ICD-10 - Oklahoma Chiropractors' Association

ICD-10 Boot Camp
On Behalf of:
Oklahoma Chiropractors Association
Presented by: David Klein CPC, CHC & Evan M.
Gwilliam, MBA DC
CPC CCPC NCICS CCCPC CPC-I MCS-P CPMA
Sponsored by:
1
Objectives
•
Gain a basic understanding of ICD-10
•
Understand the reason for the transition
•
Identify the similarities and differences from ICD-9
•
Get familiar with relevant guidelines
•
Learn how to select the right codes
•
Learn how to document properly
•
Know how to implement ICD-10
•
Reduce ICD-10 related anxiety
2
Recommended Tools
ChiroCode’s Complete and Easy ICD-10 Coding for Chiropractic
Inside you will find:
• Comprehensive list of relevant ICD-
10-CM codes for Chiropractic (~15,000 codes)
• Tools to help you convert from ICD-9-
CM to ICD-10-CM o GEMs code map o Commonly used codes o Alphabetic index
• Complete guide to understanding
ICD-10-CM coding
• Other aids you need for a painless transition.
3
Recommended Tools
You could also use the complete code set (~68,000 codes), available from multiple publishers
4
Disclaimer
Every attempt has been made to make this presentation as current as possible, but things change
Be sure to check with your local carriers and
Medicare for updates as the
ICD-10 implementation date gets closer
Subscribe to
ChiroCode alerts or follow
ChiroCode on Twitter for updates that pertain to DCs
5
The Landscape
6
The Landscape
7
CMS-1500 Claim form
• Approved for official use 08/05
• www.nucc.org
for official instructions
8
9
CMS-1500 Claim form
Revision 02/12
• Changed to match the electronic format (5010) and ICD-10 codes
• Adds space for eight more diagnosis codes in box 21.
• January 6 th , 2014 - Health plans and clearinghouses must accept the form.
• April 1 st , 2014 – Providers must use the new form
10
Why do we have diagnosis codes?
•
•
•
•
•
•
HIPAA requirement
Establish medical necessity
Process claims
Translate written terminology into common language
Provide data for statistical analysis
Identify fraud, set healthcare policy, measure quality
11
Where did they come from?
• ICD-9 was developed by the World Health
Organization for public health and statistical analysis
• First revision 1893, ninth revision 1979 o Shifted focus from mortality to morbidity
• “ICD-9-CM” means Clinical Modification - for use with health care claims in the U.S.
• ICD-9-CM was mandated in 1988 under the
Medicare Catastrophic Coverage Act, then reaffirmed by HIPAA in 1996
12
How do I know which codes to use?
•
•
4.
Follow payer guidelines for code sequencing.
Diagnosis code hierarchy:
1.
2.
3.
Neurological
Structural
Functional
Soft tissue
For example, sciatica ( 724.3
) and DDD ( 722.4
) will carry more weight than spasm ( 728.85
) or myalgia ( 729.1
)
It is said that some software only looks at the first diagnosis when adjudicating a claim, so make it count!
13
How do I know which codes to use?
Medicare Universal Diagnosis List:
Short term (approximately 6-12 treatments)
• 721 Spondylosis
• 723-724 Back Pain
Moderate term (approximately12-18 treatments)
• 353 Root lesions
• 722 Unspecified disc disorders
• 724 Stenosis
• 846-7 Sprains
Long term (approximately18-24 treatments)
• 722 Degeneration, displaced discs
14
How do I know which codes to use?
Do not code the “kitchen sink”. Example:
• 847.0 Sprain of neck
• 723.4 Brachial neuritis or radiculitis NOS
• 739.1 Nonallopathic lesions, cervical region
• 728.4 Laxity of ligament (cervical)
• 728.85 Spasm of muscle (cervical)
• 729.1 Myalgia and myositis, unspecified
• 847.1 Sprain of thoracic
• 724.4 Thoracic or lumbosacral neuritis or radiculitis, unspecified
• 739.2 Nonallopathic lesions, thoracic region
• 728.4 Laxity of ligament (thoracic)
• 728.85 Spasm of muscle (thoracic)
• 719.7 Difficulty in walking
• 784.0 Headache
• 780.5 Sleep disturbances
15
How do I know which codes to use?
• Are all of these codes medically indicated by the patient’s records?
• Are any of the rendered codes merely symptoms of other codes?
• Are the rendered codes as accurate and precise as possible, given the supporting medical documentation?
16
Why can’t we keep using ICD-9?
•
•
•
•
•
Too old
Many sections are full and cannot be expanded
Not descriptive enough
Not able to accurately reflect advances in medical knowledge or technology
Will not meet healthcare needs of the future
17
Why can’t we keep using ICD-9?
•
•
Requires excessive reliance on supporting paper documentation
Hampers the ability to compare costs and outcomes
18
Why can’t we keep using ICD-9?
ICD-9
~14,000 codes
ICD-10
~68,000 codes
19
Will Oct. 1, 2014 be the end of the world?
21
Where did ICD-10 come from?
• The World Health Organization issued the tenth revision of the International Classification of
Disease (ICD-10) in the early 90’s.
o Each country is responsible for adapting ICD-10 to suit its needs
• Australia uses ICD-10-AM
• Germany uses ICD-10-GM
• Canada uses ICD-10-CA
• United States uses ICD-10-CM o U.S. has used ICD-10 since 1999 to report mortality data on death certificates
22
Where did ICD-10 come from?
• ICD-10-CM (CM=Clinical Modification) was developed by the National Center for Health
Statistics for reporting morbidity and mortality in the U.S.
o Ready in 1994 o Public comments 1997-1998 o Tested in 2003 by AHA and AHIMA o Final rule for implementation published 2009 o Postponed in 2012 o Implementation October 1, 2014 (for sure, maybe)
23
Won’t they just postpose it again?
24
Won’t they just postpone it again?
•
Jan. 2013, the AMA asked CMS to abandon
ICD-10
•
Feb. 6, 2013, CMS Acting Administrator,
Marilyn Tavenner said no
o Too much work has already been done to turn back now o The old system won’t work with new technologies o That would penalize innovators o It is necessary for health care reform
25
Won’t they just postpone it again?
•
•
•
•
•
•
ICD-10 does a better job than ICD-9 with:
Providing data for statistical analysis
Measuring quality and outcomes
Helping to set healthcare policy
Identifying public health threats
Identifying fraud and errors
Exchanging data among health care entities
In other words, we need it to improve our health care system.
26
How are ICD-9 and ICD-10 similar?
•
Still a tabular list divided into chapters based on body system or condition
•
Similar hierarchy
•
Still an index with main terms and sub-terms
•
Must code to the highest level of specificity
•
ICD-10 is mandated under HIPAA
27
How are ICD-9 and ICD-10 similar?
Conventions are mostly the same
(page 467)
NEC “Not elsewhere classified”
Used when the information in the medical record provides detail for which a specific code does not exist
NOS “Not otherwise specified” or “unspecified”
Used when the information in the medical record is insufficient to assign a more specific code.
28
How are ICD-9 and ICD-10 similar?
Conventions are mostly the same
(page 467)
[ ] Brackets are used in the tabular list to enclose synonyms, alternative wording or explanatory phrases.
Brackets are used in the Index to identify manifestation codes
( ) Parentheses are used in both the Index and Tabular to enclose supplementary words that may be present or absent in the statement of a disease or procedure without affecting the code number to which it is assigned. The terms within the parentheses are referred to as nonessential modifiers
29
How are ICD-9 and ICD-10 similar?
Conventions are mostly the same
“Includes”
This note appears immediately under a three-digit code title to further define, clarify, or give examples of the content of a code category.
“And”
The word “and” should be interpreted to mean either
“and” or “or” when it appears in a title… “either or”
30
How are ICD-9 and ICD-10 similar?
Conventions are mostly the same
“Excludes”
Excludes1 – is used when two conditions cannot occur together or “NOT CODED HERE!” Mutually exclusive codes; two conditions that cannot be reported together.
Excludes2 – indicates “NOT INCLUDED HERE.”
Although the excluded condition is not part of the condition, it is excluded from, a patient may have both conditions at the same time. The excluded code and the code above the excludes can be used together if the documentation supports them.
31
How are ICD-9 and ICD-10 similar?
Conventions are mostly the same
“Code First/Use additional code”
Provides instructions on how to “sequence” the codes.
Signals that that an additional code should be reported to provide a more complete picture of the diagnosis.
“Code Also”
Alerts the coder that more than one code may be required to fully describe the condition. The sequencing of the codes depends on the severity and/or the reason for the encounter.
32
How are ICD-9 and ICD-10 similar?
ICD-9
I. Official Guidelines (about 30 pages)
II. Indexes i.
Diseases and Injuries (300 pages) i.
Neoplasms (20 pages) ii. Drugs and Chemicals (30 pages) iii. External Causes (20 pages)
33
How are ICD-9 and ICD-10 similar?
ICD-10
I. Official Guidelines (about 30 pages)
II. Indexes i.
Diseases and Injuries (340 pages) ii. Neoplasms (20 pages) iii. Drugs and Chemicals (50 pages) iv. External Causes (35 pages)
34
How are ICD-9 and ICD-10 similar?
ICD-9
III. Tabular list
(340 pages)
1. Infectious Diseases
2. Neoplasms
3. Endocrine
4. Blood
5. Mental
6. Nervous
7. Circulatory
8. Respiratory
9. Digestive
10. Genitourinary
11. Pregnancy
12. Skin
13. Musculoskeletal
14. Congenital malformations
15. Perinatal
16. Signs and Symptoms
17. Injuries and Poisoning
E-codes. External Causes
V-codes. Health Status 35
How are ICD-9 and ICD-10 similar?
III. Tabular list
(600 pages)
1. Infectious Diseases
ICD-10
2. Neoplasms
3. Blood
4. Endocrine
5. Mental
6. Nervous
7. Eye
8. Ear
9. Circulatory
10. Respiratory
11. Digestive
12. Skin
13. Musculoskeletal
14. Genitourinary
15. Pregnancy
16. Perinatal
17. Congenital malformations
18. Signs and Symptoms
19. Injuries and Poisoning
20. External Causes
21. Health Status
36
How are ICD-9 and ICD-10 similar?
Chapter 13: Diseases of the Musculoskeletal System and
Connective Tissue ( M00 – M99 ) page 166
• M00 to M25, Arthropathies (diseases of the joints)
• M40 to M43, Dorsopathies (diseases of the spine)
• M45 to M49, Spondylopathies (diseases of the vertebrae)
• M50 to M54, Other Dorsopathies
• M60 to M63, Disorders of Muscles
• M65 to M67, Disorders of synovium and tendons
• M70 to M79, Other soft tissue disorders
• M80 to M94, Osteopathies and Chondropathies (diseases of bone and cartilage)
• M99 Biomechanical Lesions, NEC (subluxations and others)
Codes assigned to each chapter are broken into blocks of one or more 3 digit codes each. Each block deals with a specific disease and associated symptoms.
37
How are ICD-9 and ICD-10 different?
• The alphanumeric structure of ICD-10 allows for more specific information
• Increased codes and categories allow for more accurate representation of the patient’s diagnoses
38
How are ICD-9 and ICD-10 different?
Feature
Number of Codes
Number of characters
Number of chapters
ICD-9-CM
About 14,000
• 3-5 characters in length
• Characters are all numeric (or E or V)
• Decimal is used after 3 characters
17 chapters
(plus E and V)
ICD-10-CM
About 68,000
• 3-7 characters in length
• Character 1 is alpha
• Character 2 is numeric
• Characters 3-7 are alpha or numeric
• Decimal is used after 3 characters
• Some codes use “x” for characters 4-6
• Character 7 used in certain chapters
21 chapters
39
How are ICD-9 and ICD-10 different?
Feature
Start Date
Expansion
Detail
Laterality
ICD-9-CM
1975, 1979 in US
Very limited
Lacks detail
Lacks laterality
Encounters Encounters are not defined
Combination Codes Combination codes are limited
ICD-10-CM
1994, 2014 in US
Has significant ability to expand without a structural change
Very specific
Includes laterality when appropriate
Initial and subsequent encounters are defined
Combination codes are frequent
40
How are ICD-9 and ICD-10 different?
ICD-9
ICD-10
41
How are ICD-9 and ICD-10 different?
42
How are ICD-9 and ICD-10 different?
Placeholder “x” character (guidelines, page 466)
ICD-10-CM utilizes a placeholder character “x” in positions 4, 5, and/or 6 in certain codes to allow for future expansion.
7th Characters
Certain ICD-10-CM categories have applicable 7th characters. The applicable 7th character is required for all codes within the category, or as the notes in the Tabular
List instruct. The 7th character must always be the 7th character in the data field. If a code that requires a 7th character is not 6 characters, a placeholder “x” must be used to fill in the empty characters.
43
What are some ICD-10 examples?
ICD-10-CM code for chronic gout due to renal impairment, left shoulder, without tophus .
Note: there are 11 gout codes in ICD-9 and 365 in ICD-10
44
What are some ICD-10 examples?
In ICD-9:
E844.8 Sucked into a jet without damage to airplane; ground crew
45
What are some ICD-10 examples?
In ICD-10:
V97.2
:
Sucked into a jet without damage to airplane;
46
What are some ICD-10 examples?
In ICD-10:
V97.2
9
:
Sucked into a jet without damage to airplane; luggage cart driver
47
What are some ICD-10 examples?
In ICD-10:
V97.2
9 &
:
Sucked into a jet without damage to airplane; luggage cart driver; male
48
What are some ICD-10 examples?
In ICD-10:
V97.2
9 & A
:
Sucked into a jet without damage to airplane; luggage cart driver; male; under 5’5” in height;
49
What are some ICD-10 examples?
In ICD-10:
V97.2
9 & A #
:
Sucked into a jet without damage to airplane; luggage cart driver; male; under 5’5” in height; slightly bald;
50
What are some ICD-10 examples?
In ICD-10:
V97.2
9 & A # g
:
Sucked into a jet without damage to airplane; luggage cart driver; male; under 5’5” in height; slightly bald; wearing a tank top
51
What are some ICD-10 examples?
In ICD-10:
V97.2
9 & A # g € : Sucked into a jet without damage to airplane; luggage cart driver; male; under 5’5” in height; slightly bald; wearing a tank top; during a full moon
52
What are some ICD-10 examples?
• V95.42xA Spacecraft crash injuring occupant, initial encounter
• W59.22xA Struck by a turtle, initial encounter
• G44.82 Headache associated with sexual activity
• V91.07xA Burn due to water-skis on fire, initial encounter
(search for this one on FindACode.com)
• W22.01xD Walked into wall, subsequent encounter
• Y34 Unspecified event, undetermined intent
• R45.2 Unhappiness
53
What are some ICD-10 examples?
• M refers to "diseases of the musculoskeletal system and connective tissue."
• After the letter are two characters, then a decimal, then more characters which add more specific information.
• For example, the “ 21 ” in M21.752
(page 196) refers to " other acquired deformities of limbs "
• The “ 7 ” adds the detail of " unequal limb length ."
• The “ 5 ” tells us that it is at the femur
• The “ 2 ” tells us that it is on the left
54
What are some ICD-10 examples?
W61.43 Pecked by a turkey
55
What are some ICD-10 examples?
Migraines
(page 149)
44 choices available for migraines
• Documentation must include: o With or without aura o Intractable or not intractable o With or without status migrainosus o Persistent or chronic o With or without vomiting o With or without opthalmoplegic, menstrual, etc o Induced by ICD-10 training
G43.701 Chronic migraine without aura, not intractable, with status migrainosus
56
What are some ICD-10 examples?
Kissing Spine
In ICD-9
Kissing
(alphabetic index)
Osteophyte
Spine
Vertebra
721.5
721.5
721.5
In ICD-10
(tabular list, page 217)
Kissing Spine, unspecified M48.20
Occipito-atlanto region M48.21
Cervical region M48.22
Cervicothoracic region M48.23
Thoracic region M48.24
Thoracolumbar region M48.25
Lumbar region
Lumbosacral region
M48.26
M48.27
57
What are some ICD-10 examples?
Sixty one year old female presents to your office with ongoing right hip pain and stiffness. Patient stated she had a soft-tissue injury to her right hip six years ago following a bicycle accident.
X-rays at the time negative for fracture.
Tenderness to palpation in the right hip, with a positive Patrick’s test on the right reproducing the hip symptoms. X-rays of the left hip were unremarkable, however, the right hip showed sclerosis of the superior aspect of the acetabulum.
DX: Post-traumatic osteoarthritis of the right hip.
ICD-10:
M99.06 Segmental and somatic dysfunction of lower extremity
M16.51 Unilateral post-traumatic osteoarthritis, right hip
58
Which guidelines do DCs need to know?
General coding guidelines
(page 484) o ICD-10-CM codes should be listed at their highest level of specificity and characters.
a. Use three digit codes only if there are no four digit codes within the coding category. These are the heading of a category of codes.
b. Use the 4, 5, 6, or 7 digit code to the greatest degree of specificity available. These provide further detail.
59
Which guidelines do DCs need to know?
General coding guidelines
o Codes that describe symptoms and signs are only acceptable if that is the highest level of diagnostic certainty documented by the doctor. No other diagnosis has been established (confirmed) by the provider. (see R00 to R99) o Signs and symptoms that are associated routinely with a disease process should not be assigned as additional codes, unless otherwise instructed by the classification.
o Additional signs and symptoms that are not routinely associated with a disease may be reported.
60
Which guidelines do DCs need to know?
General coding guidelines
o Coding for diagnoses that are probable, suspected, likely or questionable are not to be coded, because they indicate uncertainty. They may not be used with outpatient encounters.
o Code all documented conditions that coexist at the time of the visit that REQUIRE OR AFFECT patient care. Do not code conditions that no longer exist.
61
Which guidelines do DCs need to know?
General coding guidelines
o The acute condition should always be listed before the chronic condition if both are present.
62
Which guidelines do DCs need to know?
General coding guidelines
o If the condition is bilateral and there is no bilateral code, then you have to list the left and right code separately.
o List unspecified if laterality is not described
63
Which guidelines do DCs need to know?
General coding guidelines
(page 486) o An unspecified code should be reported only when it is the code that most accurately reflects what is known about the patient’s condition at the time of that particular encounter.
.
o It is inappropriate to select a specific code that is not supported by the health record documentation or conduct medically unnecessary diagnostic testing in order to determine a more specific code.
64
Which guidelines do DCs need to know?
III. Tabular list
ICD-10
1.
Infectious Diseases
2.
Neoplasms
3.
Blood
4.
Endocrine
5.
Mental
6.
Nervous
7.
Eye
8.
Ear
9.
Circulatory
10. Respiratory
11. Digestive
12. Skin
13. Musculoskeletal
14. Genitourinary
15. Pregnancy
16. Perinatal
17. Congenital malformations
18. Signs and Symptoms
19. Injuries and Poisoning
20. External Causes
21. Health Status
65
Which guidelines do DCs need to know?
Chapter 6: Guidelines for diseases of the nervous system
( G00 – G99 )
(page 487)
Dominant or non-dominant side in hemiplegia ( G81 ):
• For ambidexterous patients, default is dominant
• If the left side is affected, default is non-dominant
• If the right side is affected, default is dominant
Pain ( G89 pain, not elsewhere classified )
• For generalized acute, chronic, post-thoracotomy, post-procedural, or neoplasm related.
• Localized pain codes are found in other chapters
(i.e. M54.9, back pain )
• G89 can be the principal diagnosis when it is reason for visit
66
Which guidelines do DCs need to know?
Chapter 13: Guidelines for diseases of the musculoskeletal system and connective tissue
( M00 – M99 )
(page 490)
Site & laterality
• Site represents the bone, muscle, or joint involved
• Bone conditions occurring in a joint are classified by the bone involved, not the joint
• If a “multiple sites” code is available, use it instead of listing several sites individually
Acute traumatic versus chronic recurrent
• In general acute injury should be coded from chapter
19, recurrent or chronic conditions are coded from chapter 13
67
Which guidelines do DCs need to know?
Chapter 18: Guidelines for symptom, signs, and abnormal clinical findings, not elsewhere classified
( R00 – R99 )
(page 491)
Use of symptom codes
• Acceptable when a definitive diagnosis has not been established by the provider
With a definitive diagnosis
• Only when the symptom is not routinely associated with the diagnosis
In a combination code
• Don’t code the symptom separately if it is part of a combination code
68
Which guidelines do DCs need to know?
Chapter 19: Guidelines for injury, poisoning, and certain other consequences of external causes
( S00 – T88 )
(page 492)
The seventh character
• A – initial encounter, while patient is receiving active treatment such as surgery, ER, or evaluation and treatment by a new physician
• D – subsequent encounter, routine care during the healing or recovery phase, such as cast change, medication adjustment, aftercare and follow up
• S – sequela, complications or conditions that arise as a direct result of a condition, such as degenerative disc disease a year after a neck sprain. Sequela code
69
(i.e. DDD) is first, then the injury code.
Which guidelines do DCs need to know?
Chapter 19: Guidelines for injury, poisoning, and certain other consequences of external causes
( S00 – T88 )
(page 492)
Injuries
• Code most serious injury first
• Superficial injuries are not coded with more serious injuries at the same site (such as contusions)
• Primary injury is first, then code for minor injury to nerves and blood vessels
• Pain due to medical devices would sequenced with a
T code followed by G89.18 Other acute postprocedural pain or G89.28 Other chronic postprocedural pain
70
Which guidelines do DCs need to know?
Chapter 20: Guidelines for external causes of morbidity
( V00 – Y99 )
(page 494)
Never sequenced first
Provide data about cause, intent, place, activity, or status of the accident or patient
No national requirement to use these codes, but voluntary reporting is encouraged
Y92 Place of occurrence should be listed after other codes, used only once at initial encounter, in conjunction with Y93
Y93 Activity code should be used only once, at initial encounter
71
How do I find the ICD-10 code?
How do I find the ICD-10 code?
Three methods using the ChiroCode ICD-10 book:
1.
Commonly used code list, pages 44-56 (but don’t stop there!)
2.
GEMs code map, pages 57-133 (don’t stop here either!)
3.
Alphabetic index, pages 455-472 (this is not safe either!)
Always confirm the code using the tabular list
(pages 135-454).
73
How do I find the ICD-10 code?
General Equivalence Mappings (GEMs) o Created by the National Center for
Health Statistics, part of the CDC o Forward maps from ICD-9 to ICD-10 o Backward maps from ICD-10 to ICD-9 o Download the free tablet/smartphone app called “FindACode” o Use the Code Map section in the
ChiroCode ICD-10 book (pages 57-133) o ChiroCode members can access the
MapACode tool in their accounts
74
Quiz
Do questions 1 through 9 in the case studies hand out.
75
How do I find the
ICD-10 code?
One-to-one mapping:
723.1 Cervicalgia
M54.2 Cervicalgia
(Note the Excludes1 note on page 221)
One-to-four mapping:
724.4 Thoracic or lumbosacral neuritis (radicular syndrome of the lower limbs)
M54.14, M54.15,M54.16, M54.17
Radiculopathy
(How do these four codes differ?)
How do I find the
ICD-10 code?
One-to-many mapping:
733.82 Other disorders of bone and cartilage, nonunion of fracture
S02.91XK through S92.919K
(for a total of 2530 corresponding ICD-10-CM possibilities)
How do I find the
ICD-10 code?
Look up 724.3 Sciatica in the “Code Map” section
(this is using GEMs-page 83)
M54.30 Sciatica, unspecified side
-unspecified codes need to be investigated
Look up “sciatica” in the ICD-10 index (page 470)
M54.3 Sciatica
-at least five characters required to code to the highest level of specificity
Now find it in the tabular list (page 221)
78
How do I find the
ICD-10 code?
Combination mapping:
724.3 Sciatica
M54.30 Sciatica, unspecified side
M54.31 Sciatica, right side
OR
M54.32 Sciatica, left side
M54.40 Sciatica with lumbago, unspecified
M54.41 Sciatica with lumbago, right side
M54.42 Sciatica with lumbago, left side
How do I find the
ICD-10 code?
One-to-two mapping:
728.85 Spasm of muscle
M62.40 Contracture of muscle, unspecified site
M62.838 Other muscle spasm
But is that the whole story?
How do I find the
ICD-10 code?
Look up these codes in the tabular list (page 230) and you’ll find:
728.85 Spasm of muscle
M62.40 Contracture Of Muscle Unspecified Site
M62.411 Contracture Of Muscle Right Shoulder
M62.412 Contracture Of Muscle Left Shoulder
M62.419 Contracture Of Muscle Unspecified Shoulder
M62.421 Contracture Of Muscle Right Upper Arm
M62.422 Contracture Of Muscle Left Upper Arm
M62.429 Contracture Of Muscle Unspecified Upper Arm
M62.431 Contracture Of Muscle Right Forearm
M62.432 Contracture Of Muscle Left Forearm
M62.439 Contracture Of Muscle Unspecified Forearm
M62.441 Contracture Of Muscle Right Hand
M62.442 Contracture Of Muscle Left Hand
M62.449 Contracture Of Muscle Unspecified Hand
M62.451 Contracture Of Muscle Right Thigh
M62.452 Contracture Of Muscle Left Thigh
M62.459 Contracture Of Muscle Unspecified Thigh
M62.461 Contracture Of Muscle Right Lower Leg
M62.462 Contracture Of Muscle Left Lower Leg
M62.469 Contracture Of Muscle Unspecified Leg
M62.471 Contracture Of Muscle Right Ankle And Foot
M62.472 Contracture Of Muscle Left Ankle And Foot
M62.479 Contracture Of Muscle Unspecified Ankle And Foot
M62.48 Contracture Of Muscle Other Site
M62.49 Contracture Of Muscle Multiple Sites
M62.830 Muscle Spasm Of Back
M62.831 Muscle Spasm Of Calf
M62.838 Other Muscle Spasm
How do I code for a subluxation?
739.1 Nonallopathic lesions,
Not Elsewhere Classified; cervical region, cervicothoracic region
•
Includes “Somatic and segmental dysfunction”
•
Note: The word “subluxation” does not appear in ICD-
9-CM in the 739 codes.
82
How do I code for a subluxation?
739.1 Nonallopathic lesions,
Not Elsewhere Classified; cervical region, cervicothoracic region
•
Using GEMs / code map (page 96), we find:
•
M99.01 Biomechanical lesions, Not Elsewhere
Classified; segmental and somatic dysfunction of cervical region
•
Note: Still no mention of the “subluxation” 83
How do I code for a subluxation?
739.1 Nonallopathic lesions,
Not Elsewhere Classified; cervical region, cervicothoracic region
•
Using the tabular list (page 252), we find:
•
M99.11 Subluxation complex (vertebral) of cervical region
•
Note: this code maps back to 839 , not 739 84
How do I code for a subluxation?
739.1 Nonallopathic lesions,
Not Elsewhere Classified; cervical region, cervicothoracic region
•
Using the alphabetic index (Subluxation and dislocation cervical vertebrae) we find:
•
S13.1_ _ _ subluxation and dislocation of cervical vertebrae
Still 54 possible combinations!
Note: These codes all map back to 839 codes in ICD-9
85
How do I code for a subluxation?
Fifth character gives the specific vertebral level:
S13.10_ _ Subluxation and dislocation of unspecified cervical vertebrae
S13.11_ _ Subluxation and dislocation of C0/C1 cervical vertebrae
S13.12_ _ Subluxation and dislocation of C1/C2 cervical vertebrae
S13.13_ _ Subluxation and dislocation of C2/C3 cervical vertebrae
S13.14_ _ Subluxation and dislocation of C3/C4 cervical vertebrae
S13.15_ _ Subluxation and dislocation of C4/C5 cervical vertebrae
S13.16_ _ Subluxation and dislocation of C5/C6 cervical vertebrae
S13.17_ _ Subluxation and dislocation of C6/C7 cervical vertebrae
S13.18_ _ Subluxation and dislocation of C7/T1 cervical vertebrae
How do I code for a subluxation?
Sixth character differentiates between a subluxation and a dislocation:
0= subluxation 1= dislocation
S13.110_ Subluxation of C0/C1 cervical vertebrae
S13.111_ Dislocation of C0/C1 cervical vertebrae
How do I code for a subluxation?
Seventh character identifies the encounter:
S13.110A Subluxation of C0/C1 cervical vertebrae, initial encounter
S13.110D Subluxation of C0/C1 cervical vertebrae, subsequent encounter
S13.110S Subluxation of C0/C1 cervical vertebrae, sequela
•
Seventh character extension:
•
A= initial encounter: (i.e. active treatment - initial E/M visit)
•
D= subsequent encounter: (i.e. healing, recovery, aftercare, or follow-up)
•
S= sequela (complications as a result of an injury)
•
(ex: scar due to burns)
How do I code for a subluxation?
739.1 Nonallopathic lesions,
Not Elsewhere Classified; cervical region, cervicothoracic region
•
•
•
All of these options are listed in the “Commonly Used
Codes for Chiropractic” (page 44) for the cervical region.
Be sure to confirm the code selected with the tabular list.
Understand the guidelines and conventions.
89
How do I code for whiplash?
847.0: Sprain of neck
(includes strain of joint capsule, ligament, muscle, tendon)
•
Using the Alphabetic index (sprain of spine cervical) we find:
•
S13.4_ _ _ Sprain of ligaments of the cervical spine
•
Note that there must be seven characters for the code to be complete. (See page 279)
How do I code for whiplash?
847.0 Sprain of neck
•
Using GEMs / code map (page 124) we find:
•
S13.4xxA Sprain of ligaments of the cervical spine
•
S13.8xxA Sprain of joints and ligaments of other parts of the neck
•
This represents six possible codes, depending on the 7 th character, or encounter (A: initial, D: subsequent, or S: sequela)
How do I code for whiplash?
847.0 Sprain of neck
•
S13.4xxA specifies the anterior longitudinal ligament, atlanto-axial joints, atlanto-occipital joints, and whiplash injury
•
S13.8xxA just says “other parts of the neck”
•
Documentation should match these descriptions.
How do I code for whiplash?
847.0 Sprain of neck
•
Which code will be acceptable?
•
Contact the payer to be sure
•
Note the use of the placeholder “x”
•
Note the seventh character
How do I code for whiplash?
847.0 Sprain of neck
(includes strain of joint capsule, ligament, muscle, tendon)
Using the Alphabetic index (injury of muscle, fascia and tendon at neck level) we find:
S16.1xxA Strain of muscle, fascia and tendon at neck level, initial encounter
•
Note: S16.1xxA maps backward to 847.0
How do I code for
DDD?
722.4 Degeneration of a
cervical intervertebral disc
•
Using GEMs / code map, we find:
•
M50.30 Other cervical disc degeneration, unspecified cervical region
•
Unspecified codes should be avoided, if possible
How do I code for
DDD?
722.4 Degeneration of a
cervical intervertebral disc
•
On our own (page 219), we find:
•
M50.31 Other cervical disc degeneration, high cervical region
•
M50.32 Other cervical disc degeneration, mid-cervical region
•
M50.33 Other cervical disc degeneration, cervicothoracic region
Quiz
#9 You diagnose a patient with cervicobrachial syndrome and select the ICD-9 code 723.3
.
• A code map using GEMs (pages 55-131) says that the ICD-10 code could be: M53.1 Cervicobrachial syndrome
• The alphabetic index (pages 441-457) says that the ICD-10 code could be: M53.1 Cervicobrachial syndrome
• The tabular list (page 206) confirms that the code is:
M53.1 Cervicobrachial syndrome
97
Quiz
M53.1 Cervicobrachial syndrome
The fine print in the tabular list says:
-Excludes2:
cervical disc disorder (M50._)
thoracic outlet syndrome (G54.0)
This means that these diagnoses are not included in this code. If they are present, these codes should be listed as well. This information did not appear in ICD-9.
98
Quiz
#10. Patient presents with pain, weakness, numbness, and tingling in both legs. The correct code(s) is/are: a) M54.41, M54.42
b) M54.31, M54.32
c) M54.5
d) M54.9
What method did you use to find the answer?
99
Quiz
#11.
a. In ICD-9, the code used for fibromyalgia is 729.1 Myalgia and myositis, unspecified, fibromyositis NOS . Using the alphabetic index, look up the ICD-10 codes for myalgia, myositis, and fibromyositis.
List them here:
M79.1, M60, M79.7
(note that M60 is incomplete)
b. Using GEMs, identify which codes might replace 729.1 in ICD-10.
M60.9 Myositis, M79.1 Myalgia, and M79.7 Fibromyalgia
(note that M60.9 is unspecified, and fibromyositis has been replaced with fibromyalgia)
c. Describe how you might need to change your documentation for the ICD-10 codes.
100
Quiz
#12. An 81 year old patient presents with spinal stenosis in the lumbar region. What is the appropriate ICD-10 code?
M48.06 Spinal Stenosis, lumbar region
(in index: look up “spinal”, not “stenosis”)
#13. A 32 year old female presents with low back pain at
L4/L5. The pain worsens with extension and with exercise.
The patient complains of tight hamstrings and some numbness and pain in to the right leg. An x-ray reveals a grade II spondylolisthesis at L4. On September 30, 2014, the diagnoses are 724.3 and 738.4
. On October 1, 2014, it is:
M54.31 Sciatica, right side
M43.16 Spondylolisthesis, lumbar region
(GEMs is unspecified, confirm with tabular)
101
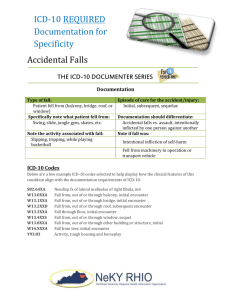
What does the documentation look like?
Codes must be supported by the documentation in the patient record.
The AAPC estimates an increase in documentation time of 15%.
The AAPC also found that
65% of physician notes were not specific enough.
Examples of details not necessary in ICD-9:
• side of dominance
• trimesters
• stages of healing
• laterality
• ordinality
102
What does the documentation look like?
S: Mrs. Finley presents today after having a new cabinet fall on her last week, suffering a concussion, as well as some cervicalgia .
She was cooking dinner at the home she shares with her husband. She did not seek treatment at that time . She states that the people that put in the cabinet in her kitchen missed the stud by about two inches. Her husband, who was home with her at the time told her she was “out cold” for about two minutes . The patient continues to have cephalgias since it happened, primarily occipital, extending up into the bilateral occipital and parietal regions. The headaches come on suddenly, last for long periods of time, and occur every day. They are not relieved by
Advil . She denies any vision changes, any taste changes, any smell changes.
The patient has a marked amount of tenderness across the superior trapezius .
O: Her weight is 188 which is up 5 pounds from last time, blood pressure 144/82, pulse rate 70, respirations are 18. She has full strength in her upper extremities.
DTRs in the biceps and triceps are adequate. Grip strength is adequate. Heart rate is regular and lungs are clear.
A: Status post concussion with acute persistent headaches
Cervicalgia
Cervical somatic dysfunction
P: The plan at this time is to send her for physical therapy, three times a week for four weeks for cervical soft tissue muscle massage, as well as upper dorsal.
We’ll recheck her in one month, sooner if needed.
103
What does the documentation look like?
S06.0x1A
Concussion with loss of consciousness of 30 minutes or less , initial encounter
G44.311
Acute post traumatic headache , intractable
M54.2
Cervicalgia
M99.01
Segmental and somatic dysfunction of cervical region
W20.8xxA
Struck by falling object (accidentally), initial encounter
Y93.G3
Activity, cooking and baking
Y92.010
Place of occurrence, house, single family, kitchen http://www.aapc.com/icd-10/icd-10-documentation-example.aspx
104
Other Activity Codes
• Y93.4 Activity involving dancing and other rhythmic movement (page 440-442) o Y93.41 Dancing o Y93.42 Yoga o Y93.43 Gymnastics o Y93.44 Trampolining o Y93.45 Cheerleading
105
What does the documentation look like?
“Exam findings are consistent with cervical sprain/strain and acute cephalgia due to motor vehicle accident”
In ICD-9, the codes might be:
• 847.0 Cervical sprain
• 339.21 Acute post-traumatic headache
• E813.0 Motor vehicle traffic accident involving collision with other vehicle; driver of motor vehicle other than motorcycle injured
106
What does the documentation look like?
“Exam findings are consistent with cervical sprain/strain and acute cephalgia due to motor vehicle accident”
In ICD-9, the codes might be:
•
847.0 Cervical sprain
• 339.21 Acute post-traumatic headache
• E813.0 Motor vehicle traffic accident involving collision with other vehicle; driver of motor vehicle other than motorcycle injured
107
What does the documentation look like?
“Exam findings are consistent with cervical sprain/strain and acute cephalgia due to motor vehicle accident”
In ICD-9, the codes might be:
• 847.0 Cervical sprain
General Equivalence Mappings (free FindACode app) suggest the following codes:
• S13.4xxA Sprain of ligaments of the cervical spine, initial encounter
OR
• S13.8xxA Sprain of other parts of the neck, initial encounter
Note: When you look up S13.4xxA
in the tabular list, you will find which parts of the cervical spine it includes in the fine print. This is why you need a complete book, not just a short crosswalk list of codes.
108
What does the documentation look like?
“Exam findings are consistent with cervical sprain/strain and acute cephalgia due to motor vehicle accident”
In ICD-9, the codes might be:
• 847.0 Cervical sprain
If you knew to look up
“injury of muscle, facscia and tendon at neck level” in the index you would also find:
• S16.1xxA Strain of muscles, fascia and tendon at neck level, initial encounter
Note: Sprain and strain are separate codes in ICD-10.
Crosswalks won’t tell you about this code, you need to know how to use the alphabetic index.
109
What does the documentation look like?
“Exam findings are consistent with cervical sprain/strain and acute cephalgia due to motor vehicle accident”
In ICD-9, the codes might be:
• 847.0 Cervical sprain
• 339.21 Acute post-traumatic headache
• E813.0 Motor vehicle traffic accident involving collision with other vehicle; driver of motor vehicle other than motorcycle injured
110
What does the documentation look like?
“Exam findings are consistent with cervical sprain/strain and acute cephalgia due to motor vehicle accident”
In ICD-9, the codes might be:
• 339.21 Acute post-traumatic headache
GEMs suggest:
• G44.319 Acute post-traumatic headache, not intractable
Note: In the index G44.319
is next to G44.311
which is the intractable version of this condition.
o Intractable means “hard to control or deal with” o This must be documented in order to select the correct code.
111
What does the documentation look like?
“Exam findings are consistent with cervical sprain/strain and acute cephalgia due to motor vehicle accident”
In ICD-9, the codes might be:
• 847.0 Cervical sprain
• 339.21 Acute post-traumatic headache
• E813.0 Motor vehicle traffic accident involving collision with other vehicle; driver of motor vehicle other than motorcycle injured
112
What does the documentation look like?
“Exam findings are consistent with cervical sprain/strain and acute cephalgia due to motor vehicle accident”
In ICD-9, the codes might be:
• E813.0 Motor vehicle traffic accident involving collision with other vehicle; driver of motor vehicle other than motorcycle injured
Note: External cause codes describe location, circumstances, and causes of injury. More detail is needed since these codes are greatly expanded in ICD-10.
(However, they are only required if you already use ICD-9 E-codes)
113
What does the documentation look like?
“Exam findings are consistent with strain and sprain of the ligaments and muscles of the cervical spine and acute traumatic headache, which does not respond to over the counter medications. Patient was the driver of a vehicle that collided with another motor vehicle on the interstate. He was not treated at the scene.”
The ICD-10 codes in this case are:
• S13.4xxA Sprain of ligaments of the cervical spine, initial encounter
• S16.1xxA Strain of muscles, fascia and tendon at neck level, initial encounter
• G44.311 Acute post-traumatic headache, intractable
• V49.40xA Driver injured in collision with unspecified motor vehicle, traffic accident, initial encounter
• Y92.411 Interstate as place of occurrence of the external cause
114
What does the documentation look like?
“Exam findings are consistent with strain and sprain of the ligaments and muscles of the cervical spine and acute traumatic headache, which does not respond to over the counter medications. Patient was the driver of a vehicle that collided with another motor vehicle on the interstate. He was not treated at the scene.”
The ICD-10 codes in this case are:
• S13.4xxA Sprain of ligaments of the cervical spine, initial encounter
• S16.1xxA Strain of muscles, fascia and tendon at neck level, initial encounter
• G44.311 Acute post-traumatic headache, intractable
• V49.40xA Driver injured in collision with unspecified motor vehicle, traffic accident, initial encounter
• Y92.411 Interstate as place of occurrence of the external cause
115
What does the documentation look like?
“Exam findings are consistent with strain and sprain of the ligaments and muscles of the cervical spine and acute traumatic headache, which does not respond to over the counter medications. Patient was the driver of a vehicle that collided with another motor vehicle on the interstate. He was not treated at the scene.”
The ICD-10 codes in this case are:
• S13.4xxA Sprain of ligaments of the cervical spine, initial encounter
• S16.1xxA Strain of muscles, fascia and tendon at neck level, initial encounter
• G44.311 Acute post-traumatic headache, intractable
• V49.40xA Driver injured in collision with unspecified motor vehicle, traffic accident, initial encounter
• Y92.411 Interstate as place of occurrence of the external cause
116
What does the documentation look like?
“Exam findings are consistent with strain and sprain of the ligaments and muscles of the cervical spine and acute traumatic headache, which does not respond to over the counter medications. Patient was the driver of a vehicle that collided with another motor vehicle on the interstate. He was not treated at the scene.”
The ICD-10 codes in this case are:
• S13.4xxA Sprain of ligaments of the cervical spine, initial encounter
• S16.1xxA Strain of muscles, fascia and tendon at neck level, initial encounter
• G44.311 Acute post-traumatic headache, intractable
• V49.40xA Driver injured in collision with unspecified motor vehicle, traffic accident, initial encounter
• Y92.411 Interstate as place of occurrence of the external cause
117
What does the documentation look like?
“Exam findings are consistent with strain and sprain of the ligaments and muscles of the cervical spine and acute traumatic headache, which does not respond to over the counter medications. Patient was the driver of a vehicle that collided with another motor vehicle on the interstate. He was not treated at the scene.”
The ICD-10 codes in this case are:
• S13.4xxA Sprain of ligaments of the cervical spine, initial encounter
• S16.1xxA Strain of muscles, fascia and tendon at neck level, initial encounter
• G44.311 Acute post-traumatic headache, intractable
• V49.40xA Driver injured in collision with unspecified motor vehicle, traffic accident, initial encounter
• Y92.411 Interstate as place of occurrence of the external cause
118
What does the documentation look like?
“Exam findings are consistent with strain and sprain of the ligaments and muscles of the cervical spine and acute traumatic headache, which does not respond to over the counter medications. Patient was the driver of a vehicle that collided with another motor vehicle on the interstate. He was not treated at the scene.”
The ICD-10 codes in this case are:
• S13.4xxA Sprain of ligaments of the cervical spine, initial encounter
• S16.1xxA Strain of muscles, fascia and tendon at neck level, initial encounter
• G44.311 Acute post-traumatic headache, intractable
• V49.40xA Driver injured in collision with unspecified motor vehicle, traffic accident, initial encounter
• Y92.411 Interstate as place of occurrence of the external cause
119
What does the documentation look like?
“Exam findings are consistent with strain and sprain of the ligaments and muscles of the cervical spine and acute traumatic headache, which does not respond to over the counter medications. Patient was the driver of a vehicle that collided with another motor vehicle on the interstate. He was not treated at the scene.”
The ICD-10 codes in this case are:
• S13.4xxA Sprain of ligaments of the cervical spine, initial encounter
• S16.1xxA Strain of muscles, fascia and tendon at neck level, initial encounter
• G44.311 Acute post-traumatic headache, intractable
• V49.40xA Driver injured in collision with unspecified motor vehicle, traffic accident, initial encounter
• Y92.411 Interstate as place of occurrence of the external cause
120
What does the documentation look like?
“Exam findings are consistent with strain and sprain of the ligaments and muscles of the cervical spine and acute traumatic headache, which does not respond to over the counter medications. Patient was the driver of a vehicle that collided with another motor vehicle on the interstate. He was not treated at the scene.”
The ICD-10 codes in this case are:
• S13.4xxA Sprain of ligaments of the cervical spine, initial encounter
• S16.1xxA Strain of muscles, fascia and tendon at neck level, initial encounter
• G44.311 Acute post-traumatic headache, intractable
• V49.40xA Driver injured in collision with unspecified motor vehicle, traffic accident, initial encounter
• Y92.411 Interstate as place of occurrence of the external cause
121
How do I implement ICD-10 in my practice?
ICD-10 Myths and Facts
• The date will be delayed
Myth
• Worker’s Comp and Auto insurance will still use ICD-9
Fact
• The number of codes make ICD-10 impossible to use
Myth
Documentation requirements are impractical
Myth or Fact
• ICD-10 is already out of date
Myth
• ICD-10 will replace CPT
Myth http://www.cms.gov/Medicare/Coding/ICD10/downloads/ICD-10MythsandFacts.pdf
How do I implement ICD-10 in my practice?
123
How do I implement ICD-10 in my practice?
125
Which parts of a practice will be affected?
Front Desk
• System updates, training
Management
• Vendor and payer contracts
• Budgeting
• Training plan
• Compliance plan, coding guidelines
Providers
• Documentation with more specificity
• New code specific training
Which parts of a practice will be affected?
Clinical areas
• New patient coverage policies
• New super bills
• New LCDs
Billing
• Code set training
• Reimbursement policies (more denials?)
How do I implement ICD-10 in my practice?
According to CMS, 1 in 5 physician practices will see
Medicare denials double within 6 months because they weren't prepared for
ICD-10 by Oct. 1, 2014.
128
How do I implement ICD-10 in my practice?
Readiness Survey:
1. What do you already know about ICD-10?
2. Why are we changing?
3. How much do you think ICD-10 will affect your clinic?
4. What specific questions would you like answered on ICD-10?
5. Where do you plan to go for more information?
How do I implement ICD-10 in my practice?
Budgeting for ICD-10 falls into four categories:
1. Information systems upgrades
2. Education and training
3. Staffing and overtime costs
4. Auditing and monitoring documentation for ICD-10
According to a RAND corporation study, it could cost as much as $40,000 on average, but small clinics may be closer to just $4,000.
How do I implement ICD-10 in my practice?
Questions for your software vendors:
• Do I need to pay for an upgrade?
• Will the software have a built in crosswalk? If so, is it based only on GEMs?
• Will you provide any training or assistance?
• Will the software be able to report both ICD-9 and ICD-10 codes if necessary?
• When will you be ready to test your program?
http://www.cms.gov/Medicare/Coding/ICD10/Downloads
/ICD10TalkingtoVendorforMedicalPractices.pdf
How do I implement ICD-10 in my practice?
Places to update your ICD-9 codes:
• EHR/EMR
• Software – allow time for updates and training.
• Forms – charting forms, internal forms, etc.
• Documents – ex. ABN form
• Website
• Contracts
• Policy & Procedure Manuals
• Inter-departmental documents
How do I implement ICD-10 in my practice?
Update the list of ICD-9 codes you use most often.
Create a new superbill with
your specific ICD-10 mapping!
Start with GEMs code maps, the common code list, and the alphabetic index, but recognize the need to dig deeper.
How do I implement ICD-10 in my practice?
Medicare: free training
ChiroCode.com: free email alerts and webinars, more training, memberships, and chart audits, coding tools
FindACode.com: Crosswalks and other advanced tools
ICD10Monitor.com: free articles
AAPC.com and AHIMA.org
How do I implement ICD-10 in my practice?
How do I implement ICD-10 in my practice?
1. Review the basics- go over these notes again with your whole office
2. Buy ChiroCode Complete and Easy ICD-10 Coding for
Chiropractic (or some other, less spectacular, comprehensive resource)
3. Dedicate a few minutes of each office meeting to ICD-10
1. Assign someone to read ten pages from the book, then report on what they learned (only 43 intro pages).
2. Find articles in Chiropractic trade journals and share them at each meeting.
3. Run a report with the list of most common ICD-9 codes, then create your own crosswalk
4. Take a real patient file and crosswalk it to ICD-10, then rework the documentation.
How do I implement ICD-10 in my practice?
5. Use the project management steps in the book (page 37) to keep on track. You will:
1. Plan a budget for implementation expenses
2. Update all your forms
3. Contact all your vendors
4. Conduct internal testing
6. Use ChiroCode Consulting services if you need help.
7. Have a good time!
Is ICD-10 good….
or bad?
• Researchers will have better data
• Physicians will need to work on documentation
• Billers and coders will need to get familiar with which codes are preferred by payers
• Payers will be able to reimburse more accurately
• Expect increased rejections, denials, and payment delays as both health plans and providers get used to the new codes.
138
Is ICD-10 good….
or bad?
Recommendation: don’t procrastinate.
139
Quiz
#14.
a. Use the commonly used ICD-10-CM codes for Chiropractic section to find idiopathic thoracic scoliosis. (pages 44-56).
M41.24 Other idiopathic scoliosis, thoracic region
b. Now look it up in the alphabetic index (pages 455-472)
M41 Scoliosis
c. Now look up 737.30 in the code map section (pages 57-133)
M41.20 Other idiopathic scoliosis, site unspecified
d. Now go to the tabular list. What do you need to know to choose a code that is not unspecified?
Type of scoliosis (infantile, juvenile, adolescent, thoracogenic, neuromuscular, secondary), then location
140
Quiz
#15. Suzie Derkins reports to the office today after falling at home out of her bed. She appears to suffer from thoracolumbar radiculopathy as a result. She states that she was previously diagnosed with neuralgia. a. The coder selects M54.15 and M79.2. This is wrong.
Why?
Excludes1 b. Use the index to find the appropriate External Cause codes for this scenario. (hint: one describes the place of the accident and the other explains the cause of the injury)
Y92.013 Bedroom of single family house (look up
“place” in the index, then browse Y92)
W06.xxxA Fall from bed (fall from bed)
141
Quiz
16. Find the ICD-10 code for Rheumatoid arthritis:
M06.9 Rheumatoid arthritis, unspecified
17. Find the ICD-10 Code for pain in the neck:
M54.2 Cervicalgia
(look up “cervicalgia” not “neck” or “pain”)
142
Quiz
21. Mr. Smith presents with a sprained ankle. What questions need to be asked in order to find the complete ICD-10 code?
Which ligament, which side, which encounter?
S93.4_ _ _ Sprain of ankle
22. Create the proper documentation for S43.211D
Anterior subluxation of right sterno-clavicular joint, subsequent encounter
23. a. Create the proper documentation for M41.124.
Adolescent idiopathic scoliosis, thoracic region b. Is this code appropriate for congenital scoliosis?
No, excludes1, should be Q67.5 Congenital deformity of the spine
143
Quiz
24. After an MRI, Mr. Hobbes is diagnosed with L4/5 disc herniation with right-sided sciatica. How many codes are necessary? One or two?
M51.16 Intervertebral disc disorders with radiculopathy, lumbar region - includes the disc and the sciatica. See excludes1 at M54.3_ Sciatica
25. Calvin complains of numbness in his right hand as well as neck pain. An x-ray reveals spondylosis all throughout the cervical spine.
M47.22 Other spondylosis with radiculopathy,
cervical region M54.2 Cervicalgia may be included
144
Procrastination
145
Thank You
Visit Our Booths
For More Information Contact www.paydc.com
www.chirocode.com
146