Document
advertisement

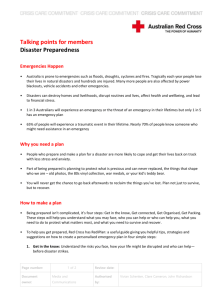
Monday January 25, 2016 Do Now: How do you improve your level of fitness? Learning Target: I can analyze a situation, overcome obstacles, and begin to enact the steps Check, Call, Care. Success Criteria: I am listening to instructions and following the demonstrations to correctly analyze and approach an injured person. First Aid/CPR Manual You will be creating a First Aid/CPR manual during this health unit. You will need 1 sheet of red paper and 10 sheets of white paper. First Aid/CPR Manual The front cover should include a title, a picture, and your name. The first page will be titled “Table of Contents” As we add information to our books make sure you update this table. Lesson 1 Before Giving Care and Checking an Injured or Ill Person Introduction Video Lesson 1: Before Giving Care Lesson Objectives: - Describe how to recognize an emergency - Describe the purpose of the Good Samaritan laws - Explain how to perform a “Scene Risk Assessment” - Identify how to reduce the risk of disease transmission when giving care - Explain how to check a conscious person for both life and non-life threatening conditions - Identify the signals of shock - Explain how to minimize the effects of shock - Explain how to check an unconscious person for life-threatening conditions. My First Aid Kit A good First Aid kit will have the essential items needed to care for most non-life threatening emergencies and general care. More complete kits will include materials and tools for life threatening emergencies. These are often carried by medical professionals such as EMTs, Paramedics, and Fire Fighters. Use page 19 of your classroom book to add the essentials into your manual. Overcoming Barriers Far too often people do not act as first responders because they are scared or nervous. What do you think are some common barriers that prevent bystanders from helping others? Common Barriers Panic or fear of doing something wrong Uncertainty of the person’s condition or what to do Assuming someone else will take action Type of injury or illness Fear of catching a disease or germs Fear of being sued Being unsure of when to call 9-1-1 What would you do? VIDEO Good Samaritan Laws The Good Samaritan Laws protect a responder from being sued for attempting to help. A reasonable and prudent person would: Only move a person if their life was in danger Ask a conscious person for consent before providing care Check for life-threatening conditions before giving care Call 9-1-1 Continue to provide care until emergency medical professionals arrive and take over Disease and Bodily Fluid Prevention When providing care for an injured person it is extremely important to protect yourself as well. Always wear gloves and keep hair tied back Wear face protection if needed ( safety glasses, masks, etc. ) Remove gloves and wash hands after helping victim Remove and wash clothes when possible Check Call Care Check the scene and person Call 9-1-1 for help or assistance Care for the person Check Always make sure that the scene is safe before entering! Checking a Conscious Person After checking if the scene is safe: Approach person Instruct them to stay still Introduce yourself and ask for consent Check for life threatening emergencies Begin Care Practice Questions Checking an Unconscious Person After checking if the scene is safe: Approach person Tap shoulder to check for consciousness If no response call 9-1-1 or instruct someone else to call Check for vital signs Look, Listen, Feel Begin Care Checking Unconscious Video Call After checking the scene for any danger and assessing the victim it is time to call for help. Call 9-1-1 if the injury is severe and requires a medical professional You can also instruct someone nearby to call while you provide initial care. Care After checking the scene and calling for help it is time to provide the initial care. If the victim is conscious ask them for details about the accident/injury to help you determine the appropriate care. If the victim is unconscious you need to Look, Listen, and Feel Look, Listen, Feel Look for bleeding, physical injury to the victim, or movement of the chest Listen for breathing and signs of life Feel for a pulse and breath from the nose/mouth Open the airway if needed Open the Airway Head Tilt Chin Lift Practice In groups of three we will practice the three C’s Check Call Care Tuesday January 26, 2016 Do Now: What are the first steps when approaching an injured person? Learning Target: I can analyze a situation, overcome obstacles, and begin to enact the steps Check, Call, Care. Success Criteria: I am listening to instructions and following the demonstrations to correctly analyze and approach an injured person. Lesson 2 Sudden Illness Lesson 2: Sudden Illness Lesson Objectives: - Identify the signals of common sudden illness - Describe how to care for common sudden illness - Describe how to care for someone who is having a seizure Sudden Illness Sudden Illness includes: Fainting Seizures Stroke Diabetic Emergencies Allergic Reactions Poisoning Signs and Symptoms Dizziness Trouble Breathing Nausea Headaches Diarrhea Changes in Consciousness Weakness Confusion Change in Body Temperature Fainting Fainting occurs when there is an insufficient supply of blood to the brain. Fainting results in a temporary loss of consciousness. When in doubt, call 911 if you are unsure of the person’s condition. Seizures Seizures are the result of abnormal electrical activity in the brain which causes temporary involuntary body movements, functions, behavior, etc. Call 911 immediately and wait with the person until help arrives. Do not try and restrain the person as you can cause even more damage. Stroke A stroke is caused by the loss of blood flow to the brain. Call 911 immediately if a stroke is suspected. F- Face A- Arms S- Speech T- Time Diabetic Emergency A diabetic emergency can be serious and life threatening as well. Diabetes is a condition where the body cannot process sugars into energy. Call 911 if the person becomes extremely week or loses consciousness. Allergic Reactions An allergic reaction is caused by the over activity of the immune system against antigens ( foreign substances ) Allergic reactions can range in severity from minor to lifethreatening. The victim will usually be able to tell you the details in order for you to provide appropriate care. Poisoning Poison is a substance that causes illness, injury, or death if it enters the body. Poisons can be inhaled, swallowed, absorbed, or injected. Call 911 if the person loses consciousness or experiences trouble breathing. Monday February 1, 2016 Do Now: What does FAST stand for when caring for a stroke victim? Learning Target: I can identify the signs of environmental emergencies and explain how to provide care. I can explain how to care for various soft tissue injuries. Success Criteria: I am listening to instructions and adding the important information into my First Aid Manual. Lesson 3: Environmental Emergencies Lesson Objectives: - Identify the signals of heat-related illness and cold-related emergencies - Describe how to care for heat-related illness and coldrelated emergencies Environmental Emergencies Environmental emergencies occur when a person is subjected to extreme conditions. People who work outdoors, elderly folks, and young children are most at risk. Heat Related Illness Cold Related Illness Heat Related Illness Heat related illnesses are caused by overexposure to heat and dehydration. This can lead to heat strokes, heat cramps, and heat exhaustion. Heat Cramps Heat cramps are painful muscle spasms usually occurring in the legs or abdomen. Care: Move to a cool place Give the person a sports drink or water Lightly stretch the cramped muscle and massage surrounding area Heat Exhaustion Heat exhaustion is fatigue caused by an overexposure to extreme heat. Signs: Cool, pale skin, headaches, nausea, dizziness, weakness, exhaustion. Care: Move person to a cool place Remove/loosen clothing Apply cool wet cloths Heat Exhaustion Care: Move person to a cool place Remove/loosen clothing Apply cool wet cloths Spray person with water or fan them Give the person small amounts of cool sports drink or water If condition does not get better or worsens call 911 Heat Stroke Heat stroke occurs when the body overheats and begins to stop functioning. Signs: Extremely high body temperature, red skin, changes in consciousness, vomiting, rapid weak pulse, rapid shallow breathing, confusion, seizures Heat Stroke Care: Call 911 as a heat stroke is life threatening Immerse the person in cold water or Douse or spray with cold water or Cover person with ice or Cover person in cold, wet towels Cold Related Emergencies Cold related emergencies are caused by overexposure to extreme cold conditions. This can lead to hypothermia and frostbite Frostbite Frostbite is the freezing of a body part that is exposed to the cold. The severity of frostbite depends on the temperature, length of exposure, and wind speed. Frostbite can lead to the loss of fingers, arms, toes, or legs. Signs of frostbite include cold skin, numbness in affected area, discolored skin (yellow, blue, or black). Frostbite Care: Always handle the affected area carefully. For minor frostbite warm the area with skin to skin contact. For more serious frostbite, gently soak affected area in water no warmer than 105 degrees. Let soak for 20-30 mins. Loosely bandage area with dry sterile dressings. Place cloth between frostbitten toes and fingers. Hypothermia Hypothermia is the lowering of the body’s core temperature to a point in which the body becomes impaired. Hypothermia can occur in even wet and windy environments. Signs of hypothermia include shivering, numbness, glassy stare, and loss of consciousness. Hypothermia Care: Call 911 if you suspect severe hypothermia. Move to a warm place, remove wet clothing, and dry person. Gradually warm the body by wrapping in blankets and plastic sheets to trap heat inside. Keep the head covered. Give person warm liquids. Lesson 4: Soft Tissue Injuries Lesson Objectives: - Identify signals of various soft tissue and musculoskeletal injuries - Describe how to care for various soft tissue and musculoskeletal injuries - Demonstrate how to control external bleeding Soft Tissue Injuries Soft tissue injuries include both open and closed wounds. When caring for open wounds be sure to always wear gloves and eye wear if you suspect the blood to spray/splatter. Bruises A bruise is caused by impact to the body and results in ruptured blood cells collecting under the surface of the skin. Bruises will often turn black and blue as they heal. To treat a bruise apply ice and have your mommy kiss it. Nosebleeds A nosebleed is the of a blow to the head or face. Most nosebleeds are not serious and can be treated in minutes. To stop the bleeding lean head slightly forward and pinch the upper nostrils for 10 minutes. If bleeding still continues press firmly on the upper lip while pinching nostrils. Nosebleeds A nosebleed is the of a blow to the head or face. Most nosebleeds are not serious and can be treated in minutes. To stop the bleeding lean head slightly forward and pinch the upper nostrils for 10 minutes. If bleeding still continues press firmly on the upper lip while pinching nostrils. Cuts and Scrapes Cuts and scrapes are open wounds and require special treatment. Always wear gloves when dealing with open wounds. Cover the wound with a dressing and apply pressure until bleeding stops. Apply a bandage over the dressing and wrap firmly. If bleeding seeps through bandage do not remove, just add more dressings and bandages. Stitches are required for deep or wide cuts. Burns Burns are classified by their depth. The deeper the burn, the more serious it is. Call 911 if the person with the burn: Has trouble breathing. Has burns covering more than one body part or a large portion of the body. Has burns to the head, neck, hands, feet, or genitals. Tuesday February 2, 2016 Do Now: How do you care for a person with heat exhaustion? How do you care for someone with hypothermia? Learning Target: I can identify the signs of environmental emergencies and explain how to provide care. I can explain how to care for various soft tissue injuries. Success Criteria: I am listening to instructions and adding the important information into my First Aid Manual. Lesson 5: Injury to Muscles, Bones, and Joints Lesson Objectives: - Identify signals of head, neck, and spinal injuries Explain how to care for muscle, bone, or joint injuries Explain how to care for head, neck, and spinal injuries Explain how to care for muscle, bone, or joint injuries Injury to Head, Neck, and Spine Although injuries to the head, neck, and spine account for only a small fraction of all injuries, they can cause neurological damage or even death. The head holds the most important organ in the body, the brain. The spine travels from the head to the lower back and provides support for the rest of the body. When caring for someone with a suspected injury to the head/neck/spine keep the person still. Ask for verbal answers, no head shaking. Injury to Head, Neck, and Spine Care: If you find someone with a head/neck/spine injury do not move them. Keep the head in the position you found it. Try to stabilize and support the head in place. Do not remove any helmets, hats, or face shields from the person. Get professional help - 911 Concussions Concussions are brain injuries caused by a blow to the head or the rapid shaking of the head and body. Concussions can be life threatening if not treated correctly. There are multiple levels of seriousness which require different rehabilitation. Stop all physical activity and seek medical help immediately if you suspect a person to have a concussion. Concussions Signs: Confusion Headache Memory Loss Loss of Consciousness Nausea Speech Problems Blurred Vision or Light Sensitivity Concussions Care: Remove from activity Question the person ( name, location, date, repeat sentences ) Stay in front of the person at remain at eye/head level Watch closely Seek medical help Wednesday February 3, 2016 Do Now: How do you treat a concussion? Learning Target: I can correctly diagnose an injury and create a splint/sling to support that injury. Success Criteria: I am using my textbook as a guide for teaching me to splint an injured limb. Splinting Splinting is used to support a broken limb for transport to a medical facility. The main types of splints include: Anatomic Splint Soft Splint Rigid Splint Sling and Binder Anatomic Splint Textbook Page 142-143 Soft Splint Textbook Page 144-145 Rigid Splint Textbook Page 146-147 Sling and Binder Textbook Page 148-149 Friday February 5, 2016 Do Now: How do you create an anatomic splint? Learning Target: I can correctly identify the signs of choking and take steps to help the choking person. Success Criteria: I am practicing my moves while paying attention to my instructor. Lesson 6: Breathing Emergencies Lesson Objectives: - Recognize the signals of a breathing emergency - Demonstrate how to care for a person who is choking Breathing Emergencies A breathing emergency occurs when a person is having trouble breathing or cannot breathe at all. Can be caused by injury, illness, or disease. If untreated these emergencies can turn into cardiac emergencies. Breathing Emergencies SignalsNoisy Breathing Rapid or Slow Patterns Unusually moist or cool skin Dizziness or Light-Headed Pain in Chest Tingling in hands, feet, or lips Apprehensive feelings Breathing Emergencies Common Causes- Choking Illness Asthma Electrocution Irregular Heartbeat Heart Attack Injury to head, neck, back, or chest Allergic Reaction Drug Overdose Drowning Breathing Emergencies More Causes- Trying to swallow large pieces of food Drinking alcohol before or during meals ( dulls nerves that aid in swallowing ) Wearing dentures Eating while talking or laughing Eating too fast Walking or playing with food in mouth Putting things that don’t belong in your mouth Being stupid Breathing Emergencies Common Killers- Round, firm foods like hotdogs and carrots Hard, gooey, or sticky candy Grapes Popcorn Chewing Gum Vitamins Marbles Coins Pen/Marker caps Small Batteries Breathing Emergencies CareTalk to the person ( If they can speak they can breathe ) Encourage person to continue coughing Back Blows Heimlich Maneuver ( Abdominal Thrust ) Back Blows 1- Bend person over at waist 2- Stand to side 3- Using palm thrust down and forward on mid-back Abdominal Thrust 1- Stand behind person 2- Reach around and locate belly button 3- Place back of thumb just above belly button 4- Make a fist and grab your fist with other hand 5- Thrust fists upward into abdomen Breathing Emergencies Care for Unconscious Person Open the Airway Look, Listen, Feel 911 Chest Compressions ( 30 ) Look for Object Rescue Breaths