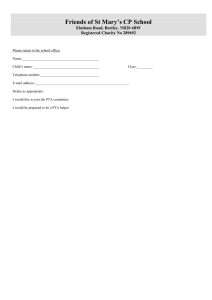
essential abilities
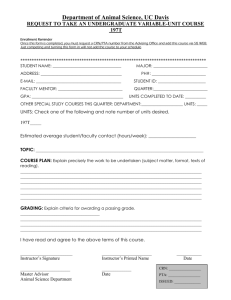
advertisement

Clinical Instructor Handbook 2013 – 2014 Physical Therapist Assistant Program St. Philip’s College St. Philip’s College Physical Therapist Assistant Program Clinical Instructors Handbook Table of Contents Welcome ........................................................................................................................ 2 General Information......................................................................................................... 3 A Philosophy........................................................................................................ 3 B Mission and Goals............................................................................................ 3 C Non-Discrimination Policy ................................................................................ 3 D Accreditation .................................................................................................... 4 Physical Therapist Assistant Curriculum ......................................................................... 4 Course Descriptions ........................................................................................................ 5 Course Sequencing ......................................................................................................... 7 Professionalism in Physical Therapy: Core Values ......................................................... 7 Generic Abilities .............................................................................................................. 8 Essential Abilities ............................................................................................................ 8 Clinical Policies A Clinical Evaluation .......................................................................................... 10 B Grade Compilation ......................................................................................... 10 C Clinical Attendance ........................................................................................ 10 D Clinical Assignments ...................................................................................... 11 E Clinical Attire .................................................................................................. 11 Safety and Health Information A Immunizations ................................................................................................ 11 B Criminal Background and Drug Screens ........................................................ 12 C Blood and Body Fluid Exposure ..................................................................... 12 D Clinical Safety & Competent Practice ............................................................ 12 E Incident Report ............................................................................................... 12 F Accident/Health Insurance.............................................................................. 13 G Confidentiality/HIPAA/Laws ........................................................................... 13 Suggestions for Clinical Instructors ............................................................................... 13 A Expectations for a Clinical Instructor .............................................................. 14 B Clinical Education Faculty Development ........................................................ 15 Web Sites of Interest ..................................................................................................... 16 Appendices Appendix A – Protocol for Sharp Puncture, Blood or Potentially Infectious Body Fluids Exposure ....................................................................................................................... 18 Appendix B – Student Clinical Incident/Injury Form ...................................................... 19 Appendix C – Patient Survey ........................................................................................ 20 Welcome Thank you for your interest in the clinical education of our students, your future physical therapist assistants. You are instrumental in the clinical education process of our students. You will guide them in taking the academic information they have learned in the classroom and apply it to the “real world” in your clinic. The purpose of this handbook is to provide the CCCE and CI with the information and resources needed to prepare for the clinical experience and assess the facility’s clinical education program. St. Philip’s College PTA students complete three clinical courses which begin in the summer between the first and second year of the program. The summer clinical is 160 hours in length over four weeks. The final rotations are in the spring of year two after all academics have been completed. Rotation two is 240 hours over six weeks and the last rotation is 280 hours over seven weeks. The students will receive a variety of experiences in multiple physical therapy settings. All of the St. Philip’s College Health Sciences students are required to complete immunizations, a criminal background check, and a drug screen prior to clinical rotations. They have all completed CPR for the healthcare provider. Each of the students has completed the required course work in HIPPAA, and has viewed the required Healthcare films that include fire safety, blood borne pathogens, TB, and HIPPAA. Please let us know if we can assist you in any way. If you would like a clinical instructor or PTA MACS information session, or if you have questions please call Mary Hays, ACCE. Laura Miele, PTA, BSOE, Program Director, Instructor Office: 210.486.2443, Cell: 210.288.3433 lmiele@alamo.edu Donna Stetz, PT, MA, Instructor Office: 210.486.2051 dstetz@alamo.edu Mary Hays, PTA, BSOE, ACCE/Instructor Office: 210.486.2051, Cell: 210.325.2880 mhays@alamo.edu St. Philip's College PTA program web site: http://www.alamo.edu/spc/pta St. Philip’s College – PTA Program Clinical Instructors Handbook Page 2 of 20 GENERAL INFORMATION Philosophy The PTA program supports the goals and mission of the Allied Health Department, St. Philip’s College, and the Alamo Community Colleges. Our purpose is to provide our students with a high quality attainable education, a curriculum designed to keep pace with the ever changing healthcare field, and an atmosphere that welcomes diversity of cultures and ideas. Students are encouraged to develop the skill of self-directed learning as well as an understanding of their role as part of a healthcare team. Faculty shall promote the practice of physical therapy by teaching skills consistent with the profession, by modeling and teaching compassionate care and responsible use of healthcare resources, and by encouraging the highest degree of integrity and ethical standards. Mission and Goals The Physical Therapist Assistant program serves the community by facilitating the preparation of our students for a career in physical therapy while encouraging personal growth, critical thinking, ethical behavior and lifelong learning. The goals of the Physical Therapist Assistant Program are to: 1. equip each student with the tools to achieve his/her goal of graduating from the program and securing state licensure for practice as a physical therapist assistant in an ethical and professional manner under the supervision of a physical therapist. 2. prepare each student to operate as a general practitioner capable of critical thinking and responding to changes in healthcare delivery and increasing technological advances. 3. encourage each student to pursue lifelong learning and regularly engage in service to his/her community. 4. encourage students to engage in continued professional growth. 5. promote professional collaboration with other healthcare professionals. 6. support the development of graduates as educators and clinicians. Non-Discrimination The Alamo Community College District, including its affiliate colleges, does not discriminate on the basis of race, religion, color, national origin, sex, age, sexual preference, or disability with respect to access, employment, programs or services. Inquiries or complaints concerning these matters should be brought to the attention of: Associate Vice Chancellor of Human Resources EEO Official/Title IX Coordinator Human Resources Department 201 W. Sheridan, Bldg A, Suite 119 San Antonio, TX 78204 (210) 485-0200 St. Philip’s College – PTA Program Clinical Instructors Handbook Page 3 of 20 Accreditation St. Philip’s College is approved and accredited by the Texas Higher Education Coordinating Board, National Accrediting Groups for Allied Health and Nursing Programs, and the Federal Aviation Administration. The Physical Therapist Assistant Program at St. Philip’s College was first granted accreditation status by the Commission on Accreditation in Physical Therapy Education in 1973. It was re-accredited in 1984, 1990, 1998, and most recently in 2009 St. Philip’s College is fully accredited by the Commission on Colleges of the Southern Association of Colleges and Schools to award degrees in Associate of Arts, Associate of Science, Associate of Applied Science, and Certificates of Completion. The latest accreditation was awarded in 2006. PTA Curriculum Year 1 Semester 1 PTHA 1301 Profession of Physical Therapy PTHA 1321 Clinical Pathology PTHA 1431 Physical Agents BIOL 2401 Human Anatomy & Physiology I Semester 2 PTHA 1413 Functional Anatomy PTHA 1405 Basic Patient Care Skills PTHA 2409 Therapeutic Exercise BIOL 2402 Human Anatomy & Physiology II Summer Semester 3 PTHA 2201 Essentials of Data Collection PTHA 1360 Clinical I – Physical Therapist Assistant ENGL 1301 Freshman Composition I St. Philip’s College – PTA Program Clinical Instructors Handbook Page 4 of 20 Year 2 Semester 4 PTHA 2435 Rehabilitation Techniques PTHA 2431 Management of Neurological Disorders MATH 1314 College Algebra or higher HUMA Three credit hours of Humanities Semester 5 PTHA 2217 Issues in Health Care PTHA 2460 Clinical II – Physical Therapist Assistant PTHA 2461 Clinical III – Physical Therapist Assistant PSYC 2301 General Psych or Introduction to Psych COURSE DESCRIPTIONS BIOL 2401. Human Anatomy and Physiology I. Basic chemistry, the cell, tissues, the skeletal, muscular and nervous systems, and the senses. BIOL 2402. Human Anatomy and Physiology II. Fundamental principles of body systems and their functions. Satisfies the requirements of human anatomy and physiology for some Paramedical and Allied Health curricula. ENGL 1301. Freshman Composition I. Emphasizes training in reading and writing skills. Course requires expository essays based on provocative and critical readings. A student must earn a passing grade in English 1301 before enrolling in English 1302.(English 1301 and 1302 cannot be taken concurrently). Math 1314. College Algebra. Topics include functions, including algebra of functions, composites, inverses, graphs, Remainder Theorem, Factor Theorem, Rational Root Theorem, logarithmic and exponential functions; systems of equations using Cramer=s Rule; matrices and determinants; Binomial Theorem; and arithmetic and geometric sequences and series with Sigma notation. PSYC 2301. General Psychology. A study of the foundations and principles of behavior. The brain, motivation, emotions, learning theories, sensations, and personality theories will be studied. or Intro to Psychology St. Philip’s College – PTA Program Clinical Instructors Handbook Page 5 of 20 PTHA 1301. The Profession of Physical Therapy. Introduction to the profession of physical therapy including the historical and current scope of physical therapy. PTHA 1321. Clinical Pathophysiology. Study of the pathogenesis, prognosis, and therapeutic management of diseases/conditions commonly encountered in physical therapy. PTHA 1431. Physical Agents Study of the biophysical principles, assessment, and application of therapeutic physical agents with specific emphasis on indications, contraindications, medical efficacy, and physiological effects. PTHA 1413. Functional Anatomy. Study of human anatomy and its application to the motion of the musculoskeletal system as it relates to normal activities and dysfunctions. Integration of skills related to the kinesiological assessment of the human body. PTHA 1305. Basic Patient Care Skills. Introduction to the theory and application of basic patient handling, functional skills, assessment techniques, and measurement techniques. PTHA 2409. Therapeutic Exercise. Critical examination of concepts and application of techniques related to therapeutic exercise and functional training. PTHA 1360. Clinical I - Physical Therapist Assistant A method of instruction providing detailed education, training, work-based experience, and directed patient/client care generally at the clinic site. Specific detailed learning objectives are developed for each course by the faculty. On-site clinical instruction, supervision, evaluation, and placement is the responsibility of the College faculty. Course may be repeated if topics and learning outcomes vary. PTHA 2435. Rehabilitation Techniques. Advanced course integrating previously learned and new skills into the comprehensive rehabilitation of selected long-termed pathologies. PTHA 2431. Management of Neurological Disorders. Advanced course integrating previously learned and new skills/techniques into the comprehensive rehabilitation of selected neurological disorders. PTHA 1317. Issues in Health Care. Exploration of the organizational patterns, administrative principles, legal and ethical issues, communications, and job placement skills in physical therapy and health care St. Philip’s College – PTA Program Clinical Instructors Handbook Page 6 of 20 PTHA 2460. Clinical II - Physical Therapist Assistant. A method of instruction providing detailed education, training, work-based experience, and directed patient/client care generally at the clinic site. Specific detailed learning objectives are developed for each course by the faculty. On-site clinical instruction, supervision, evaluation, and placement is the responsibility of the College faculty. Course may be repeated if topic and learning outcomes vary. PTHA 2461. Clinical III - Physical Therapist Assistant. A method of instruction providing detailed education, training, work-based experience, and directed patient/client care generally at the clinic site. Specific detailed learning objectives are developed for each course by the faculty. On-site clinical instruction, supervision, evaluation, and placement is the responsibility of the College faculty. Course may be repeated if topic and learning outcomes vary. COURSE SEQUENCING Throughout the curriculum, each PTA program course offered by the Department of Health Sciences must be taken in sequence. These courses can only be taken during the semester in which they are officially listed. PROFESSIONALISM in PHYSICAL THERAPY: CORE VALUES Accountability is the active acceptance of responsibility for the diverse roles, obligations, and actions of the physical therapist assistant, including self-regulation and other behaviors that positively influence patient/client outcomes, the profession, and the health needs of society. Altruism is the primary regard for or devotion to the interest of patients/clients, thus assuming the fiduciary responsibility of placing the needs of the patient/client ahead of the physical therapist assistant’s self interests. Compassion is the desire to identify with or sense something of another’s experience; a precursor of caring. Caring is the concern, empathy, and consideration for the needs and values of others. Cultural and linguistic competence is a set of congruent behaviors, attitudes, and policies that come together in a system, agency, or among professionals that enables effective work in cross-cultural situations. Duty is the commitment to meeting one’s obligations to provide effective physical therapy services to individual patients/clients, to serve the profession, and to positively influence the health of society. Integrity is steadfast adherence to high ethical principles or professional standards; truthfulness, fairness, doing what you say you will do, and “speaking forth” about why you do what you do. Social Responsibility is the promotion of a mutual trust between the physical therapist assistant, as a part of the profession, and the larger public that necessitates responding to societal needs for health and wellness. St. Philip’s College – PTA Program Clinical Instructors Handbook Page 7 of 20 GENERIC ABILITIES Generic abilities are attributes, characteristics, and behaviors that are not specifically part of the PT core knowledge but are required for successful practice in the profession. The ten Generic abilities and definitions developed by UW-Madison are: 1. Commitment to Learning: The ability to self-assess, self-correct, and self-direct; to identify needs and sources of learning; and to continually seek new knowledge and understanding. 2. Interpersonal Skills: The ability to interact effectively with cultural and ethnic diversity issues. 3. Communication Skills: The ability to communicate effectively (i.e., speaking, body language, reading, writing, listening) for varied audiences and purposes. 4. Effective Use of Time and Resources: The ability to obtain the maximum benefit from a minimum investment of time and resources. 5. Use of Constructive Feedback: The ability to identify sources of and seek out feedback and to effectively use and provide feedback for improving personal interaction. 6. Problem-Solving: The ability to recognize and define problems, analyze data, develop and implement solutions, and evaluate outcomes. 7. Professionalism: The ability to exhibit appropriate professional conduct and to represent the profession effectively. 8. Responsibility: The ability to fulfill commitments and to be accountable for actions and outcomes. 9. Critical Thinking: The ability to question logically; to identify, generate, and evaluate elements of logical argument; to recognize and differentiate facts, illusions, assumptions, and hidden assumptions; and to distinguish the relevant from the irrelevant. 10. Stress Management: The ability to identify sources of stress and to develop effective coping behaviors. Developed by the Physical Therapy Program, University of Wisconsin-Madison. May, et al. Journal of Physical Therapy Education. 9:1, Spring 1995. ESSENTIAL ABILITIES PHYSICAL THERAPIST ASSISTANT PROGRAM 1. Visual Acuity: a. Acute enough to read small printed materials such as a health record/computer screen. b. Acute enough to read small calibrations or symbols such as on a goniometer or modality equipment normally found in a physical therapy clinic. St. Philip’s College – PTA Program Clinical Instructors Handbook Page 8 of 20 c. Acute enough to obtain visual information including but not limited to movement, posture, body mechanics, and gait pattern. 2. Hearing Acuity: a. Acute enough to perceive normal level of voice so as to follow instructions and participate in conversation. b. Acute enough to collect sounds produced in the body by use of a stethoscope. 3. Communication: a. Verbal expression sound enough to express one’s thoughts and distinct enough to communicate using medical terminology and the terminology of physical medicine. b. Able to perceive non-verbal communication such as changes in mood, activity, facial expression, and postures. c. Able to communicate effectively and sensitively; requires the ability to read and write, utilizing the English language. 4. Digital Dexterity: a. Agile enough to operate the various pieces of modality equipment normally found in a physical therapy clinic. b. Agile and strong enough to administer a variety of massages and other manual therapies. 5. Physical Ability: a. Strong and agile enough to lift or assist in lifting persons in excess of 100 pounds on a frequent basis and to assist persons in: 1) climbing 5) crouching 2) balancing 6) crawling 3) stooping 7) reaching 4) kneeling b. Fine and gross motor skills necessary for administering CPR (cardio-pulmonary resuscitation) 6. Interpersonal and Behavioral Ability: a. Able to complete treatment modalities or procedures within time allotted for patient. b. Able to complete required tasks/functions effectively under stressful conditions. c. Able to utilize problem solving skills and exercise sound judgment. d. Able to adapt to changing environments in a mature, sensitive and effective manner. Reference: “Selected Characteristics of Occupations Defined in the Dictionary of Occupational Titles”. CLINICAL POLICIES A primary objective of clinical assignments is to insure that each student is exposed to a variety of clinical settings/environments during the course of the three (3) assignments. Different types of clinical environments include acute hospital settings, private clinics, nursing homes, home health care agencies, and rehabilitation hospitals. St. Philip’s College – PTA Program Clinical Instructors Handbook Page 9 of 20 Schedule: 2013 – 2014 Affiliation 1: Summer – 4 weeks, 160 hours; June 24, 2013 – July 19, 2013 Affiliation 2: Spring – 6 weeks, 240 hours; January 27, 2014 – March 7, 2014 Affiliation 3: Spring – 7 weeks, 280 hours; March 17, 2014 – May 2, 2014 Students are assigned to clinical sites by the Academic Coordinator of Clinical Education (ACCE) with input from the student and the clinical coordinator. Students may not change their clinical assignments, though special situations may be discussed. The experiences are designed to provide directed learning in an assortment of professional and clinical settings. Clinical Evaluation The clinical instructor (CI) is responsible to assess the student’s progress at the assigned clinical affiliation with the use of the PTA MACS. The document allows for an objective assessment of the student’s skills during the clinical rotation. The progress reports (pink forms pg 1-6) in the students PTA MACS are utilized for a mid-term and final assessment of the student. The mid-term evaluation is completed by the CI, discussed with the student, and reviewed by the academic coordinator of clinical education (ACCE) during the mid-term clinic site student visit. A summative progress report must be completed by the CI at the end of the clinical rotation and the results discussed with the student. The student will return all completed forms to the ACCE for review and grade computation. An explanation of the use of the PTA MACS can be found in the goldenrod page of the PTA MACS or at the following web site: http://www.alamo.edu/uploadedFiles/St_Philips_College/Library/Files/AlliedHealth-PTAMACSInstruction.pdf Grade Compilation The final clinical grade is based on a combination of skill attainment in the PTA MACS, other clinical assignments such as the journal and journal paper, accurate completion and return of all required forms, and attendance. Student adherence to policies and procedures and level of professionalism are also considered during the final grade assessment. Clinical Attendance Regular and punctual clinical attendance is required. Absences are permitted only for unavoidable circumstances, and the ACCE (Mary Hays) must be notified. Days absent must be made up prior to the end of the affiliation and at the convenience of the Clinical Instructor. Only one make-up date will be allowed each clinical affiliation. Additional make-up time will be at the discretion of the ACCE (Mary Hays). Students are not in clinical on St. Philip’s College scheduled holidays. The student is required to “clock–in & out” on the time sheet provided. The form must be initialed by the C.I. at the end of each week and signed at the end of the clinical rotation. This form will be presented for inspection to the ACCE during mid-term evaluation and turned in at the conclusion of the semester. The student’s work hours during each affiliation should be approximately 8 hours/day or 40 hours/week, mirroring the schedule of the Clinical Instructor (CI). St. Philip’s College – PTA Program Clinical Instructors Handbook Page 10 of 20 Students that are absent 10% or more of the total clinical hours will be dropped from the course. Clinical Assignments The student must have the PTA MACS with them at all times while in clinical. The PTA MACS and time sheet must be kept updated. The student will write five SOAP notes. The Clinical Instructor is to co-sign each note. A clinical journal is maintained (at least 2 entries/wk) throughout all three rotations. A clinical journal paper is to be turned into the ACCE at the completion of rotation # 1. A clinical case study is to be completed during rotation # 2. Additionally each student is to present an in-service during the final rotations 2 &/or 3. This is at the discretion of the CI at each of those sites. Clinical Attire Docker type slacks – navy or khaki, polo type shirt- solid color with collar (no tee shirts or blue jeans), closed toed shoes preferably clean white tennis shoes, minimal jewelry – wedding band, stud earrings (no piercing jewelry other than ears), watch with a second hand, St. Philip’s College picture name tag must be worn at all times; solid color scrubs may be worn if that is the “uniform” for the facility. Hair should be neat and clean, worn away from the face. Fingernails should be clean and neatly filed. The fingernails should not extend beyond the fingertips. No colored nail polish is acceptable. All tattoos should be covered. SAFETY and HEALTH INFORMATION Immunizations All students accepted into an Allied Health program at St. Philip’s College must present evidence that the following immunization requirements have been met before the student is allowed to begin clinical practicum I. The student must present documentation from a physician or medical clinic of the following immunizations: a. One dose of Tetanus and Diphtheria toxoid (Td) within last 10 years. b. Measles/Mumps/Rubella (MMR) (a total of two doses required). Measles- Students born on or after Jan 1, 1957 must show acceptable evidence of vaccination of two doses of measles-containing vaccine administered since Jan 1, 1968, or acceptable evidence of immunity. Mumps- Students born on or after Jan 1, 1957 must show acceptable evidence of vaccination of one dose of mumps vaccine or acceptable evidence immunity. Rubella- Students must show acceptable evidence of vaccination of one dose of rubella vaccine or acceptable evidence of immunity. c. Mantoux test (TB). A PPD skin test must be done within one year prior to clinical assignment and must be repeated once a year, or more frequently if required by a specific clinic site. If PPD is positive, student must have a cleared chest X-ray. d. Hepatitis A- two doses. If vaccine received 10+ years ago, a booster shot or proof of immune status must be provided. St. Philip’s College – PTA Program Clinical Instructors Handbook Page 11 of 20 e. Hepatitis B series- three doses. If vaccine received 10+ years ago, a booster shot or proof of immune status must be provided. f. Varicella- two doses of varicella, unless the first dose was received prior to 13 years of age, or acceptable evidence of immunity, or letter from physician stating you have had the disease. g. Meningitis- a single dose if under the age of 30yrs. h. Flu – one per season. Written documentation of the above immunizations is maintained in the student’s file in the office of the program director. Cardio Pulmonary Resuscitation (CPR) All students are required to have current training in CPR for the healthcare provider (2 year card). Student Criminal Background and Drug Screens All students are required to have a cleared criminal background check and a cleared drug screen before attending clinical rotations. These records are maintained in the student’s file in the office of the program director. Blood and Body Fluid Exposure The students of St. Philip’s College Physical Therapist Assistant Program have been given in the curriculum, information regarding known risks for various diseases and have been provided skills to implement precautions appropriate to these risks. It is the responsibility of the student to implement standard precautions in the care of all assigned patients. See appendix A – Protocol for Sharp Puncture, Blood or Potentially Infectious Body Fluids Exposure Clinic Safety and Competent Practice All students have been introduced to the basic incidents and emergencies that can occur in a hospital or clinical setting, including infection control, codes and fire safety. All students have been instructed in the following skills: taking vital signs, wheelchair use and maintenance, transfer training, gait training, aseptic technique, wound care, extremity wrapping, physical agents and manual modalities. These skills are evaluated by faculty through skills tests or check-offs. Students must pass all practical exams with a grade of 77% or higher. If the student performs the critical safety elements incorrectly during the skill application the instructor will discontinue the treatment and the student will fail that skill. He/She must be re-tested on that skill until a passing grade is achieved. All skills on the check-off list must be successfully completed to pass the course. It is the student’s responsibility to maintain a safe environment for patient/client treatment. Incident Report An incident is anything happening to a patient, an employee, a visitor or the student that is out of the ordinary, inconsistent with the facility’s usual routine or treatment procedure, or an accident or situation that could cause an accident. In the event of an incident, the student should follow the protocol of the clinical facility, which may include filing an incident report at the facility. In addition, the student must complete the St. Philip’s College Allied Health Department Student Clinical Incident/Injury Form. See appendix B St. Philip’s College – PTA Program Clinical Instructors Handbook Page 12 of 20 The student must make every attempt to complete the written report within 24 hours of the incident, if at all possible, to ensure proper care and follow-up. Accident/Health Insurance All students are required to have health care insurance. Any health care costs incurred while the student is enrolled in the college is the responsibility of the student. Student health insurance is available in the College Health Center located in the Sutton Learning Center on campus. When all students register for courses at SPC, they automatically purchase Plan I: Compulsory Student Injury Insurance Plan. Before enrolling in a clinical course, all allied health students must either purchase Plan II: Student Sickness and Dependent Injury Insurance Plan, or produce evidence of an outside insurance policy that covers sickness and injury. Confidentiality/HIPAA/Laws The Family Educational Rights and Privacy Act (FERPA) affords all students certain rights with respect to their educational records. The college and program abide by this law and will not disclose any information about the student or his/her academic performance with any other person unless written permission is given by the student. Further information about this policy can be found in the St. Philip’s College Student Policy Manual. The PTA student is also expected to follow confidentiality in providing patient care at any healthcare facility assigned by the Clinical Instructor as part of a designated course of study. The student may not access, use, disclose or reproduce any confidential patient information other than for the strict purposes outlined in the student’s clinical duties. The student agrees to this policy by signing the Confidentiality Agreement which is located in the student’s file in the PTA program directors office. All students are instructed in the role of the PTA according to the Texas Practice Act and Rules; appropriate guidelines for supervision of the PTA and PT Aide in the different clinical settings; American Physical Therapy Association Standards of Ethical Conduct for the Physical Therapist Assistant. SUGGESTIONS FOR CLINICAL INSTRUCTORS 1. Familiarize yourself with the PTA MACS skills, objectives, and the grading criteria early on. 2. Provide an orientation to your facility. Treat the student as you would a new employee and let them know what to expect from day one, what you expect from them and what they can expect from you. Times to meet go to lunch, and how long they are expected to stay at your clinic each day. 3. Meet with the student within the first day or so to go over the skills that they have completed in the PTA MACS, and the skills that they can work on with expectation to be checked off as entry level at this clinical rotation site. Set goals and discuss any specific past problem areas noted in the MACS (e.g. NI’s, U’s). 4. Help the student by selecting patients that can help them meet the goals previously set. Update the goals as the student meets them and schedule other patients that may help them address the new goals. 5. Allow the student to review all completed patient evaluations and charts before treatment. Follow up by asking them questions concerning the proposed treatment plan and goals, indications, contraindications and precautions in regards to the upcoming patient treatment. 6. A skill performed by the student should be observed several times before a “” is given. The use of “pretend patients” (e.g., other staff members) can be used to practice skills when appropriate patients are not available. However, skills should be considered as entry level only if they are performed and evaluated on actual patients. St. Philip’s College – PTA Program Clinical Instructors Handbook Page 13 of 20 7. Please remember that students are not employees and should be supervised as such and not “let loose” to treat the patients. Some will require more supervision and feedback than others but all should receive encouragement as well as guidance for improvement. 8. The student and the CI should meet on a regular basis. Choose a time of day that works the best for you to have one on one time. This may not work daily but weekly for some CI’s. That is fine just so the student has access to you for questions that may arise. It is best if the CI has a lighter work load so that they can spend more time with the student. The clinical instructor must provide a formal evaluation at mid-term and at the end of the affiliation. They should be discussed with the student at that time. These forms are in the PTA MACS, pages 1-6 (pink evaluation forms). 9. Please have only one person rating the student in the PTA MACS. Inconsistencies and confusion sometimes arise when multiple clinical instructors rate the same skill. It is appropriate for more than one person to supervise and instruct the student but make it clear to the student who will be rating them in the skills to be completed in the PTA MACS. 10. If a student rates a “NI” in a specific area let them know as soon as possible so that they can have time to correct the deficit seen. Discuss this with the student and guide them to make a plan to be able to pass the skill as entry level, if possible. This may involve more practice, more study/research, or possibly counseling from the ACCE (Mary Hays). 11. The students should be allowed to work with the patients. Once the CI feels that the student can safely work with patients they should be allowed to do so. If the CI feels that the student cannot safely treat patients after remediation the ACCE should be contacted for further direction or removal of the student from the site. 12. If any student related problem arises that cannot be easily resolved please contact the ACCE for assistance. 13. After completion of the evaluation forms the CI may keep a copy but all forms must be returned to the ACCE, usually by giving them to the student to hand carry. These forms are used for grading and are kept in the student’s file. Expectations for a Clinical Instructor Have at least one year of clinical experience as a licensed physical therapist or physical therapist assistant. Demonstrate a desire to work with students Plan a student orientation of the facility Provide the student with the facility policy and procedure information for review Adhere to legal and ethical practice standards Work with the student to develop goals and objectives Plan a variety of learning experiences for the student Provide formal and informal feedback to the student Guide and modify the student learning experiences based on the students performance Become familiar with the PTA MACS Promote the student to evaluate their own clinical experience St. Philip’s College – PTA Program Clinical Instructors Handbook Page 14 of 20 Note areas that need improvement early Discuss problem areas with the CCCE and ACCE Complete the mid-term and final progress reports in the PTA MACS, discuss the completed mid-term report with the ACCE at the mid-term clinical visit Pursue knowledge and skills in clinical teaching (see links below) Assess your ability as a CI and identify areas for further development (see APTA link below) Clinical Education Faculty Development The following are ways in which the CI can further develop his/her skills in clinical instruction: Understand the use of the PTA MACS by one on one instruction with the ACCE (just call or email ACCE), attend regularly scheduled CEU courses offered by St. Philip’s College PTA faculty, or complete the Texas Consortium of Physical Therapy Clinical Education CI CEU course. An explanation of the use of the PTA MACS can be found in the goldenrod pages of the PTA MACS or at the following web site: http://www.alamo.edu/uploadedFiles/St_Philips_College/Library/Files/AlliedHealth-PTAMACSInstruction.pdf Orient yourself to this Clinical Instructor Manual Attend regularly scheduled CEU courses at St. Philip’s College, ask the ACCE about the upcoming course. Topics of the courses presented are ones that have been suggested by previous CI’s, such as Ethics, PTA MACS instruction and Professional behaviors. Better understand teaching and learning, communication and feedback and the Use of the PT and PTA MACS by completing the Texas Consortium for Physical Therapy Clinical Education CI courses. (See link below) Become a Credentialed Clinical Instructor through the APTA; course content and schedules can be found at their web site below. Review the APTA document Guidelines and Self-Assessments for Clinical Education at the web site below. St. Philip’s College – PTA Program Clinical Instructors Handbook Page 15 of 20 SITES of INTEREST for CLINICAL EDUCATION An explanation of the use of the PTA MACS can be found in the goldenrod page of the PTA MACS or at the following web site : http://www.alamo.edu/uploadedFiles/St_Philips_College/Library/Files/AlliedHealth-PTAMACSInstruction.pdf St. Philip’s College PTA Program: http://www.alamo.edu/spc/pta The Texas Physical Therapy Association: www.tpta.org APTA clinical instructor area, Guidelines and Self-Assessments for Clinical Education, access to clinic site information form (CSIF), credentialing courses, etc.: http://www.apta.org/Educators/Clinical The Texas Consortium for Physical Therapy Clinical Education, Incorporated conducts a two part CI certification course. The Basic CI Certification course is online and can be accessed at the link below for $40. When the basic course is successfully completed the CI will earn .4 CEUs. http://texasconsortium.org/ci_cert.htm Medicare guidelines for student supervision: http://www.apta.org/Payment/Medicare/Supervision St. Philip’s College – PTA Program Clinical Instructors Handbook Page 16 of 20 Appendices Appendix A Protocol for Sharp Puncture, Blood or Potentially Infectious Body Fluids Exposure Appendix B Student Clinical Incident/Injury Form - St. Philip’s College Allied Health Department Appendix C Patient Survey Page 17 of 20 Appendix A St. Philip’s College Health Sciences Department Protocol for Sharp Puncture, Blood or Potentially Infectious Body Fluids Exposure It is the policy of St. Philip’s College Allied Health Department that all students who sustain a sharp (needle stick, glass, blade, etc) or other exposure to blood or bodily fluids while engaged in a college sponsored educational program should receive prompt medical attention, including counseling, prophylactic drug treatment, and baseline and follow up laboratory values, as necessary. In accordance with this policy, the following procedures must be followed by students who have been exposed to blood / body fluids. Please keep in mind that drug prophylaxis is time sensitive (2 – 24 hours), and therefore the student must immediately seek help from the appropriate supervising personnel. Immediately after exposure first aid steps should be taken. 1. Squeeze out blood from puncture wound if applicable. 2. Clean wound with soap and water. 3. Flush mucous membranes with water or saline. It is recommended that appropriate medical follow-up be obtained. Some medical facilities will treat, provide accident form, and pay for treatment. If not, students who incurred a sharp puncture or exposure will go to the nearest emergency room for the appropriate consultation and testing. These services will be covered by the Academic Health Care Plan provided through Alamo Colleges. Students should obtain an insurance card at the beginning of each semester. The card is effective for one school year as long as the student is enrolled. They should be instructed to carry the card with them at all times while participating in college sponsored educational programs. Testing of the source patient’s blood will be done according to the facility’s policy. The student is NOT to ask the source patient for permission for blood testing. The student will be counseled and advised regarding post-exposure prophylaxis, if necessary. Baseline blood tests will be administered on the student. Retesting occurs at 6 weeks, 3 months, and 6 months after exposure. All procedures, testing, and results will remain confidential. The clinical instructor should be notified as soon as possible after the incident. The instructor will initiate an incident / injury report and evaluate the circumstances of the incident. If the student declines medical treatment, this should be documented and signed by that individual. Academic Health Care Plan claim forms may be obtained by contacting the campus nurse, or the website at www.ahpcare.com\alamo . For assistance in filing a claim form, please contact the campus nurse. Page 18 of 20 Appendix B STUDENT CLINICAL INCIDENT / INJURY FORM ST. PHILIP’S COLLEGE - ALLIED HEALTH DEPARTMENT DATE OF INCIDENT: _________________ TIME OF INCIDENT: _______________ CLINICAL SITE WHERE INCIDENT OCCURRED: ___________________________ STUDENT NAME: ______________________________________________________ INSTRUCTOR NAME: ___________________________________________________ STUDENT CONTACT INFORMATION: STREET: ____________________________ CITY, STATE, ZIP: __________________________________PHONE: ____________ DESCRIBE WHAT HAPPENED AND NATURE OF ANY INJURY: ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ PLEASE INITIAL ONLY ONE OF THE FOLLOWING: TESTING / TREATMENT WAS DECLINED: __________ TESTING / TREATMENT WAS SOUGHT: ___________ FOLLOW UP DATES: 6 WEEKS ____________ 3 MONTHS __________ 6 MONTHS __________ Student Signature: _____________________________ Date: ____________________ Instructor Signature: ____________________________ Date: ____________________ Page 19 of 20 Appendix C St. Philip’s College Patient Survey of the Student Physical Therapist Assistant Please answer the following questions about the student physical therapist assistant who has worked with you. Circle the number that applies most closely to how you feel about the student. This survey is confidential. When the physical therapist assistant student treated you: 1. The student was polite and courteous? Comments? Agree 5 4 Disagree 3 2 1 _________________ 2. The student seemed to know what he/she was doing? Agree 5 4 Disagree 3 2 1 _________________ 3. The student seemed caring and compassionate? Agree 5 4 After filling this out: Disagree 3 2 1 _________________ 1. Put survey in the envelope provided 2. Seal the envelope 3. Give to the student to return it to school Questions? Call Mary Hays, St. Philip’s College PTA Program, and 210 - 4862459 Page 20 of 20