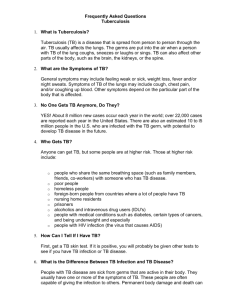
Tuberculosis
Tuberculosis
Pearly disease
• Definition: Tuberculosis (TB) is an infectious, granulomatous disease of mammals including human, caused by acid-fast bacilli of the genus Mycobacterium, characterized clinically by progressive development of primary nodular granulomas known as tubercles (caseous nodules) in lungs and pulmonary lymph nodes and disseminated caseous nodules in internal organs.
• Any body tissue can be affected but lesions are frequently observed in lymph nodes (particularly of head and thorax), lungs, intestine, liver, spleen, and pleura. Clinical signs depend on the involved organs
Etiology
• Three main types of tubercle bacilli are recognized: human, bovine, and avian, respectively, M. tuberculosis , M. bovis , and M. avium complex ( M. avium-intracellulare-
scrofulaceum ). The 3 types differ in cultural characteristics and pathogenicity.
• M. bovis can cause progressive disease in most warm-blooded vertebrates, including humans.
• Skin tuberculosis of cattle is caused by M. fortuitum but skin tuberculosis of sheep and goats is due to the infection with M. bovis. There is a cross antigenic reaction among the members of this group also with other organisms such as Corybacterium, Nocardia and Rhodococci
• Morphology and staining:
▫ Mycobacteria are Gram positive, acid fast, no motile and non spore forming small rods. They can be stained by acid-fast stain or Ziehl-Neelsen stain
(appear red color).
• Growth requirements and characteristics:
▫ Mycobacteria grow well but slowly on
Lowenstein-Jensen slants and egg yolk agar with incubation under aerobic conditions at 33-39 ° C for up to 8 weeks. Colonies are dry, delicate, dome-shaped (avian type) and crumbly
(mammalian type).
Epidemiology:
1.
Distribution: The disease is worldwide distributed and endemic in Egypt.
2.
Animal susceptible:
▫ The disease affects all species of vertebrates.
Cattle, buffaloes, pigs and humans are highly susceptible. Sheep, goats, camels and equines are sporadically affected.
• Factors effect on susceptibility:
▫ The disease is more common in dairy cattle than in fattening cattle due to the long life span of dairy cattle. Also, the incidence of the disease is high in old animals.
▫ It is of low prevalence in cattle kept on pasture.
The indoor housed animals are at high risk of the infection due to aerosol transmission.
▫ Stress factors as repeated pregnancy, lactation, debilitating factors (poor feeding, chronic disease), close housing and poor ventilation.
3. Transmission:
• Source of infection:
▫ Infected cattle are the main source of infection for other cattle. Organisms are excreted in the exhaled air, in sputum, feces, milk, urine, vaginal and uterine discharges, and discharges from open peripheral lymph nodes.
• Mode of transmission:
▫ Commonly entry is affected by inhalation or ingestion.
▫ Inhalation is the almost invariable portal of entry in housed cattle
▫ by ingestion is possible at pasture when feces contaminate the feed and communal drinking water
▫ The drinking of infected milk by young animals
▫ Other uncommon routes of infection include intrauterine infection at coitus, by the use of infected semen
▫ intramammary infection by the use of contaminated teat siphons
Pathogenesis
• Tuberculosis spreads in the body by two stages, the primary complex and postprimary dissemination.
• The primary complex consists of the lesion at the point of entry and in the local lymph node, especially when infection is by inhalation.
• More commonly the only observable lesion is in the pharyngeal or mesenteric lymph nodes. A visible primary focus develops within 8 days of entry being affected by the bacteria. Calcification of the lesions commences about 2 weeks later. The developing necrotic focus is soon surrounded by granulation tissue, monocytes, and plasma cells and the pathognomonic
'tubercle' is established.
• Bacteria pass from this primary focus, which is in the respiratory tract 90-
95% of cases, to a regional lymph node and cause the development of a similar lesion
Pathogenesis
• Post-primary dissemination from the primary complex may take the form of acute military tuberculosis, discrete nodular lesions in various organs, or chronic organ tuberculosis caused by endogenous or exogenous reinfection of tissues rendered allergic to tuberculoprotein.
• In the latter case there may be no involvement of the local lymph node.
• Depending upon the sites of localization of infection, clinical signs vary, because the disease is always progressive, there is the constant underlying toxemia which causes weakness, debility, and the eventual death of the animal.
Clinical signs
• The incubation period is long and varied from 2 months to several years. Morbidity and mortality rates are generally low (5-20%) and depend on the rearing system.
• General signs:
▫ Most cases progressive emaciation unassociated with other signs occurs, and should arouse suspicion of tuberculosis. A capricious appetite and fluctuating temperature are also commonly associated with the disease. Affected animals tend to become more docile and sluggish. These general signs often become more pronounced after calving.
• Specific signs:
• Pulmonary involvement:
▫ Pulmonary involvement is characterized by a chronic cough due to bronchopneumonia. The cough is never loud occurring only once or twice at a time. It is easily stimulated by squeezing the pharynx or by exercise and is most common in the morning or in cold weather.
▫ In the advanced stages when much lung has been destroyed, dyspnea with increased rate and depth of respiration becomes apparent. At this stage, abnormalities may be detected by auscultation and percussion of the chest. Areas with no breath sounds and dullness on percussion are accompanied by areas in which squeaky crackles are audible.
▫ Involvement of the bronchial lymph nodes may cause dyspnea because of constriction of air passages, and enlargement of the mediastinal lymph node is commonly associated with recurrent and then persistent ruminal tympany.
• Alimentary tract involvement:
▫ Rarely tuberculous ulcers of the small intestine cause diarrhea. Retropharyngeal lymph node enlargement causes dysphagia and noisy breathing due to pharyngeal obstruction. Pharyngeal palpation, or endoscopy, reveals a large, firm, rounded swelling in the dorsum of the pharynx. Chronic, painless swelling of the submaxillary, prescapular, precrural, and supramammary lymph nodes is relatively rare.
• Genital system:
▫ There is tuberculous metritis, there may be infertility, or conception may be followed by recurrent abortion late in pregnancy, or a live calf is produced which in most cases dies quickly of generalized tuberculosis.
▫ . Rare cases of tuberculous orchitis are characterized by the development of large, indurated, painless testicles.
• Udder involvement (tuberculous mastitis):
▫ it has characteristic feature is a marked induration and hypertrophy which usually develops first in the upper part of the udder, particularly in rear quarter.
In the early stages, the milk is not macroscopically abnormal but very fine floccules appear later and settle after the milk stands, leaving a clear, amber fluid. Later still the secretion may be an amber fluid only.
• Lymphatic involvement:
▫ There is chronic painless swelling in the affected lymphnodes as submaxillary, prescapular, prefemoral and supramammary. These lesions may be unilateral or bilateral. The affected lymph node may be containing fistula or discharging duct.
• Brain involvement:
▫ In young calve; tuberculosis meningitis with nervous manifestation may develop.
• Skin involvement:
▫ Skin lesions appear as nodules similar to small hard cauliflower on skin of the neck, shoulder and upper forelegs. These lesions may involve the lymphatics.
Postmortem lesions:
• Carcass is emaciated. Tuberculous nodules may be found in many organs and lymph nodes especially bronchial and mediastinal lymph nodes.
• In lungs, there is bronchopneumonia and military abscesses.
• Pus is creamy to orange in color and varies in consistency from thick cream to crumbly cheese.
• Small nodules may be found on pleura and peritoneum.
• Closed lesions are characteristically discrete nodules containing thick yellow to orange caseous materials. They are often calcified and surrounded by thick capsules.
Diagnosis
• Field diagnosis: It is depend on history of area where TB is endemic or not, clinical signs such as progressive emaciation and chronic cough, postmortem lesions and zoonotic implications.
In living animal TB can be diagnosed by allergic field tuberculin test.
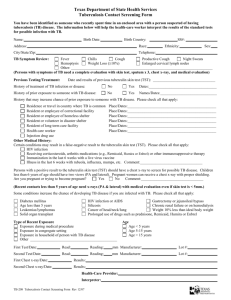
Tuberculin test
• The standard method for detection of bovine tuberculosis is the tuberculin test, which involves the intradermal injection of bovine tuberculin purified protein derivative (PPD) and the subsequent detection of swelling (delayed hypersensitivity) at the site of injection 72 hours later
Types of tuberculin test
1.
Single intradermal test (SID):
▫ it can be applied on calves more than 6 months of age. This test can be detecting more than 90% of infected animals.
▫ Indication: It can be used as an initial test in unknown herds, in case of the suspected reactors and in the introduction of animals from free herds.
▫ Procedure:
▫ Dose: 0.1 ml in unknown status herd and 0.2 ml for infected one
▫ Site: ID middle part of the neck or mucocuataneous J as anal or caudal fold of base of the tail (england)
• Result: read result after 48 (for max. sens.)-96 h
(for max. specf.)
▫ Increase thickness of skin more than 4mm, +ve
▫ Increase thickness 3-4 mm, doubtful
▫ Increase thickness 1-2 mm, -ve
Disadvantage:
Lack of specificity, can not differentiate between pathogenic and non pathogenic TB
Non of non visible lesion reactors exceed 10%
False (-ve) with min. sensitized animals;
Early stage of infection
Late stage of infection
Old animal
Recent parturition
• False positive result with;
▫ Non pathogenic mycobacterium (Avium, paratuberculosis, Neocadia)
▫ Animal vaccinated with BCG vaccine within 8-60 d post vaccination
▫ Recent born calve suckling milk of infected dam during first 3 w after parturition
Single intradermal comparative (SIDC) test:
• The test used to differentiate between infection due to pathogenic TB and non pathogenic mycobacterium
(avian, paratuberulosis)
• Procedure; Avian and bovine tuberculin are injected simultaneously into two separate sites on the same side of the neck, 12 cm apart and one above the other, and the test is read 72 hours later
• Result;
▫ increase thickness of skin more than 3 mm indicate positive for homologous organism which responsible for reaction
Short Thermal Test
• It has a high efficiency in the detection of spreaders that give negative result with SID
• Dose,
▫ 4 ml S/C, The body temp. of examined animal must be normal during and 2 h after injection.
• Result;
▫ read the result after 4, 6 and 8 h
Increase body temp 1 C , indicate +ve
Normal body temp, indicate –ve
• Advantage
▫ It can be detect min sensitized animals.
• Disadvantage:
▫ Anaphylactic shock due to large dose of PPD
Stormont test
• This test has a highly efficiency in the detection and selection of the poorly sensitized animals especially cows that have calved recently.
• Dose; 0.1 ml I/D in middle part of cervical region and repeat after 7 days in the same site
• Result, read after 24 h fro 2 nd injection, increase of thickness more than 4mm indicate +ve result
• Disadventages;
▫ It causes long period of desensitization, laborious and needs three visits to the farm, need special PPD with specified potency.
• Post-parturient desensitization:
▫ It occurs immediately before and after parturition, the loss of sensitivity may be due to removal of the fixed cells antibodies from skin to general circulation then to colostrums. On the other hands, colostral antibodies cause false positive result in calve for up to 3 weeks.
• Anergic animals:
• Those animals are with visible lesion of TB but not react with the cutaneous test. Those anergic animals can be reduced by the inoculation of sufficient amount of PPD and read the results at
48-72 hours.
Laboratory Diagnosis:
• Samples: nasal discharges, sputum, trachobronchial and gastric lavage, discharges of the reproductive tract, lymph nodes, thoracic and abdominal fluid, milk, urine, feces and samples from organs (liver, kidney, lung and reproductive organs), blood, serum.
• Procedures:
1.
Direct microscopic examination for tissue and organ smear after staining with Ziehl Neelsen acid fast stain.
2. Isolation and identification of the organism: the organism grows on Lowenstein media at 37°C for 6 w.
Identification of the colonies can be done on the basis of culture characteristics, morphology, staining and biochemical reaction. It is important to know that detection of the organism is not sufficient by culture.
Also, negative culture results do not mean that the animal is free of infection.
3. Serological examination:
Various serological examinations can be applied such as ELISA (gives some false positive results but it picks up some carriers that missed by SID),
FAT (of great value in detection of some cases that gave false negative results with tuberculin but it failed to detect high number of tuberculous cattle), the gamma interferon test (it detects specific lymphokines produced by lymphocytes due to the response to the organism and can be used with SID).
4. Lung radiograph: it can be used to detect the lung nodules.
5. PCR: It is rapid and sensitive. It can detect even one tubercle bacillus in the suspected material.
Treatment
• Because of the progress being made in the treatment of human tuberculosis with such drugs as combinations of streptomycin and para aminosalicylic, and other acids
Control
• The control depends on the identification of the infected animals by tuberculin test and elimination of the positive cases by slaughter
I.
Control on herd basis:
▫ Control in a herd depends on:
1. removal of the infected animals,
2. prevention of spread of infection, and
3. avoidance of further introduction of the disease.
1.
Detection and removal of infected animals:
▫ control is applied by careful and regular clinical examination and tuberculin testing of all animals above 3-6 months every
6 months and then immediate culling (slaughter) of the reactors.
▫ Doubtful cases should be isolated and retested after 2 months.
▫ SIDC test should be used if there is high incidence of infection with human or avian types
▫ If there is a high incidence of reactors at first step of examination or if open lesions were observed in culled animals at PM examination, the test should be repeated at short intervals (2-3 months) till negative results are obtained and then another confirmatory test should be applied after 6 months.
▫ If last test gives negative results, herd is considered free from
TB and should be tested annually.
2. Prevent spread of infection and avoidance of further introduction of disease:
▫ Hygienic measures to prevent the spread of infection should be instituted as soon as the first group of reactors is removed.
▫ Feed troughs should be cleaned and thoroughly disinfected with 5% phenol . Water troughs and drinking cups should be emptied and similarly disinfected.
▫ Separation of infected and susceptible animals by a double fence provides practical protection against spread of the disease.
▫ It is important that calves being reared as herd replacements be fed on tuberculosis-free milk
▫ After Culling of the reactors, the replacement animals should be from free herd
II. Control on an area basis:
▫ The incidence and distribution of the disease should be defined by tuberculin testing of samples of cattle along with the good meat inspection in abattoirs to detect the free areas, low incidence and high incidence areas.
▫ In the low incidence areas, disease should be eradicated by test and slaughter policy.
▫ In the high incidence areas, it is impossible to apply the routine test and slaughter policy. These areas should be divided into infected and non-infected herds on basis of clinical examination and tuberculin test and so on to reduce the infected area
III. During outbreaks of TB:
▫ The clinically infected herds should be isolated.
Infected animals should be slaughtered and subjected to pathological examination. The herd should be monitored with elimination of the reactors every 3 months and then every 6 months for several years. Farms should be carefully cleaned and disinfected. The source of the infection should be investigated.