Antidotes - Tripod.com
advertisement

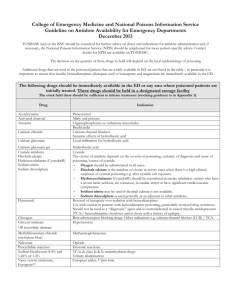
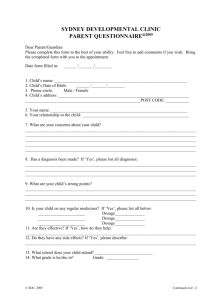
Antidotes Dr. F.L. Lau COS (AED) UCH Effective antidotes are limited Availability / stocking level variable Some very expensive (expire before use) Appropriate use can : reduce M&M avoid unnecessary investigation Not without risk—poison itself UCH Antidotes Use (1999-2004) Nalaxone NaHCO3 Glucagon No Antidotes NAC Calcium Atropine Flumazenil Physostigmine Antivenom Antidote Frequency Naloxone 136 (7%) N-acetylcysteine 57 (3%) Flumazenil 29 (2%) NaHCO3 11 (1%) Calcium 8 (0%) Physostigmine 3 (0%) Glucagon 1 (0%) Atropine 1 (0%) Antivenom 1 (0%) No Antidotes 1648 (87%) Use of Antidote Consider risk benefit ratio Patients clinical status (e.g. Benzodiazepine) Appropriate laboratory result (Panadol) Expected pharmaceutical action of toxin Possible adverse reactions of antidote Case1 F/30 mental patient Found unconscious in bed with suicidal note RR 10/min, BP 100/80, pulse 60/min Pupil small (E&R) SaO2: 98% After initial stabilization What antidote will you use? Drug induced coma A B C N O T alcohols & anticonvulsants barbiturate & benzodiazepine & other sedatives carbon monoxide & cyanide neuroleptics opiates & oral hypoglycemic TCA & other tranquilizers Relative produce empty bags of Doloxene, Mogadon & Sinequan When would you give Narcan? Anexate? NaHCO3? Naloxone (Narcan) Indications Reversal of CNS & respiratory depression in opioid poisoning Also effective for clonidine +/- ethanol/benzo/valproic acid Diagnostic use for coma patient Naloxone (Narcan) Dosage: 0.4-2mg I.V. bolus, can be repeated up to 10 mg For chronic user, titrate with low dose (0.1mg) upward Infusion usually indicated (T ½ ~ 1 hour) -2/3 initial effective close hourly Caution: Rapid reversion cause withdrawal seizure Pulmonary edema & vent. fibrillation Flumazenil (Anexate) Pure competitive benzodiazepine receptor antagonist Indications Post op or post procedure reversal of benzodiazepine sedation Rapid reversal of benzodiazepine – induced coma & resp. depression as a diagnostic aid or avoid intubation Flumazenil (Anexate) Cautions Oral benzodiazepine overdose never life-threatening In chronic user cause withdrawal & convulsion In polydrug overdose, removal of protective effective of benzodiazepine unmask convulsion or arrhythmia of TCA or cocaine Dosage: Titrate with response starting 0.2mg I.V. over 30 sec Up to 3mg Case1 F/30 mental patient Found unconscious in bed with suicidal note RR 10/min, BP 100/80, pulse 60/min Pupil small (E&R) SaO2: 98% Compatible with TCA poisoning? NaHCO3 Indications 1. Reverse sodium channel blockers overdose TCA Antiarrhythmic 1a: Quindine, procainamide & disopyramide 1c: Encainide & flecaimide Propanolol Propoxyphene (Doloxene) Phenothiazines (melleril) Diphenhydramine (benadryl) Cocaine Quinidine-like effect Myocardial depression – hypotension Reduce excitability – heart block Reduce conduction velocity – wide QRS Delay repolarization – prolong QTc Sodium ion load & alkalaemia reverse membrane depressant effects Indicated if QRS > 0.1 sec, hypotension & bradycardia Dosage: 1-2mEq/Kg bolus repeated q 5-10 min till pH: 7.45-7.5 or QRS shorten to normal NaHCO3 2. Urinary alkalinazation Enhance elimination of salicylate & phenobarbital Prevent renal deposition of myoglobin after rhadomyolysis 100 ml NaHCO3 in 1 litre of D5 in 0.25% saline at 150ml/hour Adjust rate to maintain urine pH7-8 Add 20 mEq/L of potassium NaHCO3 3.Correction of Acidaemia For poisoning of methanol ethylene glycol salicylate What if the patient taken a bottle of industrial alcohol ? What antidote to use? Ethanol Compete with methanol/ethylene glycol Higher affinity for alcohol dehydrogenase Allow toxic alcohol excreted avoiding toxic metabolite production Indication Symptoms of toxicity/anion gap metabolic acidosis with history of ingestion Ethanol Dosage: Loading: 750 mg/kg Maintenance: 100-150 mg/kg/hr to keep serum level 100mg/dL Increase rate with dialysis (Fomepizole : not A/V in HK) Case II M/30 Well all along Recent depression after diagnosis of T.B. Status epilepticus 1 hour after dinner Poor response to all anticonvulsants What is your DDX? Drug induced convulsion Status epilepticuts Organophosphate Tricyclic antidepressant Isoniazid Sympathomimetic Amoxopine INAH Camphor, cocaine cocaine Amphetamines Methylxanthines Phencyclidine Benzodiazepine withdrawal Ethenol withdrawal Lithium, lidocaine Lead Amphetamines theophylline ethanol withdrawal Lead Tetramine Pyridoxine (vit B6) INAH inhibit brain pyridoxal phosphate decrease GABA levels causing repeated seizure block liver metabolism causing lactate acidosis High dose Pyridoxine control the convulsion Also correct the lactic acidosis Adjunct therapy for ethylene glycol poisoning (Glyoxylic acid to glycine) Dosage: 1 gm pyridoxine per gram of INAH or empirically 5g I.V.I. If no response, think of tetramine Especially if no evidence of suicidal drug ingestion DMPS Sodium dimercaptopropane sulfonate is related to BAL (dimercaprol) & succimer (dimercaptosuccinic acid) All are chelating agents DMPS & succimer also useful for nonmetalic pesticide -Tetramine R1 H S C H S C H H R2 R2 R1 Compound H CH2OH BAL COOH COOH Succimer CH2SO2Na H DMPS Mechanism of action unknown (? Dithiol group) Proven in animal study control convulsion & mortality Many studies in China show effectiveness Study not vigorous Journal of China Clin Med 2002 Cheng Kids Rx Death Disable 20 DMPS + Valium 0 0 4 Luminal + Valium 3 1 Henan Journ Pract Neuro Diseae: Yee 10 DMPs 0 deaths 11 control 2 deaths Action within 30 min. reduce convulsion Side effect mild: allergic reactions, vertigo & weakness Dosage No standard protocol Na-DMPS 0.25 mg IMI (0.5 mg/kg for child), response within 30 mins Can be repeated 30-60 min. to max. 1gm/day Then 2 doses on D2 Then 1 dose daily for 2-3 weeks Adjunct therapy Vit B6 0.5-1.5/D I.V. plasmaphoresis If taken huge dose of organophosphate, what is the antidote? Atropine For organophosphate or carbamate poisoning Anti-muscarinic effect & central effect Will not reverse nicotinic effects Dosage: 1mg I.V. titrated as needed May need huge doses Endpoint: drying of secretions and lung clear Pralidoxime Reverse cholinesterase inhibition Reactivate phosphorylated cholinesterase enzyme (before it aged) Most pronounced with organophosphate Also in carbamate with nicotinic toxicity May precipitate myasthenic crisis Rapid infusion : tachycardia, laryngospasm, muscle rigidity Pralidoxime Dosage: 1-2 gm IV over 30 min Repeat the dose if muscle weakness not improved Followed by infusion 200-500 mg/hr May need several days (for fat soluble one, avoid intermediate syndrome) Patient was on TCA, which is known to have anticholinergic property What is the antidote for anticholingergic poisoning? Should we use it? Physostigmine Reversible inhibitor of acetyl cholinesterase Tertiary amine cross BBB exerting central cholinergic effects Onset of action a few minute & half life ~ 30 min Non-specific arousal reticular activating system Physostigmine Indication Severe anticholinergic poisoning – agitated delirium, seizure + (coma, severe hypertension, arrhythmia and hypothermia). Sometimes diagnostic test for delirium (functional/anticholinergic) Physostigmine Contraindications Not for TCA poisoning Not for non-specific coma Aggravate arrhythmia & induce convulsion Unless pure anticholinergic toxidrome Not with depolarizing NM blockers (scoline) Dosage Diagnostic trial 1mg IV slowly over 5 min Therapeutic 0.5mg I.V. repeated every 5 min till 2mg or desired effect Atropine standby to reverse excessive muscarinic stimulation Case III M/30 Worker caught in factory fire No burn nor smoke inhalation, SaO2 90% Persistent hypotension, acidosis What antidote to use? Oxygen 100% or hyperbaric For possible carbon monoxide poisoning Also for : hypoxaemia from toxic lung injury Cellular respiration inhibitor (cyanide & H2S) Use with care in paraquat poisoning aggravate lipid peroxidation in lung resulting in fibrosis) Co-oximetry: COHb level: 10% What antidote to use? Cyanide Kit Sodium nitrite (Amyl nitrite) Produce cyanide – scavenging methemoglobin 1 dose produce 20-30% met Hb C/1 pre-existing methemoglobinaemia > 40% hypotension & concurrent CO poisoning Dosage: NaNO2 300mg I.V. over 3-5min Half dose can be repeated if no response within 30 min Sodium thiosulphate Sulfur donor that promote convertion of cyanide to thiocyanate Non-toxic can be used empirically Also for prophylaxis during Nitroprusside infusion Cause burning sensation, muscle clamping & twitching Dosage: 12.5g IV at 5ml/min Half dose can be repeated after 30-60 min Hydroxocohalamin Synthetic form of Vit B12 Exchange with plasma cyanide to give non-toxic cyanocobalamin Minimal adverse effect Brown coloration of body fluid (interfere lab test) Nausea/vomiting Muscle twitching & spasm Dosage: Give 50 times of cyanide exposed or empirically 4gm Other antidotes Methanol Ethanol Ethylene glycol Fomepizole* Panadol Acetylcysteine Calcium channel blocker Ca cl Hydrogen floride Ca gluconate Oral hypoglycaemic D50 Insulin Octreotide Arseric, Hg, Lead Dimercaprol, Succimer* Beta blockers Glucagon Methaemoglobinaemia Methylene blue Warfarin Vit K1 Iron Deferoxamine Other antidotes Heparin Protamine sulphate Methotrexate, Methanol Folinic acid* Valproic acid carnitine* Digoxin Digoxin-specific antibodies (digibind) Stone fish sting Stone fish antivenom Bamboo snake specific antivenin Russell riper Chinese Cobra King Cobra Banded Krait Botulism Botulinum antitoxin* Minimal Stocking Level AED Hospital Know where to get at odd hour Need a central station (PCC?) Stock taking in all AEDs/Hospital Pharmacies Thank you