Becker Sarah Becker KNH 411 2015 November 18 Diabetes Case
advertisement

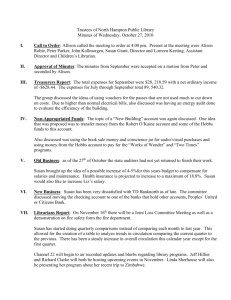
Becker 1 Sarah Becker KNH 411 2015 November 18 Diabetes Case Study 1. Define insulin. Describes its major functions within normal metabolism. a. Insulin is a hormone produced by the beta cells of the islets of Langerhans in the pancreas to regulate blood glucose; it promotes uptake, utilization, and storage of nutrients (470). It controls the metabolic fate of carbohydrates, proteins, and lipids. It transports glucose from the bloodstream into cells to be used as energy. Insulin also promotes active transport of proteins from the blood into muscle, promoting protein synthesis within cells, causing a positive nitrogen balance (477). 2. What are the current opinions regarding the etiology of type 1 diabetes mellitus (DM)? a. T1DM is a result of a cell-mediated autoimmune response causing a gradual decline in beta-cell mass within genetically susceptible individuals. T1DM is genetic, as the primary gene is located in the HLA region on chromosome 6. Polymorphisms of this region account for roughly 50% of the genetic risk of getting T1DM. Other potential causes of T1DM include environmental agents, such as viruses and gluten, or infant feeding practices, including length of breastfeeding and exposure to cow’s milk proteins. 3. What genes have been identified that indicate susceptibility to type 1 diabetes mellitus? a. On chromosome 6, the HLA region has been identified as the primary risk factor for T1DM. A polymorphism in this region accounts for approximately 50% of the genetic risk of getting T1DM. 20 other different gene associations have also been linked to risk for this disease. Even though the genetic component of T1DM Becker 2 supports the increased risk of relatives of individuals with T1DM, the risk is still low. It is 3-4% if the parent has DM, or 5-15% if a sibling has it (481). 4. After examining Susan’s medical history, can you identify any risk factors for type 1 DM? a. In her medical history, it is indicated that her maternal grandmother had Diabetes. Having a relative with diabetes increases the risk of having diabetes as well (481). Furthermore, Susan indicated upon admit that she had polydipsia, polyuria, polyphagia, weight loss, and fatigue. These are all classic symptoms of T1DM (481). 5. What are the established diagnostic criteria for type 1 DM? How can physicians distinguish between type 1 and type 2 DM? a. The established diagnostic criteria for diabetes is fasting plasma glucose ≥ 126 mg/dl or casual plasma glucose ≥ 200 mg/dl, along with classic symptoms of unexplained weight loss, polydipsia, polyuria, and polyphagia. T1DM can be determined through lack of beta cells and production of insulin (486). People with T2DM produce insulin, but their tissues are insulin resistant. Thus, those with T2DM display insulin resistance and relative insulin deficiency. While T1DM is genetic, T2DM is polygenic and mostly caused by environmental factors such as obesity, poor nutrition, and physical inactivity (484). 6. Describe the metabolic events that led to Susan’s symptoms (polyuria, polydipsia, polyphagia, weight loss, and fatigue) and integrate these with the pathophysiology of the disease. Becker 3 a. T1DM is caused by the deficiency of insulin due to the destruction of pancreatic B cells, resulting in the inability of cells to use glucose for energy. Because glucose can’t enter the cells, plasma glucose levels rise (hyperglycemia), and the cells starve. In order to compensate for hyperglycemia, excess glucose is lost in the urine. This causes polyuria, which brings forth fluid loss, stimulating the thirst mechanism and leading to polydipsia. Since cells are dependent on glucose for energy and can’t get it, the body promotes hunger, causing polyphagia (481). 7. List the microvascular and neurologic complications associated with type 1 diabetes. a. Microvascular and neurologic complications include retinopathy and neuropathy, which can be peripheral or autonomic. Risk factors primarily involve the duration of DM, as well as hyperglycemia, poor glucose control, and hypertension (489490). 8. When Susan’s blood glucose level is tested at 2 AM, she is hypoglycemic. In addition, her plasma ketones are elevated. When she is tested early in the morning before breakfast, she is hyperglycemic. Describe the dawn phenomenon. Is Susan likely to be experiencing this? How might this be prevented? a. The dawn phenomenon is a common complication in DM patients, caused by the overnight release of hormones, insufficient insulin at night, as well as excessive food at bedtime. Susan is likely to be experiencing this, because a key symptom is unexplained fasting hyperglycemia in the morning. The dawn phenomenon can be prevented by adjusting insulin dosages and bedtime snacks. This varies per patient, so treatment will be trial and error (488). Becker 4 9. What precipitating factors may lead to the complication of diabetic ketoacidosis? List these factors and describe the metabolic events that result in the signs and symptoms associated with DKA. a. Diabetic ketoacidosis is often caused by lack of blood glucose monitoring, severe illness or infection, not using insulin, or increased insulin needs due to growth spurts (488). Metabolically, it is caused by persistent insulin deficiency which causes additional hormones to be created. This leads to lipolysis, allowing the body to break down fat stored in adipose tissue, transforming the resulting fatty acids into keto acids by the liver. These excess keto acids cause pH to fall, and ketone bodies appearing in the urine. Metabolic acidosis develops as bicarbonate concentration is reduced, resulting in ketoacidosis. Kussmaul respirations (heavy, labored breathing) commonly occurs as the body tries to get rid of the ketones. As total body water decreases, potassium, sodium, magnesium, and phosphorus are also lost. This can cause nausea and vomiting (481). 10. Determine Susan’s stature-for-age and weight-for-age percentiles. a. Using a pediatric growth chart, Susan is in the 50% percentile for stature and is in the 10% percentile for weight. 11. Interpret these values using the appropriate growth chart. a. For pediatric patients, anything under 5% percentile is concerning and called ‘underweight’. Having percentiles between 5-85% percentiles are normal. Thus, Susan is in the normal range for her weight and height. However, her weight is low and could become concerning should she continue to lose weight with her untreated T1DM (53). Becker 5 12. Estimate Susan’s daily energy and protein needs. Be sure to consider Susan’s age. a. Schofield (female: A 10-18): 8.365W + 4.65H +200 i. W (kg) = 100/2.2 = 45.46 kg ii. H (cm) = 62*2.54 = 157.48 cm iii. 8.365(45.46) + 4.65(157.48) + 200 =1312.55 b. Pro: 0.85g *kg i. 0.85*45.46kg = 38.64 g/day ii. 15-35% kcal: 81-184g 1. 2100*.15=315kcal/4 = 81g 2. 2100*.35=735kcal/4 = 184g c. Mifflin: 10(wt) +6.25(ht) – 5*age -161 i. 10(45.56) + 6.25 (157.48) -5*15 – 161 = 1203.85 * 1.8 (PAL) = 2167kcal (2100-2200kcal) d. Susan needs between 2100-2200kcal daily using the Mifflin equation, as the Schofield Pediatric equation was not accurate for her needs. I used a PAL of 1.8, since she plays vigorous volleyball 6x a week as well. For protein, a DRI chart in the back of Nelms recommends 46g of protein for Susan per day, or 0.85g/kg (back cover DRI). Using the RDA of 15-35%, Susan requires 81-184g per day. Thus, Susan needs between 38-184 grams of protein per day. I would follow the current diet order of 55-65 grams of protein due to her being an athlete. This is the middle of the ranges I created. 13. What would the clinician monitor in order to determine where or not the prescribed energy level is accurate? Becker 6 a. The clinician would have to monitor if there was continued weight loss, fatigue, or muscle wasting to ensure that the prescribed energy level is accurate. Furthermore, asking Susan if she feels hungry or full at different times is another way to determine this. 14. Using a computer dietary analysis program or food composition table, calculate the kcalories, protein, fat (saturated, polyunsaturated, and monosaturated), CHO, fiber, and cholesterol content of Susan’s typical diet. a. Using Supertracker, Susan consumed 3847kcal during her dietary recall. She consumed 122g of protein (13%), 529g CHO (55%), and 34% of her calories came from fat. 12% of the fat consumed contained saturated fat; 7% was polyunsaturated; and 11% was monounsaturated. Susan consumed 30g of fiber, which is above the recommended. She also received 256mg of cholesterol, which is within the normal range as well. She ate over the recommended amount of protein, but that’s not generally not concerning. However, she did significantly overconsume calories, and could stand to cut back on saturated fats (Foodtracker). 15. What dietary assessment tools can Susan use to coordinate her eating patterns with her insulin and physical activity? a. Susan can work on having set meal times during the day, and she can create a Supertracker account to record her physical activity and diet intake. With a comprehensive nutrition assessment, a self-care treatment plan, her health status, learning ability, readiness for change, and current lifestyle, Susan can control her T1DM (495). Becker 7 16. Dietitians must obtain and use information from all components of a nutrition assessment to develop appropriate interventions and goals that are achievable for the patient. This assessment is ongoing and continuously modified and updated throughout the nutrition therapy process. For each of the following components of an initial nutrition assessment, list at least three assessments you would perform for each component: Component Assessments You Would Perform Clinical data Previous medical conditions or surgeries; medication; determine socioeconomic status/food security, support systems, and education; energy needs Nutrition history Ability to chew; problems swallowing; nausea, vomiting, constipation, diarrhea or heartburn; any other symptoms interfering with ability to ingest a normal diet; ability to feed self; food allergies Weight history Height; current weight; highest adult weight; usual body weight; reference weight (BMI) Physical activity history Estimate energy expenditure; determine type and frequency of PA Monitoring Determine self-monitored outcomes; laboratory tests; further education; adjust dosages Psychosocial/economic Determine income level; confidence levels in school; food security Knowledge and skills level Primary language; grade in school; ability to prick self using needles Expectations and readiness to change Talk to patient to determine; reassess to see how that’s going Becker 8 17. Does Susan have any laboratory results that support her diagnosis? a. Susan has several lab values that support her diagnosis of T1DM, including her osmolality, glucose, BUN, and HbA1C. Her blood glucose was 250mg/dl when she was admitted, making her hyperglycemic. A high osmolality indicates the presence of water-attracting particles (glucose) within her internal fluids (G-16). A high BUN is indicative of poor kidney function usually; though in this case it is probably elevated due to dehydration (553). Furthermore, a key value is HbA1C. This measure the amount of glucose to hemoglobin protein. The higher the glucose concentration in the blood, the more hemoglobin is glycated, thus testing hyperglycemia. As it has a half-life of three months, it can show unregulated glucose monitoring as well (487). 18. Why did Dr. Green order a lipid profile? a. Dr. Green ordered a lipid profile to double-check the diagnosis of T1DM versus T2DM. Type 1 diabetic patients have similar lipid profiles to non-diabetic patients, as is seen in Susan’s profile. However, people with T2DM tend to have high levels of triglycerides and low HDLs. LDL particles also are prone to do more damage in patients with T2DM (“Lipid Profile”). 19. Evaluate Susan’s laboratory values: Chemistry Prealbumin (59) Normal Susan’s Reason for Nutritional Value value abnormality implications 16-35 40 Malnutrition Dehydration; and can be fixed dehydration quickly with insulin to help glucose intake Becker 9 Osmolality (G-16) 285-295 304 Presence of glucose in fluids Glucose (487) 70-110 250 Insufficient insulin BUN (553) 8-18 20 Poor kidney function HbA1C (487) 3.9-5.2 7.95 Excess glucose attached to hemoglobin 20. Compare the pharmacological differences in insulins: (page 491) Type of Insulin Lispro Aspart Glulisine NPH Brand Name Onset of Action Peak of Action (hours) 30-90 30-90 30-90 4-10 Too much water in body; may cause electrolyte imbalances Inadequate nutrition for cells Dehydration Hyperglycemia; insufficient glucose regulation Duration of Action (hours) 3-5 3-5 3-5 10-18 Humalog 5-15 min Novolog 5-15 min Apidra 5-15 min Humulin R, 2-4 hours ReliOn Glargine Lantus 2-4 hours Peakless 20-24 detemir Levemir 1-3 hours 6-8 18-22 70/30 premix Humulin 70/30, 30-60 min Dual 10-16 Novolin 70/30 50/50 premix Humulin 50/50 30-60 min Varies 10-16 60/40 premix Humulin 60/40 30-60 min 2-4 hours 24 21. Once Susan’s blood glucose levels were under control, Dr. Green prescribed the following insulin regimen: 24 units of glargine in PM with the other 24 units as lispro divided between meals and snacks. How did Dr. Green arrive at this dosage? a. Glargine is used at night, and so can’t be mixed with other insulins. 24 units should keep her steady throughout the night, so that she won’t have to add more insulin. Glargine is good for this, because it is peakless and should prevent any Becker 10 hypo- or hyperglycemia. Lispro is fast-acting and has a peak, but it can be used multiple times throughout the day. This will allow Susan to change her dosages depending on her activity and food she eats throughout the day (491). 22. Identify at least three specific potential nutrition problems within this domain that will need to be addressed for Susan and her family. a. A potential nutrition problem is lack of education. Susan needs to be educated on what foods contain lots of carbohydrates, and she needs to learn how to carb count to prevent hyperglycemia. She needs to know how to take insulin regularly to prevent hypo-/hyperglycemia. She and her family will also need education on cooking for diabetic patients, as Susan will need to learn how to eat as a diabetic patient. 23. Just before Susan is discharged, her mother asks you, “My friend who owns a health food store told me that Susan should use stevia instead of artificial sweeteners or sugar. What do you think?” What will you tell Susan and her mother? a. For Susan, there is no real difference regarding taking stevia or using real sugar. They both affect blood glucose levels about the same, and so she can treat them the same. Saying that, she should try to limit her intake of added sugars and consume natural sugars instead (Barriocanal). 24. Select two high-priority nutrition problems and complete the PES statement for each. a. Inadequate food and nutrition knowledge (FH-4.1) as related to hyperglycemia as evidenced by onset of Type 1 Diabetes. b. Excessive energy intake (NI-1.3) as related to polyphagia, as evidenced by consumption of 3800kcal in dietary recall and diagnosis of Type 1 Diabetes. Becker 11 25. For each of the PES statements that you have written, establish an ideal goal (based on the signs and symptoms) and an appropriate intervention (based on the etiology). a. Inadequate food and nutrition knowledge: An ideal goal for Susan is to no longer be hyperglycemic and to prevent this from occurring as often as possible. Interventions include nutrition education programs to educate Susan on her insulin needs, since she now knows what is going on with her body. b. Excessive energy intake: Susan only needs about 2400kcal per day with her activity level. She is way over, likely due to polyphagia and inadequate amounts of glucose entering her cells. Ideally, once Susan begins tracking her calories, she will begin eating a normal diet at 2400kcal. She can track using Supertracker and since she now has insulin, she most likely will not be as hungry. 26. Does the current diet order meet Susan’s overall nutritional needs? If yes, explain why it is appropriate. If no, what would you recommend? Justify your answer. a. The current order does meet Susan’s nutritional needs. The order is for 2400kcal and she needs about 2200. I would lower it to 2200 unless she expresses that she is hungry. This is appropriate for her activity and growth level. Her protein level is also appropriate for a young athlete. 55g is between the two levels I calculated, and I believe the middle level is best, since she needs protein to maintain and grow muscle. 27. Susan is discharged Friday morning. She and her family have received information on insulin administration, SMBG, urine ketones, recordkeeping, exercise, signs, symptoms, and Tx of hypo-/hyperglycemia, meal planning (CHO counting), and contraception. Susan and her parents verbalize understanding of the instructions and have no further Becker 12 questions at this time. They are instructed to return in two weeks for appointments with the outpatient dietician and CDE. When you come in to work Monday morning, you see that Susan was admitted through the ER Saturday night with a BG of 50mg/dL. You see her when you make rounds and review her chart. During an interview, Susan tells you she was invited to a party Saturday night after her discharge on Friday. She tested her blood glucose before going to the party, and it measured 95mg/dl. She took 2 units of insulin and knew she needed to have a snack that contained approximately 15g CHO, so she drank one beer when she arrived at the party. She remembers getting lightheaded and then woke up in the ER. What happened to Susan physiologically? a. Susan went to the party with normal blood sugar, but with two units of insulin. Consuming one beer was not an adequate snack, since it only accounted for one unit, and alcohol inhibits gluconeogenesis. This can then provoke hypoglycemia. When she became hypoglycemic, she became light-headed. Since her body was intoxicated, having digested the beer quickly, Susan didn’t recognize the symptoms and passed out (van de Wiel). 28. What kind of educational information will you give her before this discharge? Keep in mind that she is underage for legal consumption of alcohol. a. I will remind her about CHO counting and insulin dosages, especially since insulin can react with alcohol, and the two should be taken together with caution. I will also give her information on how alcohol affects the body and explain that it is illegal for her to be consuming it. I will tell her what happened, and explain how the beer caused her to pass out. Alcohol consumption may cause delayed hypoglycemia. Plus, alcohol kilocalories should be considered an addition to Becker 13 regular food or meals, and alcohol should not be substituted for food (497). A key piece of information is that if she is going to drink, she needs to be cautious and always take alcohol with food, or else she may become hypoglycemic again (van de Wiel). Becker 14 Resources Barriocanal, L. (2008, June 5). Apparent lack of pharmacological effect of steviol glycosides used as sweeteners in humans. A pilot study of repeated exposures in some normotensive and hypotensive individuals and in Type 1 and Type 2 diabetics. Retrieved November 16, 2015, from http://www.ncbi.nlm.nih.gov/pubmed/18397817 Foodtracker. (2015). Retrieved November 17, 2015 from https://supertracker.usda.gov/foodtracker.aspx Lipid Profile. (2013, March 26). Retrieved November 17, 2015, from http://www.diabetesselfmanagement.com/diabetes-resources/definitions/lipid-profile/ Van de Wiel, A. (2004, July 20). Diabetes mellitus and alcohol. Retrieved November 19, 2015, from http://www.ncbi.nlm.nih.gov/pubmed/15250029