SKIN INTEGRITY AND WOUND CARE
advertisement

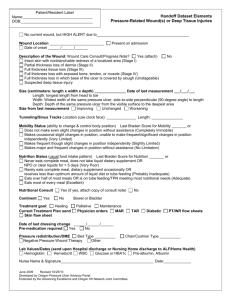
SKIN INTEGRITY AND WOUND CARE SKIN AND SKIN BREAKDOWN WOUND CLASSIFICATION: AN INTENTIONAL WOUND UNINTENTIONAL WOUNDS AN OPEN WOUND AN CLOSED WOUND PHASES OF WOUND HEALING INFLAMATORY PHASE FIBROPLASIA (Proliferation )phase Maturation (remolding) phase WOUND HEALING PROCESSES PRIMARY HEALING SECONDARY HEALING TERTIARY HEALING FACTORS AFFECTING WOUND HEALING AGE CIRCULATION & OXYGENATION WOUND CONDITION OVERALL PATIENT HEALTH WOUND COMPLICATIONS INFECTION: Purulent Drainage Increased Drainage Pain Redness Swelling Increased Body Temperature Increased White Blood Cell Count (WBC) DEHISCENCE OR EVISCERATION DEFINE EACH: Patients at greatest risk for these complications Include: Obese or malnourished Have infected wounds Excessive coughing Vomiting or straining HEMMORHAGE Occurrences may be due to: Slipped sutures A dislodged clot from stress at the suture line or operative site Infection Erosion of a blood vessel by a foreign body such as a drain PSYCHOLOGICAL EFFECTS OF WOUNDS PAIN ANXIETY AND FEAR ALTERATION IN BODY IMAGE ASSESSING THE WOUND Inspection Sight Smell Palpation Appearance Drainage Pain DIAGNOSING IN WOUND CARE Altered skin integrity Risk for infection Pain Delayed surgical recovery Body image disturbance PLANNING EXPECTED OUTCOMES FOR WOUND CARE Facilitating the patients return to health Providing interventions that facilitate wound healing Reduce the risk for complications Promote psychosocial adaptation IMPLEMENTING WOUND CARE Promote wound healing Prevent further injury Prevent alterations in skin integrity Prevent infections Promote physical and emotional comfort Facilitate coping TEACHING FOR HOME CARE OF A WOUND Explain the terminology Identify risk factors Explain where and how pressure ulcers develop Describe various prevention strategies and options EVALUATING WOUND CARE Evaluating is based on the expected outcome (EO) No complications Wound is progressing through the healing stages PRESSURE ULCERS: PATHOLOGY OF ULCER DEVELOPMENT: External Pressure Friction Shearing Forces FACTORS AFFECTING PRESSURE ULCER DEVELOPING Mobility Immobility Nutrition Hydration Moisture on the skin Mental status Age PRESSURE ULCER STAGING Stage I Stage II Stage III Stage IV ASSESSING THE RISK FOR:PRESSURE ULCERS Nursing history Physical assessment pg.933 Mobility Nutrition Incontinence Use of Braden scale pg.936 ASSESSING: “ACTUAL” PRESSURE ULCER 1st sign of pressure =“blanching” (local anemia, is called “ischemia”) Ischemia is rapid followed by hyperemia when pressure is relieved. DIAGNOSING PRESSURE ULCERS Impaired Skin Integrity* The stage of the ulcer is a factor in determining the nursing diagnosis Stage I and II pressure = superficial skin damage. Stage III and IV pressure ulcer = full thickness skin loss and damage to underlying tissue Impaired Tissue Integrity is more appropriate* PLANNING EXPECTED OUTCOMES FOR PRESSURE ULCERS Patient participation Demonstrate progression in healing of the ulcer Demonstrate increase in body wt. and muscle size Remain free of infection at the wound site Develop no new areas of skin breakdown Demonstrate self-care measures necessary to prevent development of a pressure ulcer IMPLEMENTING INTERVENTIONS TO PREVENT PRESSURE ULCERS: Protecting the skin from external mechanical forces Teach patient and caregivers about prevention Pressure ulcer care Cleaning the pressure ulcer Dressing the pressure ulcer Controlling infection Providing care when surgical intervention is necessary Evaluate Pressure Ulcer Care Had the patient and caregiver participated effectively in prevention and treatment Prevention of additional skin breakdown Demonstrated progressive healing of pressure ulcer Remained free of infection Improved overall physical condition