Bhatt/Hartzell - The Shift from Volume to Value
advertisement

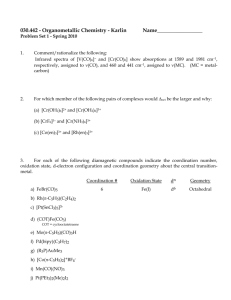
ECG Management Consultants, Inc. The Shift From Volume to Value: Emerging Reimbursement and Alignment Models August 22, 2014 Ms. Purvi B. Bhatt, Senior Manager Mr. Sean T. Hartzell, Senior Manager Agenda I. II. III. IV. V. Market Trends Alignment Models Innovative Payment Models Case Studies Key Takeaways Appendix A – Alignment Model Examples 1 0100.015\313186(pptx)-E2 I. Market Trends 2 0100.015\313186(pptx)-E2 I. Market Trends Key Issues The burning platform is here. • Evidenced by significant federal, state, and commercial payor initiatives, strategic direction, and financial urgency (governmental). • Health systems focused on eliminating waste. • Strong physician partnerships critical to driving change and protecting market share. • Systems focused on efficiencies must restructure contracts to be rewarded for improved value. The pacing of the movement to value-based care is critical. • Providers largely dependent on a productivity-based system and cannot simply “flip a switch.” • As utilization is taken out of the system (through focused medical/chronic disease/population management initiatives), hospital and specialist financial performance at risk if contracts not restructured. Not all organizations can or should strive for the end-state model (in its totality). • Critical (no matter what provider type) to focus on efficiencies, measurement, and quality. • Essential to execute strategy that closely aligns organization with preferred care partners. 3 0100.015\313186(pptx)-E2 I. Market Trends End-State Model The end-state model is a clinically integrated network (CIN) of providers who follow common clinical protocols, have aligned measures and incentives based on improved value, and obtain joint payor contracts. Independent Providers Independent Providers • • • • Fragmented Delivery System Home Health SNF Pharmacy Other Employed Physicians Outcomes • Provider Organization • Management/Governance • Clinical Protocols • Disease Management • Wellness • Integrated EHR • Performance Measurement • Reporting • Disease Registry • Joint Payor Contracting • Employee Health Plan (EHP) • Funds Flow Design • Aligned Incentives • • • • CIN Home Health SNF Pharmacy Other Employed Physicians Hospital Hospital 4 0100.015\313186(pptx)-E2 I. Market Trends A Time for New Alliances “The goals of population health management may be encouraging rampant consolidation across the healthcare industry, but some systems are pushing back and seeing whether they can achieve the same results with looser arrangements.” – Modern Healthcare, July 2013 Philadelphia Indianapolis georgia Three Leading Health Systems Form New Initiative Three Health Systems Create Accountable Care Consortium 23 Hospitals Form Care Alliance Three Philadelphia-area health systems form an alliance to work collaboratively to improve care and meet demands of health reform. The initial focus is to jointly manage the healthcare benefit plans of the systems' employees and their families. This new alliance will bring together more than 30 facilities, including 6 of the 10 that make up Indiana's Suburban Health Organization. “Healthcare reform has required healthcare systems to think differently than in the past,” – Vincent Caponi, CEO. In Central and Southern Georgia, 23 hospitals form a not-for-profit LLC called Stratus Healthcare. This new network is a partnership allowing the member hospitals to collaborate while remaining independent. . 5 0100.015\313186(pptx)-E2 I. Market Trends The Spectrum of Integration Independent/ Competitive Segmented Integration Clinical Integration Provider Network/ACO • Traditional medical • Organizational models • Systems and processes in • All characteristics of staff/hospital relationship. • Physicians are “customers” of the hospital. • Competition over outpatient services and revenue streams. • FFS mechanisms predominate. created to achieve physician/hospital integration (e.g., joint ventures [JVs], employment). • Physician-only models may include entering into managed care risk (e.g., independent practice association [IPA]). • Focus is on creating structures that align strategic and financial goals – typically of one aspect of the healthcare delivery system (e.g., a service line, an outpatient service, physician recruitment, payor type). place to measure quality and cost across a continuum (e.g., hospital, physicians, pharmacy, outpatient services). • Selective participation of physicians who are willing to comply with set protocols and outcome measures. • Pursuit of new models of clinical care delivery to enhance the management of chronic disease and coordination of care overall. clinical integration with a greater degree of financial integration and interdependence. • Ability to approach the market and payors with an integrated system (i.e., hospitals, physicians, and other providers of care). • Culture is totally focused on the success of the system versus individual components (e.g., hospital versus physician group). 6 0100.015\313186(pptx)-E2 II. Alignment Models 7 0100.015\313186(pptx)-E2 II. Alignment Models How Physicians Are Organizing Physicians are choosing to organize themselves in response to changing payor dynamics. SingleSpecialty Group Management Services Organization( MSO) Multispecialty Group • Loose; little • Shared services, interrelationship. • Difficult to realize IPA/ PHO1 lower cost. • Little negotiating economies of scale. power. Service Line Management Equity JV • More risk sharing. • Rewards for improved performance. Professional Services Agreement (PSA) Hospital Employment • More integrated relationship. • Possible hospital financial support. Ultimately, group dynamics will play into the preferred relationship/tactic. 1 PHO = Physician Hospital Organization. 8 0100.015\313186(pptx)-E2 II. Alignment Models Alignment Approaches and Their Characteristics There are a variety of approaches for pursuing alignment, yet the requirements for infrastructure and capabilities related to population management will vary. Alignment Approach Ability to Maintain Financial Autonomy/ Independence Ability to Leverage Infrastructure Development Costs Ability to Facilitate Clinical Collaboration Ability to Manage Care Across Continuum Ability to Pursue Joint Contracting With Payors Single-Specialty Group High Low Medium/High Low High Multispecialty Group High Low Medium/High Medium High MSO High Medium Low Low Low PHO Medium/High Medium/High High Medium/High Medium IPA Medium/High Medium/High High Medium/High Medium Service Line Management Medium/High Low High Medium/High Medium Equity JV Medium Low Low Low Medium PSA Medium Medium High Medium Medium/High Low High High High High Hospital Employment 9 0100.015\313186(pptx)-E2 II. Alignment Models Range of Provider/Payor Collaborations Providers are contemplating a range of payor collaborative models, a thoughtful network strategy, and models for building appropriate insurance capabilities. Range of Payor and Provider Collaborative Models Traditional Contractual Relationship Incentive Arrangement Risk Contract JV Clinical Programs Infrastructure Research JV Financial Integration Clinical Integration ACO Merged Organization Single Organization/O wnership Major Considerations Network Strategy Need for Premium Access Need for Insurance Capabilities Degree of Clinical/Financial Integration Level of Commitment Complexity and Financial Investment Potential Upside 10 0100.015\313186(pptx)-E2 II. Alignment Models Network Participation Tiers Network formation typically includes participation tiers, allowing organizations to choose the most appropriate level of their commitment and exclusivity related to clinical integration efforts. Typical Network Tiers Network Contractors • No governance or decision-making participation. • FFS only. • For example, radiology group. Network Participants • No governance or decisionmaking participation. • FFS with shared savings. • For example, home health agency. Network Affiliates • Participation in decision making. • Potential risk sharing. • For example, aligned independent medical group. Network Core • Ownership (if necessary). • Governance. • Risk sharing. • Surplus sharing. Level of Commitment and Exclusivity A provider organization’s strategy must consider how it fits into the full continuum of care and its vision for future care delivery. 11 0100.015\313186(pptx)-E2 II. Alignment Models Alignment of Payment Models With Network Goals The funds flow is an important tool for creating alignment among the participating providers with both the immediate and longer-term goals of the network. Possible Transition Over Time Characteristic Emphasis First Generation • Gain experience. • Develop capabilities. • Generate modest financial/ Second Generation • Leverage experience. • Expand capabilities. • Participate in associated cost improvement. Scope EHP only. Ultimate Goal • Market/promote experience. • Capitalize on capabilities. • Engage in population health savings. • EHP. • Medicare Advantage (MA) • and/or commercial plans. Medicaid HMO contracts. management. • • • • EHP. MA and/or commercial plans. Self-funded employer plans. Medicaid HMO contracts. Level of Risk Moderate upside opportunity. Shared savings. Shared risk. Business Requirements/ Capabilities Evolving. More advanced. Advanced. Level of Risk 12 0100.015\313186(pptx)-E2 III. Innovative Payment Models 13 0100.015\313186(pptx)-E2 III. Innovative Payment Models Clinically Integrated Models Less Integrated Independent Contracting Decisions “Messenger” Model Third-Party Messenger More Integrated Range of Clinical Integration P4P Physician/Hospital Alignment Potential Models of Integration Risk Sharing “United Front” Clinical Integration Coordinated Care Financial Integration Merger/ Acquisition • This model involves • Care is provided in • Providers share • Patient-centered care • System-wide efficiencies separate, independent, and unilateral contracting decisions. • Offers and counteroffers between individual providers and payors are conveyed by PHO messenger. • Objective information is communicated to providers regarding proposed contract terms. accordance with quality targets. • The quality of care is reviewed and monitored. • There are provisions for adequate peer review if quality targets are not achieved. • Payments are based on historical activity to avoid referral incentives. responsibility for cost or utilization and have a significant positive gain for achieving targets. • Members or owners share financial risk directly or through membership in another organization. • Members may not account for more than 30% of physicians in local market. focused on common understanding of desired outcomes. • Broad network of providers. • Integrated IT and efficient information exchange. • Compliance with utilization review and performance standards. across providers. • Centralized ownership. 14 0100.015\313186(pptx)-E2 III. Innovative Payment Models Range of Value-Based Payment Models As more risk is introduced into payment methodologies, providers are moving toward greater integration and scale to efficiently develop capabilities for value-based models. Risk Continuum Associated With Various Reimbursement Structures Medical Home1 FFS Bundled Payment P4P Payment for Episodes of Care Global Payment With Performance Risk and P4P Total Cost of Care/ Shared Savings Global Payment With Financial Risk Clinical and Financial Integration Complexity/Broader Capabilities Required Greater Risk/Potential Upside 1 Medical homes that receive extra dollars for patient management. Source: Healthcare Financial Management Association, “Accountable Care: The Journey Begins,” August 2010. 15 0100.015\313186(pptx)-E2 III. Innovative Payment Models Contracting Vehicles The economic reality of reform has caused enormous changes in the insurance industry; plans are differentiating themselves through the creation of innovative products. Payor initiatives are putting downward pressure on provider reimbursement. Health Exchanges Commercial MA Narrow Networks P4P Bundled Payments PatientCentered Medical Home (PCMH) Shared Savings Disease Management Shared/ Full Risk Those providers positioned for a value-based system will emerge as market leaders. Managed Medicaid EHPs Dual Eligibles 16 0100.015\313186(pptx)-E2 III. Innovative Payment Models Range of Potential Risk Arrangements Global payment arrangements (total cost of care models) range from shared savings (e.g., gain sharing, “one sided” track) within an FFS environment to shared-risk and ultimately to global-risk (e.g., capitation) arrangements with quality bonuses. Gain Sharing/One-Sided/ Asymmetric Model • • • “Two Sided”/ Symmetric/SharedRisk Model Global Risk/Partial Capitation Model Ideally, as a provider network matures, it will adopt payment models with increasingly more risk. With the increased risk should come the opportunity to earn a greater percentage of shared savings, because the network/entity will be more accountable for cost and quality. As organizations become more adept at managing risk and enhance their clinical integration through care process redesign and better health IT, they can transition from risk-free or one-sided risk models to two-sided risk models in which organizations suffer a loss if they spend more than their projected global medical spending amount. 17 0100.015\313186(pptx)-E2 III. Innovative Payment Models Critical Success Factors in Full-Risk Contracting Overall, there are major clinical, financial, operational, and strategic requirements that will drive successful population health management. Provider Composition/Practice • Sufficient primary care size for population • • • • • • • • Governance and Management • Meeting of financial strength requirements to accept management. risk. Clinical consideration for specialty management • Legal structure in place to receive and distribute and/or involvement for patients with chronic payments. conditions. • Broad base of clinical and administrative leadership. Hospital partnership. • Clear lines of authority and accountability among Support of the transformation of the care process to related entities. a team approach. • Alignment of compensation/funds flow programs. Use of physician extenders. • Adequate incentives for population. Group visits, e-visits, or other forms of patient • Alignment of incentives. encounters. Communication tools to facilitate integration of practice teams. Patient satisfaction monitoring. Patient attribution method in place. Source: Adapted from the AMGA Accountable Care Organization Readiness Assessment, 2010. 18 0100.015\313186(pptx)-E2 III. Innovative Payment Models Critical Success Factors in Full-Risk Contracting (continued) Care Management/Coordination • • • • • • • • • • • Chronic care management processes. PCMH practices. Predictive analytical tools to identify high-risk patients. Case managers assigned to high-risk patients. Systems in place to manage transitions of patient care settings. Medication reconciliation. Behavioral health programs integrated into care management plans. Home health and other extended care programs integrated into care management plans. Patient communication established as standard practice. Patient follow-up and reminder systems. Follow-up visits and referrals scheduled at time of initial encounter. Source: Accountability/Reporting • Systems to manage population costs. • System-wide measures and performance tracking of • • • • • • • • • • quality and efficiency. Episode-based resource-use metrics linked to quality metrics. Public reporting on outcomes/costs. Common EHR across providers. Practice guidelines/clinical protocols embedded in EHR. Appropriate alerts for clinical decision support. Processes to improve coding. Registries for chronic disease patients. E-prescribing used by PCPs. Formularies for generics. Electronic patient communication. Adapted from the AMGA Accountable Care Organization Readiness Assessment, 2010. 19 0100.015\313186(pptx)-E2 IV. Case Studies 20 0100.015\313186(pptx)-E2 IV. Case Studies Example #1 – Nonurban Hospital With Local Providers Background • 250-bed hospital, 40 miles outside of major metropolitan • • • • • • • • • city. Inpatient market share in the core market is high. Payor market is consolidated, and the local Blue Cross plan is dominant. The medical community is predominantly composed of small, independent, single-specialty physician practices. A significant proportion of the primary care base, while generally loyal to the hospital, is economically aligned with a regional network of primary care practices. The hospital is preferred by affiliated physicians and patients. Multiple clinical affiliations augment local expertise. Quality, excellence, and continuous improvement are areas of ongoing emphasis for the organization. Costs and utilization are lower compared to other area hospitals. Limited experience with pilots for care management of specific patient populations. Considerations for the Future • Most of the covered lives cared for by the hospital and • • • • • • • the medical community are “owned” by the regional primary care network. Market share of covered lives will be a key measure of indispensability in the future, replacing today’s emphasis on market share of beds, discharges, and/or specialists. Local PCPs have growing expertise to support the management of care for specific populations. Most nearby competitors have achieved greater economic alignment with physicians and have a larger base of employed PCPs. Hospital-centric mind-set means health system model is underdeveloped. Despite pilot initiatives around care coordination, the care model remains fragmented, with generally uncoordinated care transitions. Success in new care delivery models and under new payments models will require more than improved performance on traditional metrics. Financial capacity to fund growth is limited. 21 0100.015\313186(pptx)-E2 IV. Case Studies Example #1 – Nonurban Hospital With Local Providers (continued) The key to being relevant in the future is to strengthen existing relationships and establish new ones that add value, capture new markets, and accelerate the development of new competencies and capabilities. Secure an economically aligned referral base in order to be indispensable in the primary market. Build the competencies required to be successful as healthcare reform drives delivery and payment system changes. Enhance financial strength and market position to continue to operate as an independent hospital/health system. Develop a system of community care that is no longer hospital-centric, reaches out proactively, and engages all providers and the patient. Shift focus from managing episodes of hospital-based care to managing the health of a population, thereby requiring clinical integration. 22 0100.015\313186(pptx)-E2 IV. Case Studies Example #1 – Nonurban Hospital With Local Providers (continued) Transforming Care Delivery System • Bundled payment initiatives. • Economic alignment between Financial incentives for high-quality, lowcost care to a large patient cohort. PCPs and specialists. • Improved geographic access to primary care. • Continuous quality improvement initiatives. • Pilots with EHP. • Platform for exchanging electronic health data. • PHO. • Strong physician/hospital relationships and shared decision making. Population health management tools and delivery of targeted, cost-effective care. • Health system model with stronger linkages across system of care. • Evidence-based protocols and Infrastructure that encourages and facilitates collaboration. care guidelines. • Coordinated care transitions using decision support tools and reporting capabilities. Culture that supports physicians in delivering the best care. • Cost discipline maintenance. • Capitalizing on existing expertise. The previous investments and commitment by the physicians and the hospital in cultivating a strong partnership, implementing technology, and engaging in continuous improvement provide a strong foundation for the medical community to build upon. 23 0100.015\313186(pptx)-E2 IV. Case Studies Example #2 – Nonurban CIN More than a dozen inpatient facilities and over 1,000 employed physicians formed a CIN focused on improving the quality and efficiency of care Vision being delivered. The CIN members will collaborate and innovate to: Improve Outcomes Gain Efficiencies Deliver Value to the Populations the CIN Serves Guiding Principles Support Local Autonomy and Independence Collaborate With Independent Providers Who Choose to Work Together Provide Options for Degree of Involvement Engage Physicians Focus on Innovating to Create Value for Purchasers and Patients 24 0100.015\313186(pptx)-E2 IV. Case Studies Example #2 – Nonurban CIN (continued) Two main functional areas have been identified to provide benefit to members of the CIN: (1) payor contracting and (2) shared services. Shared Services Payor Contracting • • • • Integrated IT. – Health information exchange. – Population health/utilization data warehousing. – Disease registries. Utilization, medical management, and care design. – Utilization review. – Standard protocol development and compliance. – PCMH. – Standardized care transitions. – Care management and infrastructure. Contracting. – Collective negotiations. – Risk-based contracting/shared risk. – Network formation and contract execution. – Funds flow design and planning. Managed care administration – Risk management support. – Data analytics and reporting. – Surplus and deficit accounting and distribution. • • • • • Vendor contracts and pricing. – Supply chain. – Insurance. – Consulting. Provider credentialing. Best practices and education. – Evidence-based practice guidelines. – Quality improvement. – Staff “in-services.” – Industry trends. – Regulatory compliance. Medical delivery support. – Telemedicine. – Physician staffing/rotations. – Medical transport. Centralized corporate/other functions. – Human resources (HR)/benefits. – Revenue cycle. – IT. – Pharmacy. 25 0100.015\313186(pptx)-E2 IV. Case Studies Example #2 – Nonurban CIN (continued) The ultimate goal is to evolve the CIN through the management of a series of phased-in populations. • • • The CIN will begin with consistent measurements and the development/refinement of programs for major chronic conditions, using the EHP as a starting point. The CIN will evaluate payor contracting opportunities to expand population management capabilities to additional patient populations. As a first step in this process, it will evaluate MA. Second Generation First Generation • EHP. • MA. Ultimate Goal • Commercial contracts. • New Medicare or Medicaid programs. • State health exchange. • Direct-to-employer contracting. • CIN. A single EHP network will be developed by year-end 2014 aimed at improving the health of employees through clinical integration and reducing the total cost of care. 26 0100.015\313186(pptx)-E2 V. Key Takeaways 27 0100.015\313186(pptx)-E2 V. Key Takeaways So What Does It All Mean? Practice Responses New Demands for Care New demands from patients and payors are forcing care delivery changes in hospitals and physician practices. Access • Schedules with same-day open access and/or extended hours. • Dedicated care managers or disease management PCMHs. • New delivery model (PCMH). • Coordination with dentists, pharmacists, and nutritionists for preventive care. • New patient encounter types (e-visits, e-mail). • Stratification of patient panel at start of visit to off-load physician schedule. Coordinated Care Comprehensive Care • • Provision of services at schools, employers, etc. Evidence-based practices. • • • PCP collaboration with specialists to set expectations for referral coordination. Standards for information sharing (e.g., patient discharge notes, medication reconciliation). Organization-wide standard protocols for patient follow-up. Patient Engagement and Communication • Patient portals, chat rooms, e-visits. • Group visits. • Education champions in each practice. • Online scheduling. • In-office resource centers. • Telephone calls for patient follow-up. Organizations can leverage the new care model and position themselves in the competitive healthcare market as a high-quality, high-value provider. 28 0100.015\313186(pptx)-E2 29 0100.015\313186(pptx)-E2 Presenter Biographies Ms. Purvi B. Bhatt, Senior Manager, ECG Management Consultants, Inc. • Ms. Bhatt works with providers and health systems as they transition from volume- to value-based delivery systems, analyzing quality and financial data; facilitating stakeholder discussions regarding a culture of collaboration, creativity, and accountability; and developing ACO/delivery-based strategies. • She has master’s degrees in business administration and health services administration from the University of Houston and a bachelor of arts degree in psychology from the University of Texas at Austin. • Ms. Bhatt can be reached at 703-522-8450 or pbhatt@ecgmc.com. Mr. Sean T. Hartzell, Senior Manager, ECG Management Consultants, Inc. • Mr. Hartzell is the co-leader of the firm’s transaction advisory service line, which focuses on developing and disseminating the firm’s thought leadership in the areas of transaction planning, facilitation, and implementation, and he has published thought leadership pieces and spoken nationally on these topics. • He received a master of business administration degree from the Darden Graduate School of Business at the University of Virginia and a bachelor of science degree in operations research and industrial engineering from Cornell University. • Mr. Hartzell can be reached at 703-522-8450 or shartzell@ecgmc.com. 30 0100.015\313186(pptx)-E2 Appendix A Alignment Model Examples 0100.015\313186(pptx)-E2 Appendix A Alignment Model Examples1 Collaborators Horizon BCBS, PCPs, and New Jersey Academy of Family Physicians Location/ Date New Jersey, 2011 Details • Pilot PCMH program included eight practices and 24,000 Horizon members. • Horizon paid practices a care coordination fee ($2 to $3 per member per month [PMPM]) to support practice transformation and for the provision of additional services under the PCMH model, in addition to existing FFS reimbursement. • Practices are also eligible for additional payments for meeting quality and utilization outcomes. • An expanded version of the program is now implemented in 48 practices serving 154,000 Horizon members. California Public Employees’ Retirement System (CalPERS) and Multiple HighQuality Hospitals California, 2008 • CalPERS limited what it would pay for hip and knee replacements to $30,000. • Found several hospitals willing to stick to threshold amount. • Some CalPERS members have 100% coverage, including travel costs, when electing to receive these procedures at participating facilities. Outcomes • 8% higher rate in improved diabetes control (HbA1c). • 6% higher rate in breast cancer screening. • 6% higher rate in cervical cancer screening. • 10% lower cost of care (PMPM). • 26% lower rate in emergency room (ER) visits. • 25% lower rate in hospital readmissions. • 21% lower rate in hospital inpatient admissions. • 5% higher rate in the use of generic prescriptions. • In 2008, hip and knee replacement cost CalPERS $55 million, and hospital bills ranged from $15,000 to $110,000 with no discernible difference in quality. • In 2011, the average price per surgery dropped nearly 28% to $23,113. • CalPERS has since applied thresholds to colonoscopies, cataract surgeries, and arthroscopies. • Members required to pay for charges above threshold when using outpatient hospitals instead of ASCs. 1 Source: Oregon’s Office for Health Policy and Research, Alternative Payment Methodologies. A-1 0100.015\313186(pptx)-E2 Appendix A Alignment Model Examples1 (continued) Collaborators 1 2 Location/ Date BCBS Illinois and Advocate Health Care Illinois, 2011 Texas Medicaid, MCOs, and Network Physicians and Hospitals2 Texas, 2012 New York Medicaid Program and Health Plans Contracting With Medicaid New York, 2002 Details Outcomes • Began shared savings program for fully and self-insured • In the first 6 months of 2011, hospital admissions commercial PPOs in Chicago area. • Performance and cost standards were implemented for physicians, who would be penalized for failure to meet them. • ER visits fell 5.4%. • Medicaid managed care contracts in Texas require MCOs to • Potential savings related to readmissions is $120 conduct gain-sharing programs in which network physicians and hospitals share a portion of an MCO’s savings resulting from reduced utilization and inappropriate admissions. • Contracts also include a Quality Challenge Award whereby 4% of an MCO’s capitation is withheld based on eight quality measures. • If an MCO does not achieve performance levels, future monthly capitation payments will be adjusted by an appropriate portion of the 4% at-risk amount. Unearned funds are redirected to the Quality Challenge Award. million in the first year. • The state found that most preventable admissions were related to mental health conditions. • The program underwent substantial changes in 2014 to emphasize incremental improvement, rather than quality challenge and at-risk measures. • This is part of Texas’ broader effort to shift from FFS to managed care for Medicaid populations. • New York Medicaid offering quality-based bonuses and • During first 4 years of program, New York paid performance-based auto-assignment incentives to health plans. • Using HEDIS and CAHPS measures to develop quality and patient satisfaction benchmarks. • Created quality incentive score based on a scale of 150 points. nearly $71.5 million in bonuses. • The state saw an increase in enrollment plans that it deems as high quality. • A study by The Commonwealth Fund reported that appropriate postpartum care rose from 49% to 68%. per member decreased 10.6% compared with 2010. Source: Oregon’s Office for Health Policy and Research, Alternative Payment Methodologies. Source: Deloitte report on Texas Medicaid reform. A-2 0100.015\313186(pptx)-E2 Appendix A Alignment Model Examples1 (continued) Collaborators Oregon Health Plan (Medicaid) and Healthcare Providers – Care Coordination Organizations (CCOs) Location/ Date Oregon, 2012 Details • Initiative calls for the formation of a cross-functional network of all healthcare providers working together to provide medical services to persons covered under the Oregon Health Plan. • As of September 2013, 16 CCOs are in operation. • CCOs participate in quality pool funding, which is a pool totaling 2% of the aggregate CCO payments. The payments are made completely outside of the capitation rates. • Oregon plans to increase the incentive percentage on an annual basis and has a waiver in place that allows the supplemental pool to grow to 5%. • Oregon publishes Quarterly Progress Reports, showing the performance of the CCOs on 33 designated measures. Of these measures, 17 are linked to incentive payments, and the remaining measures are data the CCOs are required to submit to the state to be reported publicly. Outcomes • Oregon believes one of the most successful aspects of its program is the state’s strong relationships with the CCOs. One of the reasons for these strong relationships is that Oregon designates a single point of contact who is made available to the CCOs to address all questions regarding quality measures and the reporting and analyzing of their results. • Utilization and spending data in 2013 compared to 2011: – ER visits down 9%. – ER spending down 18%. – Hospitalization for congestive heart failure down 29%. – Hospitalization for obstructive pulmonary disease down 28%. – Hospitalization for adult asthma down 14%. – Primary care outpatient visits up 18%. – Adoption of EHRs up 29%. 1 Source: Oregon’s Office for Health Policy and Research, Alternative Payment Methodologies. A-3 0100.015\313186(pptx)-E2