Document
advertisement

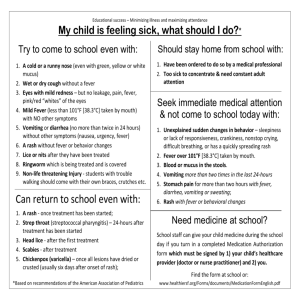
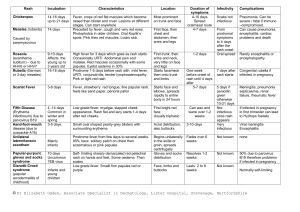
Differential Diagnosis Digital Lecture Series : Chapter 29 Dr. Saumya Panda Professor, Department of Dermatology, KPC Medical College, Kolkata CONTENTS Formulating the d/d Malar rash Occam’s razor Thickened nerves Fever with rash Bubo Arthritis, fever and rash Genital ulcer disease Dysesthesia without obvious Annular lesions primary lesion Painful nodules Hypopigmented patch MCQs Photo Quiz Differential diagnosis - Factors to consider Symptoms (e.g. fever, pain, pruritus) Duration and natural history ( acute, subacute, chronic, intermittent) Basic morphology (‘primary lesions’) (macules, patches, papules, plaques, nodules, vesicles, bullae, pustules) Secondary morphology (scales, crusts, erosions, ulcers, scars) Arrangement (annular, linear, solitary, generalized) Topographical location (arms, feet, head) Colour (black, blue, brown, red, yellow) Laboratory findings Histopathology findings Occam’s Razor Principle of problem-solving. Among competing hypotheses, the one with the fewest assumptions should be selected. Other, more complicated solutions may ultimately prove correct, but-in the absence of certainty - the fewer assumptions that are made, the better for accurate diagnosis. Fever with Rash Fever & Rash Viral infection Measles Rubella Varicella Erythema infectiosum Roseola Enterovirus infection Infectious mononucleosis Dengue Viral hepatitis Other infections Meningococcemia Staphylococcemia Scarlet fever Typhoid fever Pseudomonas bacteremia Syphilis Rocky mountain spotted fever Lyme disease Bacterial endocarditis Drug hypersensitivity Penicillins Sulphonamides Quinolones ATTs Anticonvulsants Thiazides Miscellaneous Serum sickness Erythema marginatum Erythema nodosum SLE Dermatomyositis Allergic vasculitis Pityriasis rosea Viral Infections Infections : Viral exanthems Disease/ Incubation Virus Measles (1-2 wks) 1st disease Paramyxovirus rubeola Prodrome, Koplik’s spots , rash 4/ 5th day of fever, cephalo-caudal, fades 5- 10 days, complications: diarrhoea, pneumonia, SSPE. Rubella (2-3 wks) 3rd disease Togavirus rubella 50% subclinical, Mild prodrome , Forschheimer’s spots, rash begins on face and spreads downwards; lymphadenopathy. Clinical Features Measles Koplik’s spots : A prodromic viral enanthem of measles manifesting 1-2 days before the rash. Characterized as clustered, white lesions on the buccal mucosa (opposite the lower 1st & 2nd molars). Fever characteristics : Typically the fever continues increasing in intensity till 4-5 days after onset. Exanthem : Typically appears on the 3rd day of fever and subsides with desquamation. Measles Exanthem Infections : Viral exanthems Disease/ Incubation Erythema infectiosum (2-3 wks) 5th disease Exanthem subitum (5-15 days) 6th disease Virus Clinical Features Parvovirus B19 Mild / absent prodrome, 3 distinct, stages slapped cheek, generalised exanthem, reticulate erythema , recurrent phase , no lymphadenopathy, Complications: polyarthropathy , gloves and stocking syndrome. HHV6, HHV7 Rash begins suddenly when fever subsides on 6th day, Pink almond shaped macules- neck and trunk, no complications. Erythema Infectiosum Exanthem Subitum Roseola Infantum. Evolution of Signs and Symptoms. Pale pink macules may appear first on the neck. Numerous pale pink, almond-shaped macules. Infections : Viral Disease/ Incubation Virus Clinical Features Non-specific exanthem (variable) Entero, echo, coxsackie virus Morbilliform rash with fever, asymptomatic. Occ urticarial, petechial vesicular, palms/soles involved, confused with drug rash. HFMD (4-6 days) Coxsackie virus A16, enterovirus 71 Mild prodrome, aphthae, small macules with vesicular center and red areola, oval, extremities and buttocks, complications : CNS, pulmonary edema. Hand Foot & Mouth Disease HFM Infections : Viral Disease/ Incubation Varicella (14-16 days) Virus Clinical Features Low grade fever, malaise, classical dew drops Varicella-zoster on a rose petal, pleomorphic, centripetal, complications : pneumonia, CNS, Reyes. Herpes Simplex HSV I & II (2 -14 days) Primary and recurrent episodes, fever, malaise, lymphadenopathy, gingivostomatitis, kaposi’s varicelliform eruption. Varicella Primary Herpes Tzanck smear shows multinucleated giant cells. Primary cases may be severe, recurrent or secondary cases are relatively asymptomatic, with patients being mostly afebrile. Infections : Viral Disease/Incubation Infectious mononucleosis Dengue Chikungunya Virus Epstein Barr Virus FlavivirusDengue fever virus Chikungunya virus Clinical Features Fever, pharyngitis, lymphadenopathy- triad palatal enanthem, morbilliform rash, scarlatiniform, urticarial or petechial, periorbital edema, uncommonly-EM, EN Severe eruption may be associated with antibiotic Rx ampicillin , amoxicillin. Fever, muscle and joint pain, thrombocytopenia causing petechiae, ecchymoses, mucosal bleeding, exanthematous rash, generalized erythema with areas of normal skin. Fever, arthralgia, exanthem, rash appears 1-10 days, fades in 1 week, unusual features- vesiculobullous, purpuric macules, pigmentation, aphthae. Dengue Skin Rash and Subconjunctival Haemorrhage Note the well-defined islands of uninvolved skin in a sea of erythema Other Infections Other infections Staphylococcal Scalded Skin Syndrome (SSSS) : Staphylococcal aureus Scarlet fever : streptococcus pyrogenic exotoxin A. Toxic Shock syndrome : Staphylococcal aureus or streptococcus pyogenes. Meningococcemia : N. meningitidis Pseudomonas, Pneumococcal, H. influenza infections. Enteric fever Leptospirosis Syphilis Rickettsial infections Clinical picture of sepsis, DIC- Disseminated purpuric papules plaques, infarcts, peripheral gangrene, purpura fulminans, necrotic areas with eschar formation. Staphylococcal scalded skin syndrome Also known as Ritter’s disease. Phage group II staphylococcus, type 55 and 71, epidermolytic toxin. Diffuse erythema, scaling, blisters, Nikolsky+. No mucosal involvement. Scarlet fever Pharyngitis, Forschheimer’s spots, strawberry tongue Lymphadenopathy, Scarlatiniform rash generalized within 2 days, Pastia’s lines, fades in 1 week Schultz-Charlton test: Intradermal injection of human scarlet fever immune serum; a positive reaction consists of blanching of the rash in the area surrounding the point of injection. Scarlet fever Toxic shock syndrome Toxin-mediated acute life-threatening illness, precipitated by infection with either Staphylococcus aureus or group A Streptococcus (GAS), also called Streptococcus pyogenes. Characterized by high fever, rash, hypotension, multi-organ failure (involving at least 3 or more organ systems), and desquamation, typically of the palms and soles, 1-2 weeks after the onset of acute illness. The clinical syndrome can also include severe myalgia, vomiting, diarrhea, headache, and nonfocal neurologic abnormalities. Toxic shock syndrome : Evolution of signs and symptoms Meningococcal Disease and Purpura Fulminans Rapid onset and fulminant course Prodrome Headache, neck stiffness, nausea, vomitting, high grade fever and rash within 2-5 hours Pseudomonas aeruginosa Infections Pseudomonas Folliculitis Pseudomonas infections can present as folliculitis, ecthyma gangrenosum, or with features of sepsis Progression of soft tissue swelling to vesicle or bulla formation is an ominous sign. Enteric fever and Leptospirosis Rose spots in typhoid Characteristic rash in leptospirosis Congenital Syphilis Rickettsial infections in India Scrub Typhus Spotted Fever Indian Tick Typhus Rickettsial Pox Classical Triad of Rickettsial Pox Fever Eschar Rash : numerous monomorphous papules with a small central vesicular component Difference of Chickenpox from Rickettsial Infections More number of lesions No eschar Polymorphic Common Systemic Features Fever Myalgia,arthralgia G I Symptoms Lymphadenopathy Rickettsial Pox In ricketssial pox, the site of tick bite can be seen, may show escharification; the rash can mimic chickenpox. Chicken pox has to be differentiated from rickettsial pox by the presence of polymporphous rashes at different stages of evolution and the presence of eschar in the latter. Drugs Drug Eruptions (with fever and rash) Type Clinical Features Drugs Exanthemata Generalized, morbilliform Anticonvulsants, ampicillin, cephaosporins, dapsone, sulfonamides, NSAIDS, NNRTI Urticarial Wheals, variable, angioedema Penicillins, NSAIDs, sulfonamides, vaccines, radiocontrast media EM major Target lesions, Mucosal involvement Anticonvulsants, AKT, sulfonamides, NSAIDs, dapsone, NNRTI Drug Eruptions (with fever and rash) Type Clinical Features Drugs SJS/TEN Atypical target, bullae, epidermal necrosis, Mucosal involvement, Nikolsky+ Anticonvulsants, AKT, sulfonamides, NSAIDs, dapsone, NNRTI DHS Facial edema, gen erythema, lymphadenopathy, internal organ involvement Aromatic anticonvulsants, Sulfonamides Erythroderma Generalized erythema Penicillins, sulfonamides, dapsone, with scaling anticonvulsants Drug vs Bug : Exanthem Clinical Feature Drug Bug Incidence Uncommon Common Fever ++ ++++ Constitutional symptoms ++ ++++ Lymphadenopathy ++ +++ Pruritus Present Usually absent Mucosal involvement + ++ Drug vs Bug : Exanthem Clinical Feature Drug Bug Evolution of rash Variable evolution, Characteristic evolution, subsides slowly after drug prodrome, rash and fever, withdrawal, 1-2 weeks subsides faster 3-5 days Skin biopsy Interface dermatitis Perivascular mononuclear Laboratory values Eosinophilia, abnormal liver enzymes Lymphocytosis Severe Urticaria and erythema multiforme Early Lesions of TEN Extensive Skin Involvement in TEN Arthritis, Fever and Rash Viral infections Acute rheumatic fever • Rubella Kawasaki disease • Parvovirus B-19 Urticarial vasculitis • Gonococcemia Acute sarcoidosis Other infections Still’s disease • Meningococcemia • Lyme borreliosis • Familial mediterranean fever • Secondary syphilis • Hyperimmunoglobulinemia D syndrome Periodic fever syndromes Vasculitis : Palpable purpura Erythema Chronicum Migrans (Lyme disease) caused by Borrelia burgdorferi Dysaesthesia (Pain/ paraesthesia/ pruritus) without obvious primary lesion Delusion of parasitosis Neurodermatitis Neuropathy or stroke Notalgia paresthetica Polycythemia vera Porphyria Impending bullous impetigo, cellulitis Herpes virus infections Painful Nodules Eccrine spiradenoma Neurilemmoma Glomus tumor Leiomyoma Angiolipoma Dercum’s disease (adiposis dolorosa) Neuroma and neurofibroma (sometimes) Dermatofibroma (sometimes) Arthropod bite or sting Blue rubber bleb nevus Chondrodermatitis nodularis helicis Cutaneous endometriosis Erythema nodosum Erythema Nodosum Hypo/Depigmented Lesions Halo nevus Idiopathic guttate hypomelanosis Lichen sclerosus Lupus erythematosus (discoid lesions) Molluscum contagiosum Nevus depigmentosus Pityriasis alba Postinflammatory hypopigmentation Scars Stucco keratosis (keratosis alba) Tinea versicolor Vitiligo Albinism Chediak–Higashi syndrome Chemicals (hydroquinone, phenol, etc.) Hypomelanosis of Ito Incontinentia pigmenti Leprosy Nevus anemicus Piebaldism Pinta Tuberous sclerosis (ash-leaf macules) Hypopigmented mycosis fungoides Hypo-/Depigmented Lesions Hansens Post kalaazar dermal leishmaniasis Hypo-/Depigmented Lesions Discoid lupus erythematosus Vitiligo Hypo /Depigmented Lesions Hypopigmented mycosis fungoides. Malar Rash Clinical Entity Distinguishing clinical features Distinguishing laboratory features Acute cutaneous lupus erythematosus Photosensitivity, rash spares nasolabial folds; clinical evidence of active SLE Positive ANA with confirmed SLE serology and other laboratory parameters Dermatomyositis Violaceous erythema often with edema; involves eyelids, periorbital and/or malar areas but spares nasolabial folds; often pruritic Positive ANA, elevated muscle enzymes (amyopathic form can occur, however); myositisspecific autoantibodies Allergic contact or airborne dermatitis History of contact exposure Negative ANA, positive patchtest results Rosacea Papules and pustules Negative ANA Malar Rash Clinical Entity Distinguishing clinical features Distinguishing laboratory features Seborrheic dermatitis Greasy or scaly macules and papules that involve the nasolabial folds, cheeks, chin and scalp Negative ANA Eczematous (atopic) dermatitis Papulo-vesicular lesions after first sun exposure following winter in northern latitudes; might be difficult to distinguish from ACLE and photo-induced eruptions in early phases Negative ANA IgE can be elevated Malar Rash Clinical Entity Distinguishing clinical features Distinguishing laboratory features Polymorphous light eruption Papulo-vesicular lesions after first sun exposure might be difficult to distinguish from ACLE Negative ANA and photo-induced eruptions in early phases Photo-induced, drugrelated eruptions History of prior exposure, confined to sun-exposed areas Negative ANA Exaggerated flushing reactions (functional or medical, carcinoid, pheochromocytoma) Not photosensitive Negative ANA Malar Rash SLE Rosacea Thickened Nerves Mnemonic : LANDS • Leprosy • Amyloidosis • Neurofibromatosis • Diabetes • Sarcoidosis Bubo Cat-scratch disease Chancroid Lymphogranuloma venereum Tularemia Bubonic plague Genital Ulcer Disease Infectious Non-infectious Herpes simplex virus (HSV) Behcet’s disease Syphilis Squamous cell carcinoma Chancroid Trauma Lymphogranuloma venereum (LGV) Drug-induced Donavanosis Granuloma inguinale HIV Herpes progenitalis Bechet’s Disease Annular Lesions Annular macules or minimally elevated plaques Cutis marmorata Erythema multiforme Erythema ab igne Erythema chronicum migrans Erythema marginatum Livedo reticularis Purpura annularis telangiectoides Targetoid hemosiderotic hemangioma Annular papules or plaques with no scale Basal cell carcinoma Granuloma annulare Sebaceous hyperplasia Desmoplastic trichoepithelioma Sarcoidosis Granuloma annulare Annular plaques with some scale or crust Basal cell carcinoma Eczema, especially nummular Prurigo Annular lichen planus Lupus erythematosus (especially Ro-positive SCLE) Pityriasis rosea Psoriasis Reiter’s disease (circinate balanitis) Seborrheic dermatitis Tinea corporis CD30+ Anaplastic Large Cell T Cell Lymphoma Cutaneous small vessel vasculitis Annular plaques with some scale or crust Secondary Syphilis Tinea Corporis Prurigo Nodularis Annular plaques – infiltrative with or without scaling Lupus vulgaris Chromomycosis Hansen’s disease Elastosis perforans serpiginosa (EPS) Erythema annulare centrifugum ( EAC) Erythema gyratum repens (EGR) Erythrokeratodermia variabilis Ichthyosis linearis circumflexa Mycosis fungoides Porokeratosis Necrolytic migratory erythema Annular plaques Icthyosis linearis circumflexa Lupus vulgaris Erythema annulare centrifugum Annular plaques CD30+ Anaplastic Large Cell T Cell Lymphoma: Annular plaque with scaling and erythema along with subcutaneous nodules Annular vesicles or pustules Linear IgA bullous dermatosis Pemphigus Subcorneal pustular dermatosis Fixed drug eruption Subcorneal pustular dermatoses MCQ’s Q.1) A. B. C. D. All of the following may present as annular vesicles, except: Linear IgA bullous dermatosis Pemphigus Subcorneal pustular dermatosis Hansen’s disease Q.2) A. B. C. D. All of the following may cause genital ulcer, except : Herpes simplex Squamous cell carcinoma Cutis marmorata Behcet disease MCQ’s Q.3) A. B. C. D. All of the following may present with thickened nerves, except : Amyloidosis Cat scratch disease Neurofibromatosis Sarcoidosis Q.4) A. B. C. D. Malar rash with negative ANA is found in : Polymorphous light-induced eruption Acute cutaneous lupus erythematosus Systemic lupus erythematosus Dermatomyositis MCQ’s Q.5) A 8 year old child, came with chief complaints of hypopigmented lesion over forearm since last 8 months, The diagnosis of Leprosy was made based on the presence of the following except : A. Hypoaesthesia B. Hypohydrosis C. Hypotrichosis D. Loss of triple response of lewis Photo Quiz Q. Describe the lesion and give differential diagnosis. Photo Quiz Q. Give a differential diagnosis. Thank You!