Organ Preservation with Histidine-Tryptophan
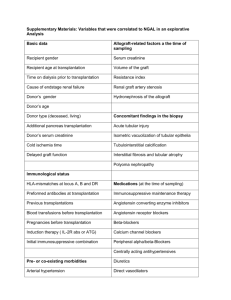
advertisement

Organ Preservation with HistidineTryptophan-Ketoglutarate (HTK) Solution: Clinical Results Charles M. Miller MD Director, Liver Transplantation Program Professor of Surgery Cleveland Clinic Organ Preservation Solutions Preservation solutions are used to maintain the hypothermic organ in optimal condition from the time of explantation until implantation Principles of Organ Preservation • Exsanguination to reduce intravascular thrombosis • Hypothermia to reduce cellular metabolism • Maintain cell membrane integrity to avoid cellular swelling • Susceptibility to cold ischemic injury: vascular endothelium > parenchymal cells Ischemia • Decreased mitochondrial function – Anaerobic conditions depletion of ATP – Alterations in ion permeability – Accumulation of lactate • Accumulation of hypoxanthine • Cell swelling • Cytosolic calcium accumulation Reperfusion • Generation of reactive oxygen species • Increased oxidative stress • Lipid peroxidation of cellular membranes • Free radical formation leads to cellular destruction • Results in macrophage/Kupffer cell activation – Increased serum tumor necrosis factor (TNF) • Damage can lead to prolonged hypoxia after reperfusion History of Organ Preservation • • • • • • • Simple cooling with cold solution Continuous hypothermic perfusion Collins (1967) Euro-Collins (1980) University of Wisconsin - ViaSpan (1986) HTK - Custodiol (1980’s) Celsior - 1994 Euro-Collins Solution • High potassium, glucose, and phosphate-based solution • Designed to mimic composition of intracellular fluid • Low cost • Poor preservation quality • Short preservation times achievable UW Solution • Use of impermeant molecules, lactobionate and raffinose, in preventing cell swelling • First developed for and applied in preservation of canine pancreas • Hydroxyethyl starch to minimize interstitial edema during machine perfusion, not necessary during cold storage • High [K+], low [Na+] Southard and Belzer UW Solution: Disadvantages • Glutathione is oxidized during storage: addition of fresh GSH immediately before use; other additives • High viscosity • Solution cannot be released into circulation (high K content) • Huge particles ~ 100 µm in diameter contained in original solution: must use in-line filtration with 40 µm pore size.Particles caught in capillary bed of perfused organ, resulting in vascular constriction, impeded reperfusion, and reduction of functional recovery Crystals in UW solution stored at sub-zero temperature (a ) perfused livers (b) pancreas (c) kidneys (d) Tullius et al: AJT 2:627 HTK Solution (Custodiol) • Developed as cardioplegia • Low potassium • High buffering capacity of histidine • No colloid - viscosity equal to that of pure water from 1 to 350C, with mean flow rate 3X that of UW solution at equal perfusion pressure organs exsanguinate and cool down to lower temperatures more rapidly than with UW M.M. Gebhard, H.J. Kirlum, C. Schlegel. Organ preservation with the solution HTK Component UW HTK Sodium (mmol/L) 40 15 Pottasium (mmol/L) 120 10 Lactobionate (mmol/L) 100 - Phosphate (mmol/L) 25 - Raffinose (mmol/L) 30 - Adenosine (mmol/L) 5 - Ketoglutarate (mmol/L) - 1 Histidine (mmol/L) - 198 50 - Mannitol (mmol/L) - 30 Tryptophan (mmol/L) - 2 Osmolality (mOsm/L) 320 310 Starch (gm/L) Randomized Controlled Trials • Kidney 1 European, 3-year follow-up 1998, n = 650 transplants, Deceased donors • Pancreas 1 European 2009, n=68 transplants • Liver 3 European 1994 (n=60) – Deceased donors 2003 (n=30) – Living donors 2005 (n=40) – Deceased donors Kidney Preservation Transplants: HTK 332, UW 312 DGF: Need for dialysis 2 or more times during first 7-days post-transplant Flush volume: HTK 5 – 6 L UW 1 – 2 L EC 4L 16 Kidney preservation de Boer, et al, Transpl Proc, 1999; 31: 2065 17 Kidney preservation de Boer, et al, Transpl Proc, 1999; 31: 2065 18 Kidney preservation Lynch RJ, et al. AJT 2008; 8:567-73 19 Kidney preservation Post-transplant kidney graft survival Living Donor: HTK n=475 UW n=475 Deceased donor: HTK n=317 UW n=317 Lynch RJ, et al. AJT 2008; 8:567-73 20 Pancreas preservation Transplants: randomized 68 transplants over 18 months at 4 centers Outcomes: 6-month graft survival – NO DIFFERENCE Graft function – NO DIFFERENCE Fasting BG C-peptide level HbA1c Insulin requirement Flush volume: HTK UW 5–8L 3L n=41 n=67 21 Pancreas preservation Figure 1. No insulin requirement Figure 2. Serum amylase level Figure 3. Serum lipase level 22 Pancreas preservation Figure 4. C-peptide level Figure 5. Units exogenous insulin Figure 6. HbA1c 23 Pancreas preservation Indiana University, 2003 to 2007-- Largest center in USA N = 310 HTK 262, UW 48 Simultaneous, retrospective 1-year graft survival – 91% (U.S. 79-86%) 24 Liver Transplantation • Hatano et al: Hepatic preservation with histidinetryptophan-ketoglutarate solution in living-related and cadaveric liver transplantation. Clinical Science (1997), 93:81 • Evaluated graft oxygenation state after reperfusion in LRLT using near-infrared (NIR) tissue spectroscopy • LRD liver: HTK (15) vs UW (49) • CAD liver: HTK (30) vs UW (18) E. Hatano, et al. Tissue oxygenation in living related liver transplantation (Clinical Science, 1997) LRLT Intraoperative changes in mean value of oxygen saturation of Hb at 10 points in liver graft After reflow of operation Biliary Complications Develop up to 30% of Patients After Liver Transplantation Post-liver Transplant Biliary Strictures • Biliary strictures after liver transplantation: 10-30% • Adequate flushing of peri-biliary arterial tree is important • High viscosity preservation solutions might not completely flush the small donor peribiliary plexus Peri-Biliary Vascular Plexus Alpini et al. et al. 7:540-545, 2001 Pirenne et al. LiverPirenne Transplantation, Liver Transplantation, 7:540-545, 2001 Two group of liver recipients: Group 1 (24): Donor aortic flush with Marshall solution Portal vein with UW Group 2 (27): Donor aortic flush with UW Portal vein with UW CIT: 692+190 ( group 1) vs. 535+129, (group 2), (P=.001) Preservation cost 1.9 times greater in the UW than in the Marshall group Pirenne et al. Liver Transplantation, 7:540-545, 2001 • Recipient surgeon : Same surgeon • All biliary reconstruction duct-to-duct except in one patient • One-year patient and graft survival 92% (1) and 100% (2) • Biliary stricture: 1/24 (4.1%) group 1 8/27 (29.2%) group 2 Biliary stricture in group 1: 4 months after LTX and anastomotic Biliary strictures in group 2: 1-12 months after LTX and anastomotic, extrahepatic, intrahepatic or a combination of intra-and extrahepatic HTK and UW for Liver Preservation Hannover (1988 - 2000) n = 1068 HTK UW • n 461 607 • PF 439 578 • INF 22 29 • INF % 4.8 % 4.8 % p = 1.00 HTK and UW for Liver Preservation Hannover (1988 - 2000) n = 1068 CIT >15 hours HTK UW • n 36 154 • PF 34 143 • INF 2 11 • INF % 5.6 7.1 p = 1.000 Liver Transplant Patient Survival Hannover (1988 - 2000) 100 % 80 HTK (n = 400) 60 UW (n =4 92) 40 20 P < 0.0331 (LogRank) 0 0 1 2 3 4 years 5 Liver Transplants Graft Survival Hannover (1988 - 2000) 100 % 80 HTK (n = 461) 60 40 UW (n = 607) 20 P < 0.0029 (LogRank) 0 0 1 2 3 4 years 5 HTK and UW for Liver Preservation Hannover (1988 - 1998) n = 836 Biliary Tract Complications HTK UW • n 305 531 • BTC 39 65 • BTC % 12.8 12.2 HTK vs. UW University of Gottingen Patients and Methods Patients 123 120 Adults, 3 Children; Age 1 - 70 years Transplantations: Total 134 Cadaveric: 123 primary, 10 secondary, 1 tertiary 114 standard orthotopic, 5 split, 4 partial Living donation: 11 (right lobe) Combined: 6 kidney transplantation 1 bone marrow transplantation 1 heart and kidney transplantation Preservation solution: 63 HTK und 71 UW HTK vs. UW: University of Gottingen Initial Liver Function OLT total HTK UW 63 71 Initial function (IF) 45 (71.5%) 43 (60.5%) Initial dysfunction (IDF) 13 (20.6%) 26 (36.6%) Initial nonfunction (INF) 5 (7.9%) 2 (2.8%) HTK vs. UW University of Gottingen Biliary Complications HTK Bile duct necrosis Localized strictures UW 3 (16, 17, 485 d) 3 (44, 10, 8, 46 d) 2 (72, 150 d) Diffuse strictures (ITBL) - Total 5 ITBL = ischemic type biliary lesion 2 (210, 305 d) 3 (610, 210, 365 d) 8 HTK vs. UW University of Gottingen Biochemical Parameters HTK AST UW (U/l) 1320 + 1254 1389 + 1214 “ pod 7 (U/l) 26.7 + 17.5 24.3 + 18.4 AP pod 7 (U/l) 159.7 + 94.6 214.8 + 109.2 81 + 52.9 84.6 + 59.5 Bilirubin pod 14 (mg/dL) 9.5 + 9.7 13.8 + 12.6 max GGT pod 7 (U/l) HTK vs. UW University of Gottingen Comparative Analysis - Similar ischemic damage (AST) in both groups. - Similar length of ICU stay in both groups. - The rate of IDF/INF was similar in both groups. - Bilirubin was higher in UW group (13.8 vs. 9.5 mg/dL pod 14). - Biliary complications significantly higher in UW group (8/71 vs. 5/63). No ITBL in the HTK group. HTK solution for organ preservation in human liver transplantation A prospective multi-center observation study Pokorny et. al. Transplant International 2004; 17:256-260 (Austria, Germany) • • • • • • 214 patients in 4 European centers (1996-1999) 5 liters of HTK for preservation CIT 444 + 224 All vascular anastomoses completed before reperfusion No pre-reperfusion flush PNF 2.3%, Initial dysfunction 6.5% Graft dysfunction not correlated with CIT • 1-year patient and graft survival 83% and 80% (unrelated to CIT) • HTK: safe and effective and easy to use. • Comparable to UW with less cost. HTK vs. UW in LDLT Chan et. al. Liver Transplantation 2004; 10:1415-1421 (Hong Kong) Number of patients Age CIT Biliary stricture* Pre-reperfusion flush Graft loss Hospital mortality UW 30 38.5 112 (79 + 334) 10 (33%) Yes 0 0 Biochemistry: No significant differences Cost analysis: UW $137.6 higher than HTK/patient * Not significant HTK 30 35.5 111.5 (75 + 222) 6 (20%) No 1 0 Liver Preservation Liver Preservation Indiana University, 2001 to 2008 All adult, deceased donor n=1013 HTK 632, UW 381 Simultaneous, retrospective Liver Preservation Indiana University, 2001 to 2008 Post-liver transplant serum ALT, n=1013 600 All adult, deceased donor Simultaneous, retrospective 500 HTK 632 UW 381 HTK 300 UW Serum ALT 200 100 0 0 5 10 15 20 25 30 35 Days post-transplant Post-liver transplant serum total bilirubin, n=1013 4 3.5 Serum total bilirubin n=1013 Serum ALT 400 3 2.5 HTK 2 UW 1.5 1 0.5 0 0 5 10 15 20 Days post-transplant 25 30 35 Serum Bilirubin Liver Preservation 3 Randomized Studies: 1. Erhard J, et al. Comparison of HTK versus UW for organ preservation in human liver transplantation: A prospective, randomized study. Transplant International 1994; 7: 177-81. • 60 deceased donor liver transplants (HTK n=30 and UW n=30) • No difference in early and late graft survival, even for 7 donor livers with cold ischemia time >15 hrs • More late biliary complications in UW group. • Higher initial transaminases in HTK group. 2. Testa G, et al. HTK versus UW in living donor liver transplantation: results of a prospective study. Liver Transplantation 2003; 9(8): 822-26. • 30 consecutive living donor right lobe transplants flushed alternately with HTK (n=16) or UW (n=14) • Patients were randomly allocated based upon timing of transplantation • 1-year post-transplant, there is no difference in graft and patient survival, liver enzymes and complications 3. Nardo B, et al. Preliminary results of a clinical randomized study comparing Celsior and HTK solutions in liver preservation for transplantation. Transpl Proc 2005; 37:320-2. • European randomized trial comparing Celsior and HTK. • No difference in initial function or survival up to 1-year post-transplant. HTK vs. UW in liver transplantation A meta analysis Feng et.al. Liver Transplant, 2007 HTK vs. UW in liver transplantation A meta analysis P= 0.87 RR 1.01 Patient Survival P= 0.86 RR 1.01 Graft Survival Feng et.al. Liver Transplant, 2007 HTK vs. UW in liver transplantation A meta analysis Feng et.al. Liver Transplant, 2007 HTK vs. UW in liver transplantation A meta analysis • Cost: HTK cheaper than UW • Biliary complications: Trend for less biliary strictures with HTK • PNF, PDF, DGF: No difference • Graft survival: No difference • Patient survival: No difference • Biochemical values: No difference Feng et.al. Liver Transplant, 2007 Recent retrospective database reviews Conclusion of all 3: These results suggest that the increasing use of HTK for abdominal organ preservation should be reexamined. Recent retrospective database reviews • Data review: – Usually large database is better to increase numbers – In large transplant research, single center better to maintain homogeneous patient, donor and management factors • Database review Selection bias • Do surgeons who use HTK differ from those that use UW ? • CONFOUNDING – database differences likely just highlight differences in practice patterns between surgeons who use HTK and those who use UW – Kidney study – exclude all machine pumped kidneys – Pancreas study – unable to differentiate high risk grafts – Liver study – no ability to analyze steatosis, hypernatremia, etc 53 Histidine-Tryptophan-Ketoglutarate Solution Vs. University of Wisconsin Solution for Deceased Donor Liver Transplantation: Analysis of SRTR Database Cleveland Clinic Purpose • This analysis aims to evaluate the impact of the organ preservation solutions (OPS) ,(Histidine-TryptophanKetoglutarate (HTK) vs. University of Wisconsin (UW) solution) on the outcome of adult deceased donor liver transplantation (DDLT) using the Scientific Registry of Transplant Recipient (SRTR) database. Materials and Methods Only adult first liver-only transplants from 2002-2006 for whom both flush and storage solutions were the same. Risk-unadjusted graft survival was estimated non-parametrically by the method of Kaplan and Meier, and parametrically by a multiphase hazard decomposition method Statistical Analysis • Risk factors for graft survival were determined using nonproportional, multiphase, multivariable hazard methodology. This methodology allows modeling of recipient, donor, and procedure variables in all phases of the hazard model simultaneously. Bootstrap aggregating was used for variable selection with a probability for inclusion of 0.001; variables appearing in at least 50% of bootstrap analyses were considered reliably statistically significant at p<0.001. Patients • The data set included 20,908 patients, 17,559 (84%) with UW and 3349 (16%) with HTK solutions. Mean follow-up was 2.9 ± 1.5 years (3.0 ± 1.5 years for UW and 1.9 ± 1.0 years for HTK). We defined an early phase (EP) shortly after DDLT followed by a constant phase (CP) of hazard for graft failure. Results • Significant predictors of graft failure in the EP after DDLT include the following recipient factors: older age, race either White or Black, portal vein thrombosis, last creatinine and last MELD for the transplant (tx) candidacy, on life support just prior to tx, and previous kidney tx. Risk Factors for Graft Failure Early Phase Risk Factor P Bootstrap % Early hazard phase Older recipient age (years) <.0001 93 .0005 69 Recipient portal vein thrombosis <.0001 95 Recipient previous abdominal surgery <.0001 48 Candidate last creatinine (used for MELD) <.0001 86 Candidate last MELD <.0001 71 Recipient on life support just prior to tx <.0001 100 Recipient previous kidney transplant <.0001 90 Donor race non-White <.0001 67 Donor donation after cardiac death <.0001 100 Donor risk index <.0001 46 Recipient race White or Black Risk Factors for Graft Failure Constant Phase Risk Factor P Bootstrap % Constant hazard phase African American recipient <.0001 97 Recipient tumor (incidental) at transplant <.0001 88 Recipient primary diagnosis for tumors <.0001 87 Recipient hepatitis C virus <.0001 100 Donor age (years) <.0001 97 Donor history of diabetes <.0001 77 Results • Significant donor factors in the EP are: race other than White, donation after cardiac death (DCD) and donor risk index (DRI). OPS did not appear as a statistically significant predictor of graft failure. Hospital death, retransplant rates (overall and within 14 days of initial transplant) and relisting rates (overall and within 30 days of tx) were similar (p>0.05). Patient Survival - Donor >65 • • • • Donor Age > 65 N=1698 UW N= 311 HTK p=.46 log rank test Patient Survival - Donor <65 • • • • Donor Age <65 N=15861 UW N= 3038 HTK p=.28 log rank test Patient Survival - DCD Donor • • • • DCD Donor N=570 UW N=159 HTK p=.73 log rank test Patient Survival - Non-DCD Donor • Non-DCD Donor • N=16989 UW • N=3190 HTK • p=.55 log rank test Patient Survival - DRI >2.5 • • • • Donor DRI >2.5 N=8663 UW N=1682 HTK p=.25 log rank test Patient Survival - DRI <2.5 • • • • Donor DRI <2.5 N=6600 UW N=1218 HTK p=.37 log rank test Graft Survival - Donor Age >65 • • • • Donor Age >65 N=1698 UW N= 311 HTK p=.64 log rank test Graft Survival - Donor Age <65 • • • • Donor Age <65 N=15861 UW N= 3038 HTK p=.045 log rank test Graft Survival - DCD Donor • • • • DCD Donor N=570 UW N=159 HTK p=.17 log rank test Survival Rate (%) . Kaplan-Meier Adult Graft Survival Primary Deceased Donor Liver Transplants 2000-2006 100 90 80 70 60 50 40 30 20 10 0 0 2 4 6 8 10 12 14 16 18 20 22 24 26 28 30 32 34 36 Months Post Transplant DBD SRTR DCD-UW DCD-HTK Includes adult, primary, liver alone transplants Graft Survival - Non-DCD Donor • Non-DCD Donor • N=16989 UW • N=3190 HTK • p=.23 log rank test Graft Survival - DRI >2.5 • • • • Donor DRI >2.5 N=8663 UW N=1682 HTK p=.053 log rank test Graft Survival - DRI <2.5 • • • • Donor DRI <2.5 N=6600 UW N=1218 HTK p=.15 log rank test Used casewise deletion of missing data, i.e. threw out cases that were missing any of the predictor variables they were studying. It means they are using only patients for whom all variables were reported - doing this can potentially bias results SRTR Information Flow Monthly Transfer OPTN Person Linking SRTR CMSESRD SSDMF SEER Data Quality Analysis File Creation Data Fixes Feedback OPTN MPSC OPOSpecific Reports Data Use Agreements Standard Analysis Files Center-Specific Analyses CenterSpecific Reports NCHS, AHA, etc Reorganization for Research Cleaning and Validation Analysis Variables Added Public Release External Research Analytical Procedures and Products TAC RFI Journal Articles Conference Present’ns OPTN, ACOT Committees Annual, Biennial Reports Implications of Casewise Deletions • While they do say that data were missing for less than 4% of covariates, if the missing values were scattered over 20% of patients, then 20% of total data might have been deleted. • Example: – SRTR CIT data: 100% complete – UNOS CIT data: 86% complete Critique • Last transplant included was 2/28/08 - the paper was submitted on 7/17/08. Assuming that it took 45 days to analyze and write the paper, then the data cutoff would have been 6/1/08. Given that the first recipient follow-up form required by UNOS is at 6 months and then they only release data after a 60 day period for completion, they only have data for transplants performed before 11/1/07 Other Considerations • Slightly different timeframes: – is there a change in clinical practice? – is there a learning curve for new users of HTK? • Do the conclusions make sense? – Recipient age 18-34 HR 1.14 – COD - CVA, HR 1.04 (SRTR HR 1.16) – COD - DCD, HR 1.97 (SRTR HR 1.51) Does Not Fit Clinical Impressions • Cleveland Clinic DCD experience – 15 controlled DCD LTX preserved with HTK since 2005 – Heparin could not be given prior to declaration of death – Mean donor age was 38 ± 12 years – Mean WIT and CIT was 25 ± 9 min and 427 ± 97 min, respectively – No recipient developed ITBS. PNF was seen in one recipient who was salvaged with retransplantation Summary and Conclusions • All randomized controlled trials large single center case series, across multiple organs, countries and time periods demonstrate no difference in clinical outcomes between HTK and UW • Question of appropriate flush volume - of particular importance to the pancreas • There is a clear cost benefit in the use of HTK • Recent database reviews of tens of thousands of patients likely reflect difference in practice patterns between surgeons who use HTK and those who use UW. It is less likely to represent a true difference in the clinical outcomes of the two solutions when the vast majority of high quality studies show no difference. 84 Thank You