Improving Follow-up to abnormal cervical pathology results at
advertisement

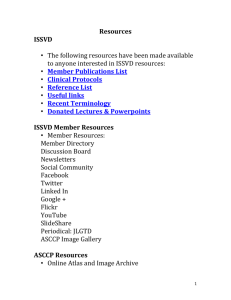
Tom Garvey, BS, M2 Ann Evensen, MD Helen Luce, DO Two main types ◦ Adenocarcinoma ◦ Squamous cell carcinoma Asymptomatic Develop slowly Risk factors Cytology ◦ ◦ ◦ ◦ High sensitivity Conventional glass slide Liquid-based cytology ASCUS, ASC-H, LGSIL, HGSIL, AIS, AGUS HPV Testing Normal vs. Abnormal Cervical Cells Histology: Colposcopy ◦ ◦ ◦ ◦ Visual examination Biopsy High specificity CIN-1, 2, or 3; Cancer Excisional Procedures ◦ Loop Electrosurgical Excision Procedure (LEEP) ◦ Cold cone excision LEEP ASCCP – algorithms for cytological and histological results4 Barriers to screening Imperfect tests Loss of follow-up to abnormal results ◦ Patient factors ◦ Provider error Special challenges at residency clinics Intervention Results Telephone counseling on psychological concerns/barriers Improves initial and long-term adherence Educational brochure/pamphlet Improves adherence Electronic tracking system Improves adherence Family physician involvement in follow-up Improves adherence Result reminder letters from cytologist to physician Improves adherence, especially with older patients Framing of result messages to patient Not shown to be effective Economic Reimbursement Improves adherence in disadvantaged patients Using an electronic tracking system to manage patients with abnormal cervical cytology will improve both communication of next steps to the patient and patient adherence with these steps at two family medicine residency clinics Data sources: Timeframes: Intervention Scoring care: ◦ UW-Verona Family Medicine Clinic ◦ UW-Wausau Family Medicine Clinic ◦ Index Pap ◦ Pre-intervention: 11/2005 - 11/2007 ◦ Post-intervention: 11/2008 - 11/2010 ◦ Spreadsheet ◦ Follow ASCCP guidelines (3 month window) ◦ Early testing appropriate ◦ Extra vigilant care appropriate If appropriate care took place, assumed communication was appropriate Inappropriate steps ◦ Review communication ◦ Attribute loss of follow-up (patient or provider) Scoring stopped after an inappropriate step Referrals appropriate Transfer of care Adolescents excluded from post-intervention results 72 Patients 5 Patients Excluded 4 History Questions 1 Chart Incomplete 67 Patients 62 Patients 9 Patients Excluded 6 Care Transferred 2 Index Pap not at Clinic 1 Chart Incomplete 53 Patients 127 Patients Las 23 Patient Excluded 13 Adolescents 9 Care Transferred 1 Superceding Provider Judgment 104 Patients 77 Patients Las 8 Patients Excluded 5 Care Transferred 3 Adolescents 69 Patients Patient Care: ◦ Percentage of follow-up steps that were appropriate Provider Communication: ◦ Percentage of follow-up steps that had correct provider communication Significance of Results: ◦ analyzed with Fisher’s test Key: V – Verona W - Wausau # of Steps with Appropriate Care # of Steps with Delayed or Absent Care Percent of Steps with Appropriate Care Clinic V W V W V W Preintervention 82 76 27 24 75.2% 76.0% Postintervention 133 76 31 23 81.1% 76.8% 5.9% 0.8% Improvement: P=0.29 P=1 Key: V – Verona W - Wausau # of Steps where Patient Received Adequate Communication # of Steps where Patients Received Either No or Erroneous Communication Percent of Steps with Adequate Communication Clinic V W V W V W Preintervention 93 87 16 13 85.3% 87.0% Postintervention 153 89 8 10 95.0% 89.9% 9.7% 2.9% Improvement: P=0.0082 P=0.66 Study not complete Challenges: ◦ ◦ ◦ ◦ Change in ASCCP guidelines Implementation of EMR Difficulty in judging communication of next steps Clinicians not interpreting algorithms correctly, especially post-colposcopy follow-up Next Steps ◦ ◦ ◦ ◦ Continue spreadsheet use Track remaining patients Provider Education Intervention Tailoring: Initiating incentives, paying for care or transportation, informational brochures Ann Evensen, MD - project advisor Anna Hendrickson, RN – project member Laura Kutzke – program coordinator Helen Luce, DO – project advisor Clarissa Renken, DO – project member Mark Shapleigh – clinic manager Jon Temte, MD,PhD – program director 1. 2. 3. 4. American Cancer Society - Cancer Facts & Figures 2009. At: http://www.cancer.org/acs/groups/content/@nho/document s/document/500809webpdf.pdf (Accessed July 13th 2010). Parkin, DM, Pisani, P, Ferlay, J. Global cancer statistics. CA Cancer J Clin 1999; 49:33. National Cancer Institute – Current Research: Health Disparities: Cervical Cancer. At: http://dceg.cancer.gov/research/healthdisparities/cervical (Accessed July 13th 2010). American Society for Colposcopy and Cervical Pathology – Consensus Guidelines: 2006. At: http://www.asccp.org/pdfs/consensus/algorithms_cyto_07.p df (Accessed July 13th 2010).