Chapter 48: Skin Integrity and Wound Care
advertisement

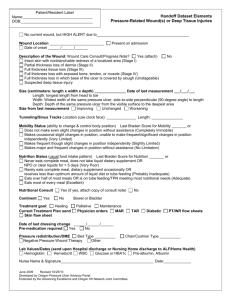
Chapter 47: Mobility and Immobility Bonnie M. Wivell, MS, RN, CNS The Nature of Movement Coordination between the musculoskeletal system and the nervous system. Alignment and Balance – The positioning of the joints, tendons, ligaments and muscles while standing, sitting, and lying Gravity and Friction – Gravity is the force of weight downward – Friction is force that opposes movement Physiology and Regulation of Movement Long bones contribute to height Short bones occur in clusters Flat bones provide structural contour Irregular bones make up the vertebral column and some bones of the skull Functions of MSK – Protects vital organs – Aids in calcium regulation – Production and storage of blood Joints Synostotic = bones joined by bones; no movement; example: skull Cartilaginous = cartilage unites bony components; allows for growth while providing stability; example: 1st sternocostal joint Fibrous = ligament or membrane unites two bony surfaces; limited movement; Example: tib/fib Synovial = A true joint; freely movable; – Pivotal – Ball and socket – Hinge Ligaments/Tendons/Cartilage Ligaments = white, shin, flexible bands of fibrous tissue binding joints together and connecting bones and cartilages Tendons = white, glistening, fibrous bands of tissue that connect muscle to bone; strong, flexible Cartilage = nonvascular, supporting connective tissue Skeletal Muscle Ability of muscles to contract and relax are the working elements of movement Muscles are made of fibers that contract when stimulated by an electrochemical impulse that travels from the nerve to the muscle Muscles associated with posture converge at a common tendon – Lower extremities, Trunk, Neck, Back Coordination and regulation of different muscle groups depend on muscle tone (normal state of balanced muscle tension) Muscle tone helps maintain functional positions such as sitting or standing The Nervous System The motor strip is the major voluntary motor area and is located in the cerebral cortex A majority of motor fibers descend from the motor strip and cross at the level of the medulla Motor fibers from right motor strip control voluntary movement on left side of body and motor fibers on left control movement on right side of body Impulses descend from motor strip to spinal cord Impulse exits the spinal cord through efferent motor nerves and travels through the nerves The Nervous System Cont’d. Neurotransmitters or chemicals transfer electric impulses from the nerve to the muscle Neurotransmitters stimulate the muscles causing movement Movement is impaired by disorders that alter – Neurotransmitter production – Transfer of impulses from the nerve to the muscle – Activation of muscle activity Pathological Influences on Mobility Postural abnormalities: congenital or acquired postural abnormalities affect the efficiency of the MSK system as well as body alignment, balance, and appearance – Can cause pain, impair alignment or mobility Impaired muscle development: patients with muscular dystrophy experience progressive, symmetrical weakness and wasting of skeletal muscle groups, with increasing disability and deformity Pathological Influences on Mobility Damage to the Central Nervous System: damage to any component of the CNS that regulates voluntary movement results in impaired body alignment, balance, and mobility – Complete transection of the spinal cord results in a bilateral loss of voluntary motor control below the level of trauma – Damage to the cerebellum causes problems with balance and motor impairment is directly related to amount and location of destruction Trauma to the Musculoskeletal System: direct trauma results in bruises, contusions, sprains, and fractures Mobility and Immobility Mobility refers to a person’s ability to move about freely and immobility refers to the inability to do so The effects of muscular deconditioning associated with lack of physical activity are often apparent in a matter of days Disuse atrophy describes the tendency of cells and tissue to reduce in size and function in response to prolonged inactivity resulting from bed rest, trauma, casting, or local nerve damage The Effects of Immobility Metabolic changes – Negative nitrogen balance – Calcium resorption (loss) GI changes – Constipation → Impaction → Mechanical Obstruction Respiratory changes – Atelectasis → Pneumonia Cardiovascular changes – Orthostatic hypotension – Increased cardiac workload – Thrombus formation (Virchow’s triad) The Effects of Immobility Cont’d. Musculoskeletal changes – ↑ protein breakdown → ↓ lean body mass – Osteoporosis – Joint contractures Foot drop Changes in urinary elimination – Urinary stasis – Renal calculi Integumentary changes – Pressure ulcers Older Adults Immobility can lead to…. – Loss of mobility and functional decline – Weakness, fatigue, and increased risk for falls – Shallow breathing resulting in pneumonia – Inadequate turning/repositioning results in skin breakdown and pressure ulcers – Anorexia and insufficient assistance with eating leads to malnutrition – Multiple interruptions and noise impair sleep, causing fatigue, depression, and confusion. Mobility ROM = amount of movement at a joint – Active/Passive – See pages 1232 – 1236 Gait = style of walking Exercise and activity tolerance: age and illness can affect this Body Alignment – Standing/Sitting/Lying Patients with impaired mobility, decreased sensation, impaired circulation, and lack of voluntary muscle control are at risk for damage to the MSK system when lying down Range of Motion Safe Patient Handling Protecting the Patient and Health Care worker – Manually lifting and transferring clients contributes to the high incidence of workrelated MSK problems and back injury – Lift teams/lift equipment – Ergonomics training Plan ahead based on patient assessment Assistive Devices for Patient Movement All devices must be appropriate for patient – Weight limit – Reason for Device – Measured to patient Canes Walkers Wheel chairs Crutches Gait Belt Wearing a Gait Belt Using a Gait Belt Ambulating With a Walker Assessment Metabolic – – – – I&O Lab values Height and weight Nutritional intake – Breakdown – Color changes Respiratory CV – Pulses/Cap refill – Edema/DVT MSK – Muscle tone/strength – Contractures Elimination – I&O – Bowel sounds – Frequency and consistency of stool – Dietary intake – Auscultate lungs Integument Psychosocial – Anxiety – Depression – Sleep deprivation Plan Goals and outcomes individualized Set priorities Collaborative care: team approach Interventions Health promotion – Education – Prevention – Early detection Prevention of work-related MSK injuries – Use of ergonomics Exercise Bone health – Screening – Maintain independence with ADLs – Assistive ambulatory devices Interventions Cont’d. Metabolic – – – – – High-protein, high-calorie diet Vitamin B for skin integrity and wound healing Vitamin C for replacing protein stores TPN Enteral feedings Respiratory – Turn, cough, and deep breathe (TCDB) – Chest physiotherapy (CPT) – 2000 mL of fluid daily if not contraindicated Interventions Cont’d. CV – Mobilize ASAP, dangle or sit in chair at minimum – Isometric Exercise – Discourage use of valsalva maneuver – DVT prophylaxis TEDS – apply properly, remove at least bid Avoid crossing legs, sitting for prolonged periods of time, wearing constrictive clothing, putting pillows under the knees, and massaging legs Meds Interventions Cont’d. MSK – ROM – CPM in orthopedics Integument – Screen for risk (Braden Scale) – Prevention – Position changes Interventions Cont’d. Elimination – – – – – Adequate hydration If incontinent, provide frequent skin care Catheterize prn Foods high in fiber Stool softners/cathartics prn Psychosocial – – – – Schedule care to prevent interruption of sleep Depression screening (GDS) Provide stimulation and re-orient prn Involve clients in own care as much as possible Positioning Semi Fowler’s Position Sim’s or Left Lateral Position Now let’s write a nursing care plan regarding immobility Chapter 48: Skin Integrity and Wound Care Skin Two layers – Epidermis = has several layers Stratum corneum = thin, outermost layer – Allows for evaporation of water from skin – Permits absorption of topical meds Basal layer – Dermis = provides strength, support and protection of underlying muscles, bones, and organs Pressure Ulcers Impaired skin integrity (damage to the skin) related to unrelieved, prolonged pressure and/or shearing/friction AKA: Pressure sore, decubitus ulcer, bedsore Localized injury to the skin or other underlying tissue, usually over a body prominence Pathogenesis Pressure Intensity – Tissue ischemia can occur due to capillary occlusion for a prolonged period of time – Patient’s with decreased sensation cannot respond to discomfort associated with ischemia hence tissue death results – Blanching = occurs when normal red tones of the light skinned client is absent (doesn’t occur in darkly pigmented skin) Pathogenesis Cont’d. Pressure Duration – Low pressure over a prolonged time period – High-intensity pressure over shot period Tissue Tolerance – Depends on integrity of the tissue and the supporting structures – Shear, friction and moisture make skin more susceptible to damage from pressure – Ability of underlying skin structures to assist with redistribution of pressure Affected by poor nutrition, increased aging, and low BP Risk Factors Impaired sensory perception Impaired mobility Alteration in LOC Shear Friction Moisture Classification of Pressure Ulcers Stage I: Intact skin with non-blanchable redness of a localized area Stage II: Partial-thickness skin loss involving epidermis, dermis or both; superficial abrasion, blister, or shallow crater Stage III: Full-thickness tissue loss; subcutaneous fat may be visible, slough may be present; may include undermining and tunneling Stage IV: Full-thickness tissue loss with exposed bone, tendon, or muscle; slough or eschar may be present on some parts; often includes undermining and tunneling Unstageable if bed is full of slough or eschar STAGE I ULCER- GREATER TROCHANTER STAGE II ULCER – ISCHEAL TUBEROSITY STAGE III STAGE IV ISCHEAL TUBEROSITY AND SACRUM Definitions Granulation tissue = red moist tissue composed of new blood vessels; indicates healing Slough = stringy substance attached to wound bed; needs removed before wound can heal Eschar = black or brown necrotic tissue; must be removed before wound can heal Exudate = Type (consistency), Amount, Color, and Odor of wound drainage; part of your assessment Process of Wound Healing Primary intention = edges are well approximated or closed; risk of infection low; heals quickly; minimal scar formation – Example: surgical wound Secondary intention = wound is left open until becomes filled with scar tissue; chance of infection is great; longer healing time – Example: burn, pressure ulcer, severe laceration Complications of Wound Healing Hemorrhage/hematoma Infection – Second most common health care associated infection Dehiscence = partial or total separation of wound layers Evisceration = protrusion of visceral organs through wound opening Fistulas = abnormal passage between two organs or between organs and the outside of the body Prediction and Prevention of Pressure Ulcers Risk Assessment – Braden Scale (see slide in chapter 47) – Prevention Factors influencing pressure ulcer formation and wound healing – – – – – Nutrition Tissue perfusion Infection Age Psychosocial impact (true impact unknown) Assessment Assess skin for signs of ulcer development Pressure ulcer assessment – Risk assessment – Mobility – Nutritional status – Body fluids – Pain Wound Assessment Type: abrasion, laceration, puncture, etc. Appearance: red, inflamed, clean, dirty Drainage: TACO Drains Closures Palpation Cultures Interventions Prevention Frequent skin assessment Keep skin clean and dry Don’t use soaps and hot water Apply moisturizers Control/contain incontinence, perspiration or wound drainage Positioning Therapeutic bed/mattress Wound Management Clean wounds with noncytotoxic wound cleansers – Normal saline – Commercial wound cleansers Cytotoxic cleansers used for chemical debridement – – – – Dakin’s solution (sodium hypochlorite soln) Acetic acid Providone-iodine Hydrogen Peroxide Debridement Removal of nonviable, necrotic tissue Mechanical – Wet-to-dry saline gauze dressing – Wound irrigation Autolytic – Uses synthetic dressings that allow the eschar to be self-digested by enzymes in wound fluids Chemical – Topical enzyme preparations (Dakin’s, sterile maggots) Surgical – Removal of devitalized tissue b use of scalpel, scissors or other sharp instrument Wound Management Cont’d. Topical growth factors regulate healing of chronic wounds Education of client and caregivers is important Nutritional status Protein status = necessary for healing; rebuilds epidermal tissue Hemoglobin = decreases delivery of O2 to tissues leading to further ischemia Dressings Dry or moist – Gauze Hydrocolloid – Protects the wound from surface contamination Hydrogel – Maintains a moist surface to support healing Wound V.A.C. – Uses negative pressure to support healing 74 Types of Dressings Brands vary by institution Follow recommendations of wound care nurse See page 1313 of text Wound VAC (vacuum assisted closure) – Negative pressure – See pages 1321-1323 Other Wound Devices Drains – Hemovac – Jackson-Pratt Closures – Staples – Sutures Binders Montgomery straps Slings Sitz baths Heat and Cold Therapy Assessment for temperature tolerance Bodily responses to heat and cold Factors influencing heat and cold tolerance Education http://www.youtube.com/watch?v=Hx26HCML3 W8 77 Nursing Diagnosis Impaired Skin Integrity r/t immobility as evidenced by stage III decubitus ulcer on coccyx Plan (stage I ulcer) On-going skin assessment Nutritional assessment Pressure relief for affected areas Preventative care for intact skin Goals Pt. will not have increase in size of pressure ulcer during hospitalization Pt. will not develop infection in pressure ulcer during hospitalization Pt. will have nutritional needs identified by dietitian Patient and family will develop a plan (with assistance of nursing) for preventing further skin breakdown Interventions RN to assess skin q shift Dietician to complete nutritional assessment and recommend a diet within 24 hours Assistive personnel to reposition patient q 2 hours using the following schedule – 8am supine – 10 am left side – 12 noon prone – 2pm right side………. Rationale Decreasing the duration of pressure on skin will prevent further skin breakdown. (Perry and Potter, p. 1281) Wound healing requires proper nutrition. (Perry and Potter, p. 1290) Family caregivers require education and counseling for interventions to be effective. (Perry and Potter, p. 1310) Outcome Evaluation By discharge date, patient had developed stage I ulcer – Evaluate and update plan for ulcer prevention Patient has gained 3lbs by discharge and serum proteins have increased Family has decided on transfer to LTC for further patient care