • Do not wear wrist watches • No jewellery to hands or wrists other than wedding band • Short Nails • No False nails/ Nail Extensions • Moisturise Hands Protective clothing It is appropriate for practitioners to wear non-sterile disposable gloves and disposable apron Wearing gloves does not protect against needle-stick injury but will protect against splashing or spillage Always ask about latex allergy if gloves are worn – use latex free gloves Waste disposal Hazardous Waste Regulations 2005 Defined with the European Waste Catalogue (EWC) Doesn’t include domestic waste Regulated by the Environment Agency Failure to comply can incur fixed penalty notices, fines and even terms of imprisonment Duty of care applies to everyone in the management chain; from the person who produces it to the person who finally disposes of, or recovers it. Use and disposal of sharps needle-stick injuries lead to increased exposure to blood- borne viruses. This can cause pain and anxiety. Sharps injuries can be prevented by careful adherence to good practice. Needles should never be re-sheathed All sharps should be disposed of at point of use Needle Stick Injuries Bleed the site and wash under running water Inform the patient Take the patient’s full details and contact number Report the incident and give patient’s details to Clinical Governance lead for risk assessment. Incident report Environment Check that the area where venepuncture is to be carried out is clean and tidy. Ensure that all equipment is easily accessible, sterile where necessary, intact and in-date. Ensure good lighting. Tourniquets can be a source of infection. Blood spillage Kits Preparation; Pre-test checks and record keeping Aim Discuss preparation Discuss anxiety Identification confidentiality Record keeping Anxiety Anxiety can be caused by: The undergoing investigations Previous bad experience ‘needle phobia’ General dislike of medical procedures Reducing anxiety Talk to the patient (check identity). Ask if they’ve had blood taken before. Do they know what the blood test is for? Explain how to obtain the results. Distraction can be useful (cough technique; creams). Be honest with the patient – regarding pain. Talk the patient through the procedure. Identification Implications of mis-identification Unnecessary tests performed Wrong procedure performed Wrong results given Wrong medication HARM TO PATIENT Patient Identification Full name Date of birth Address NHS number All these are used to identify a patient – remember if this information is lying about others can identify the individual and confidentiality may be breached Confidentiality You have a duty to protect the patient’s information. It is generally accepted that information provided by patients is given in confidence. The Data Protection Act (1998) Caldicott Report The Human Rights Act (1998) Data protection Act (1998) In March 2000, the Data Protection Act 1998 became law and applies to all organisations. It covers computer and manual records across all departments where patient information may be collected and used. The principles in the Act state that information must be: Held securely and confidentially Obtained fairly and efficiently Recorded accurately and reliably Used effectively and ethically Shared appropriately and lawfully The Caldicott Report Caldicott Report provides a number of principles & recommendations aimed at supporting the NHS in improving the way it handles identifiable information. There are 6 Caldicott principles; Justify the purpose(s) of using confidential information Only use it when absolutely necessary Use the minimum that is required Access should be on a strict need-to-know basis Everyone must understand his or her responsibilities Understand and comply with the law The Human Rights Act 1998 Article 8 – The Right to Respect for Private and Family Life The right to respect for private life The right to respect for family life The right to respect for one’s home The right to respect for correspondence The Act can be used only against a public body therefore the NHS are subject to the Act Failure to comply with either the The Human Rights Act or The Data Protection Act could lead to litigation Record keeping 4. Communicate in an open and effective way 4. Document and maintain clear and accurate record of your care and report any changes or concerns in the condition of individuals immediately to a senior member of staff Good record keeping meets legal requirements. protects staff in legal situations. meets professional statutory requirements. supports clinical audit. Good record keeping helps to protect the welfare of patients by promoting: High standards of clinical care. Continuity of care. Better communication and dissemination of information between members of the inter-professional health care team. An accurate account of treatment and care planning and delivery. The ability to detect problems, such as changes in the patient’s condition, at an early stage. Record keeping ENSURE YOU HAVE THE CORRECT PATIENT Remember the patient’s record is a legal document. Remember patients have the right to access their medical records. Record information as soon as it is obtained to minimise the chance of mistakes. Involve the patient in the compilation of their records. Enter recordings into the correct Read codes. Record the facts. Avoid abbreviations as they can be confusing Avoid duplication. Useful information WHO guidelines on drawing blood: best practices in phlebotomy Code of conduct for healthcare support workers in Wales Code of Conduct for Employers in Wales Data protection Act (1998) The Caldicott Report Hazardous Waste Regulations 2005 Look at health board guidelines The clotting process Taking a blood sample Aims Describe the anatomy of the ante-cubital fossa Discuss the appropriate choice of vein Preparing the patient for taking blood Idendtify the order of draw Factors affecting venepuncture Discuss adverse effects and how to manage them All arteries carry blood away from the heart All veins carry blood to the heart Most arteries carry oxygenated blood Most veins carry de-oxygenated blood • Veins have vavles that prevent blood from flowing in the wrong direction • Veins are wider than arteries • Contraction of body muscles helps the blood flow through the veins • Arteries have more elastic tissue and a thick muscular layer to cope with the high pressure of blood flow caused by the heart beat • Capillaries transport blood from the arterioles to venules. • They are microscopic vessels which are in most of our organs. • They are one cell thick so they allow exchange of gas (O2;CO2); salts and water to occur between the capillaries and surrounding tissue. Choice of vein The vein should be easily accessible. Choose a vein that can accommodate repeated blood samples. Choose sites that are less sensitive. Do not choose veins that are adjacent to an infected area. CVA/mastectomy – do not use affected arm. The tourniquet may cause pain if joints are inflamed through rheumatoid arthritis. Improving access to veins • • • • The application of a tourniquet promotes venous distension. The tourniquet should be tight enough to impede venous return but not restrict arterial flow. The tourniquet should be placed approx 7-8 cm above the intended venepuncture site. Placing the tourniquet over a sleeve or paper towel may be more comfortable for the patient to prevent pinching of the skin. The tourniquet should not be left on for more than one minute as it may cause haemoconcentration or pooling of the blood, leading to inaccurate results. The tourniquet should be released as soon as the vein has been successfully accessed. Opening and closing of the fist encourages muscles to force blood into the veins however this action may affect certain blood results e.g. potassium Blood supply can be increased by lowering the arm below the heart level Venodilation and venous filling can be encouraged with warm compressions either of clothing or heat packs covered in towels. This procedure can only be used once prior to any venepuncture procedure. Pathology forms biochemistry haematology • Renal • LFT • FBC • Glucose • PV • Lipids • TFT • Bone • B12/folate • ferritin Preparation 1. Wash hands 2. Assemble the equipment - maintain sterility 3. Identify the patient 4. Identify the tests required on the form 5. Allow the patient time to ask questions & express concerns 6. Site patient – comfortable position arm extended & supported Action & observation • Determine the patient’s preferred site. • Ensure patient’s skin is clean. • Apply tourniquet (quick release) to upper arm approximately 3-4 ins above puncture site. • Apply enough pressure to stop venous flow but not arterial flow – check pulse. • Observe and palpate selected vein (do not over palpate). • Instruct the patient to hold still. Action & observation Insert the needle into the vein. Once blood is flowing freely release tourniquet. Fill each tube to its mark. Invert the tube 8-10 times (do not shake) Place cotton wool over site. Remove needle. Apply pressure to site. Dispose of needle appropriately. Check site and apply dressing, ensure patient comfort. Complete labels on sample bottles. Order of draw Blue tubes Red tubes Yellow tubes Purple tubes (EDTA) Grey tubes Factors affecting the sample Wrong bottle used Wrong order of draw (contamination) Tourniquet too tight Sample left overnight Mislabeling Bottles not filled Potential complications Excessive bleeding Drug therapy (e.g. aspirin; clopidogrel; warfarin; heparin) Disease process (liver disease; hemophilia; von Willebrand disease; deficiency of vitamin k.) Prevention – ASK; don’t overuse tourniquet; may need clotting therapy before venepuncture Potential complications Haematoma – collection of blood leaked from the vein at the puncture site. Causes Overshooting the vein Inadequate pressure applied after procedure Failure to release the tourniquet before removing the needle If haematoma occurs during the procedure, remove tube, release tourniquet, remove needle, apply firm pressure for 23 mins and raise arm. Potential complications Bruising caused by blood seeping into the tissue. May occur in patients that bleed easily. Drugs(e.g. aspirin) Preventable by Using suitable veins Correct angle and insertion technique. Do not apply excessive pressure during procedure, with tourniquet. Use skin traction during insertion. Apply adequate pressure after procedure Potential complications Arterial puncture – leads to bright red blood pulsating into the tube. Preventable by thorough assessment of site and correct insertion technique. Management: Remove needle, apply digital pressure for 5 mins then pressure bandage for 5 mins. Do not reapply tourniquet to that arm for 24 hrs. seek medical help. Needs to be reported (pt records and incident reporting) Potential complications Excessive pain – caused by frequent use of vein, poor technique (blind plunging where a nerve or valve is touched), anxiety, fear or low pain threshold. Ensure patient is comfortable, arm supported Avoid sites of known nerves (lower part of cephalic vein, near wrist), Consider local anaesthetic cream Distraction – ask pt to concentrate on breathing If possible nerve damage – seek help from Dr. or nurse Potential complications Fainting Some patients may feel weak and become dizzy or faint. Patients have no control over this condition. Call for help. Ask the patient to put their head between their knees. If they feel no better help them to the floor – lie them flat - ensure a safe environment. Get help (phone). Potential complications Remember Most complications are preventable Assess site thoroughly Use correct insertion technique Use appropriate use of tourniquet Avoid blind plunging Safety checklist Do you have the right person? Is the patient comfortable and easily accessible? Are you comfortable? Is there a history of fainting? Is equipment ready and accessible (e.g. sharps bin)? Is your work area clean and tidy? Do you have adequate lighting? Ensure you have the correct patient Enquire about allergies (e.g. latex; plasters) Use quick release tourniquet. Do not re-sheath used needles. Finally All adverse incidents should be reported and an incident form filled in Any questions?