Dysphagia Power Point

Review: Osteophyte pic1: esophagus has air
Cricopharyngeal bar
Laryngectomy: No CP myotomy
Esophageal Phase
• Cervical Esophageal phase of swallowing involves the initial peristaltic wave in the esophageal musculature
• CANNOT be modified by therapy; however postural changes can be helpful
• Observable in a lateral view during MBSS
• If esophageal dysfunction is suspected, a barium swallow should be performed after the MBSS or a referral to a GI specialist is recommended.
– MBSS is performed 1 st to r/o aspiration. If aspiration is evident, the barium swallow is deferred until the risk of aspiration is eliminated.
Esophageal Phase
• SLP need to be knowledgeable about esophageal disorders that can masquerade as pharyngeal swallowing disorders bc they cause backflow into the pharynx, causing aspiration.
Esophageal Phase
• Symptom: Esophageal to Pharyngeal Backflow
• Dysfunction: Achalasia (failure of the LES to relax), reflux, tumor, stenosis, etc
• Normal: Material enters stomach and does NOT backflow into esophagus or pharynx
• Abnormal: Backflow of material from the esophagus enters the pharynx by opening of the
UES. May cause aspiration or symptoms of pharyngeal swallowing disorder.
• Achalasia, reflux, tumor, stenosis results in esophageal to pharyngeal backflow
Esophageal Phase
• Symptom: Food entering the esophagus flows back into the trachea via a hole in the party wall/Tracheoesophageal (TE) wall; aspiration after the swallow below the level of the glottis
– Usually located at the level of the 1 st to 3 thoracic vertebrae which can be shadowed by the shoulders in a lateral view. An obliqued position (shoulders turned diagonally while pt’s head and body remain in the lateral view) can improve visualization of this part of the esophagus and trachea. Swallows are repeated with the fluoro tube lowered to the base of the cervical esophagus.
• Dysfunction: Tracheoesophgeal fistula
• Normal: TE or party wall is intact with no evidence of swallowed material entering soft tissue or airway
• Abnormal: a fistula tract allows food from the esophagus to backflow into the trachea
– Patients will have symptoms of aspiration (coughing after the swallow)
– If the MBSS is normal, an evaluation of the esophagus is recommended to r/o a TE fistula
• Tracheoesophageal fistula can result in aspiration after the swallow below the level of the glottis
Esophageal Phase
• Symptom: Round balloon that fills with radiopaque material as the pt swallows; usually empties after the swallow and can backflow into the pharynx or airway
• Dysfunction: Zenker’s Diverticulum
– Side pocket that forms when pharyngeal or esophageal muscle herniates
– Located in cricopharyngeal region/UES
– Why? Increased pharyngeal pressure is required to push bolus through a hypertonic UES, thus causing the tissue to herniate over time.
• Normal: bolus cleanly passes through UES
• Abnormal: material fills into herniated soft tissue during the swallow which may backflow into the pharynx or airway
• Zenker’s Diverticulum may result in backflow of swallowed contents into the pharynx or airway after the swallow
Figure 4.30
Gastroesophageal Reflux
• Backflow of food and stomach acid from the stomach to the esophagus
• 2/2 failure of LES to keep food in stomach
• May see redness in the arytenoid area during a laryngoscopy
• Pt may complain of a burning sensation in pharynx or esophagus, frequent gagging or coughing
• Aspirated material that contains any gastric acid is more irritating to the lungs than aspirated saliva or food.
• NOT diagnosed during a MBSS. If suspected, consult a
GI specialist.
Esophageal Phase
• Symptom: Reflux or Gastroesophageal Reflux
Disease (GERD)
• Dysfunction: LES dysfunction
• Normal: material enters stomach with no evidence of backflow
• Abnormal: material backflows from the stomach to the esophagus
• LES dysfunction results in reflux
Posterior-Anterior View
Examines symmetry of structures and function in the oral and pharyngeal cavity during swallowing and of the larynx during phonation.
Normal: bolus divides fairly equally to pass down the two-sides of the pharynx and esophagus in
80% of normal swallowers; 20% swallow unilaterally
– Difficulty to determine the occurrence and amount of aspiration 2/2 the trachea and esophagus overlapping each other.
Oral Preparatory Phase: A/P view
• A/P view allows SLP to examine:
– 1: tongue’s ability to lateralize material
– 2: pattern of jaw movement during mastication
– 3: shape of tongue during bolus holding with the sides of the tongue in contact with the lateral alveolus and the central groove midline surrounding the bolus
Oral Preparatory Phase: A/P view
• Symptom : Unable to align teeth/improper occlusion for chewing
• Dysfunction : Reduced mandibular movement/ROM
– Usually occurs when there has been removal of part of the mandible
• Normal: teeth align properly for mastication
• Abnormal: incomplete mastication
• Reduced mandibular ROM results in incomplete mastication 2/2 improper teeth occlusion for chewing
Oral Preparatory Phase: A/P view
• Symptom : Unable to lateralize material with tongue
• Dysfunction : Reduced tongue lateralization
• Normal: tongue moves food from side to side for chewing with teeth
• Abnormal: incomplete mastication of food
• Reduced tongue lateralization results in incomplete mastication of food 2/2 inability to move bolus between teeth
Oral Preparatory Phase: A/P view
• Symptom : Unable to mash material with tongue
2/2 inability to lateralize food to teeth for chewing
• Dysfunction : Reduced tongue elevation/ROM
• Normal: tongue mashes food to hard palate to compensate for poor lingual lateralization
• Abnormal: inability to mash food against hard palate
• Reduced tongue ROM results in inability to mash food against hard palate
Oral Preparatory Phase: A/P view
• Symptom : material falls into the lateral sulcus
• Dysfunction : Reduced buccal tension/tone
• Normal: Buccal tension/tone closes the lateral sulcus and prevents material from lodging there and directs bolus medially towards the tongue.
• Abnormal: Material falls into the lateral sulcus during mastication
– Decreased buccal tension/tone results in bolus collection within the lateral sulcus
Oral Preparatory Phase: A/P view
• Symptom : Material falls into the floor of the mouth
• Dysfunction : Reduced tongue control
• Normal: food is free from floor of the mouth during mastication
• Abnormal: food falling into the floor of the mouth during mastication
• Reduced tongue control results in material falling into the floor of the mouth during mastication
Oral Preparatory Phase: A/P view
• Symptom : Decreased bolus formation; Bolus spreads across mouth
• Dysfunction : Reduced lingual shaping and fine tongue control
• Normal: tongue shapes around bolus to hold cohesive
• Abnormal: bolus is spread throughout oral cavity
• Reduced lingual shaping and fine motor control results in decreased bolus formation
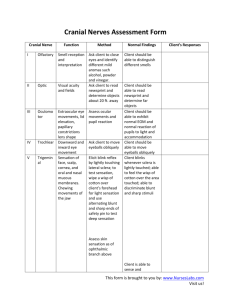
Pharyngeal Phase: A/P view
• Symptom : Unilateral vallecular residue
• Dysfunction : Unilateral dysfunction in posterior movement of the tongue base or the pharyngeal constrictors
• Normal: valleculae is free from residue
• Abnormal: food is left on only one side of the valleculae after the swallow
• Unilateral weakness in posterior movement of the tongue base or pharyngeal constrictors result in unilateral vallecular residue on the weak side
Figure 4.31
Pharyngeal Phase: A/P view
• Symptom: Residue in one pyriform sinus
• Dysfunction: Unilateral dysfunction of the pharyngeal walls
• Normal: pyriform sinuses are free from significant residue
• Abnormal: residue within the pyriform sinuses
• Unilateral weakness of the pharyngeal constriction results in residue on the weak side of the pyriform sinuses
Figure 4.32
Figure 4.33
(fairly symmetrical residue)
V
PW
PS
Pharyngeal Phase: A/P view
• Symptom: May cause aspiration during the swallow
• Dysfunction: Reduced vocal fold adduction
– can be evaluated when pt’s head is tilted backward, with the mandible out of view
– Ask pt to say “ah, ah, ah” rapidly to localize vf; then have pt inhale, prolong
“ah” for several seconds, and repeat.
– Look for symmetry with adduction and abduction
– Reduced movement of one side indicate possible unilateral vf paresis or paralysis
– May cause aspiration during the swallow 2/2 decreased airway closure
• Normal: vocal folds adduct completely during the swallow for airway protection
• Abnormal: Aspiration noted during the swallow; however if laryngeal closure is achieved above the level of the tvf, aspiration may not be witnessed.
• Reduced vocal fold adduction may result in aspiration during the swallow .
Pharyngeal Phase: A/P view
• Symptom:
• Dysfunction: Unequal height of vocal folds
Occasionally seen in partially laryngectomized patients
Reconstructed larynx on one side does not meet up with unoperated side during laryngeal closure even if both sides move well
• Normal: vocal folds adduct completely during the swallow
• Abnormal: two sides of larynx do not meet each other during laryngeal closure (incomplete closure)
– May result in aspiration during the swallow
Figure 4.34
• Questions?