Open Forum & Case Consultation - University of Nevada School of

9 million doctor visits/year!
Customary urine test is the dip stick and the mid-stream culture of voided urine. Up to 77% of cystitis cases are cultured
Traditionally- >100,000 (10⁵)CFUs was called diagnostic of either
UTI (bladder infection present) or asymptomatic bacteruria.
More recently as little as 100 CFUs in a voided sample has been positively correlated with coliform (such as E. coli ) bladder infection
The problem with this cut off: Many labs will call 0 to 10,000 CFUs
(<10⁴) as a negative culture
The way the urine test is done, diluting out the urine 1000 times, there may be no growth on the agar plates despite a bladder infection being present
What does the results of the urine culture tell you ?
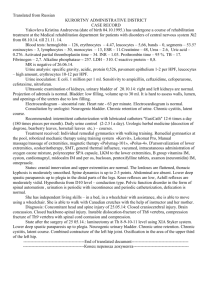
202 paired samples of mid stream collected urine cultures and catheterized bladder cultures in young woman who had symptoms of uncomplicated cystitis, no features of pyelonephritis
70% of bladder cultures positive
78% of voided mid-stream cultures positive
As few as 10 CFUs of mid-stream cultures of E. coli or Klebsiella pneumoniae– highly correlated with a true bladder infection ( 93% PPV).
In contrast – 22% of mid- stream cultures grew enterococcus or Group B strep- at even 100,000 (10⁵
CFUs) – there was no correlation with bladder cultures- These bugs were not found in the corresponding bladder culture, but E.coli was still cultured in the bladder (but not in the mid-stream culture) in 62% of these cases !
Take Home Message:
I. a young woman with classic cystitis symptoms can have a documented bladder infection, but her midstream urine culture can still be a false negative test ( too few CFUs to be detected on standard urine cultures)
II. Positive mid-stream cultures for enterococcus and Group B strep are most likely contaminants
III. In uncomplicated cases- obtaining cultures as a guide to therapy can be counter productive: either not treating patients with actual infection, or treating patients for the wrong bacteria.
Ask the patient “do you feel like you have a bladder infection- do you have both a sense of urgency and burnig when you urinate?”
Do a dip stick and treat only if leukocytes or nitrite positive?
Send the urine for culture, wait 2 days, and treat the patient only if >100,000/ml colonies
Symptoms only: +dysuria, +frequency, no discharge or irritation:*** 90% chance of cystitis***
Dipstick: leukocyte esterase + and/or nitrite + only 75% sensitive , so symptoms more important even if dip is negative
Culture:10⁵ (100,000) bacterial CFU- traditional criterion of
UTI50% sensitive -will miss up to half of cases of UTI – counts of 100 to 10,000 colonies – all at levels that may be called as “no growth” by micro lab. Least sensitive diagnostic test
**Rarely progresses to severe disease even if untreated: goal is to ameliorate symptoms
In selecting therapy, efficacy as well as “ecologic collateral damage” (selecting for antibiotic resistant bacteria, C. difficile colitis) should be considered equally- fluoroquinolones should be avoided, except in pyelonephritis
Nitrofurantoin , Septra , fosfomycin are therefore first line agents
New Study- still >50% of Rxs are for Cipro, most of the time for > than 3 days. Septra #2, nitro #3 , fosfomycin-no Rx
Definition: presence of bacteria >100,000 cfu/ml in urine of an individual without signs or symptoms of UTI.
This definition is independent of the presence or absence of pyuria, odor, cloudy urine
Very Common: i. Young healthy women : 3 to 5%
i.
ii.
iii.
Pregnant women: 2 to 9.5%
Women aged 65-80 years: 18 to 43%
Women > 80 years: up to 43%
iv.
Men 65-80 years: 2 to 15%
Causes:
Obstructive uropathy, neuromuscular disease, perineal soiling in dementia, etc
Traditional teaching: the presence of bacteriuria defines a population at risk, therefore:
Eliminating the “asymptomatic UTI” (oxymoron) minimizes the risk for a clinically symptomatic disease
Modern Teaching:
NO benefit to treatment (except in pregnancy and before urologic procedure). Term changed to
“asymptomatic bacteriuria”
3 to 5% of young women have ABU
What role does this have in recurrent UTI’s? Many women get follow-up urine studies and re-treatment after initial therapy for UTI.
Study in Clinical Inf. Disease 9/15/2012:
673 healthy non-pregnant woman followed after first UTI for one year.- all were treated again at any time if had symptomatic UTIs. urine cultures were also obtained at 3, 6 and 12 months-if positive but if patient asymptomatic only half were treated, other half were not
Results after one year of observation:
Those treated for ABU - 46.8% had a symptomatic UTI later during the year
Those not treated for ABU - only 13.1% had another UTI!
Conclusion: The paradoxical result was increased incidence of symptomatic UTIs in patients given antimicrobials for asymptomatic bacteruria!
Bacterial interference- the inability of pathogenic bacteria to set up a bladder infection due to blockage by commensal bacteria colonizing the bladder- was disrupted by the treatment of ABU.
Conclusion : The human microbiome is a potent defense mechanism against superinfecting pathogenic bacteria . Applies to the bladder, as well as the GI tract and other sites.
Antibiotic treatment of ASB does not reduce frequency of symptomatic UTI
Treatment of ASB in diabetes does not reduce adverse outcomes, improve glucose control, or reduce symptomatic
UTIs
It does lead to untreatable drug resistant bacteria, c.diff
,etc
Only exceptions are pregnancy where asymptomatic bacteriuria is associated with pyelonephritis, growth retardation, neonatal death… and patients undergoing urologic procedures (such as prostate bx)
Many older patients get screening u/a’s and reflex cultures even when they don’t have urgency and burning symptoms. They are then treated for a “UTI”. This is a too common mistake…
“older patients should not be tested or treated for UTI unless they have symptoms”
If you are treated for a true UTI: no follow-up test of cure should be performed
Antibiotics: have side-effects can cause future problems like yeast infection and colitis lead to drug resistant bacteria are a waste of money
Think twice before ordering a urine culture- go by symptoms and signs. Only culture in possible pyelonephritis, unclear diagnosis, complicated cases or treatment failure
Consider Macrodantin or Septra as first line therapy, quinolones if they are ill
Mid-stream culture results with enterococcus and GBS can be deceiving – rarely cause of UTI. Most likely still E. coli
If the patient is asymptomatic –if it ain’t broke, don’t fix it!