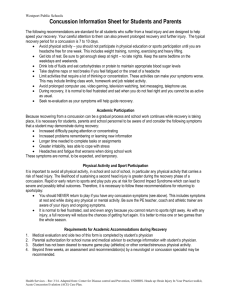
What is Concussion?
advertisement

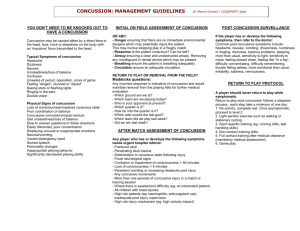
Advancements in the Treatment and Management of Concussions to Improve Patient Outcomes William R. Wellborn III, PhD Director Carilion Sports Concussion Program Department of Physical Medicine and Rehabilitation Carilion Clinic wrwellborn@carilionclinic.org Objectives • Explain Definition of Concussion – Signs & Symptoms • Integral Parts of Initial Evaluation – History, Self Report Symptoms & Neurocognitive Evaluation & Vestibular/Visual Ocular Examinations • Discuss Management & Treatment – Multidisciplinary 1. Specific Clinical Trajectories (Pathways) 2. Referral to Specialists •Recent advancements in treatment Disclosure I have affirmed to have no relevant financial relationship with any of the products, manufacturers, or providers of services that may be discussed in this presentation. Why is sport concussion such an important topic? • National Football League: – Media- TV, Newspapers, Internet, Social Media • State Laws: – Washington 2009 – Virginia 2010/2011 – Now all 50 States and Washington DC Lystedt’s Law • State of Washington – Zach Lystedt was returned to play by his coach after 2 injuries in one game – Second injury produced malignant brain swelling and permanent brain damage • Resulted in law requiring evaluation prior to return to play (2009) Virginia Law 2010/2011 • • 1. No member of a school athletic team shall participate in any athletic event or practice the same day he or she is injured and: – a. exhibits signs, symptoms or behaviors attributable to a concussion; or – b. has been diagnosed with a concussion. 2. No member of a school athletic team shall return to participate in an athletic event or training on the days after he/she experiences a concussion unless all of the following conditions have been met: – a. the student no longer exhibits signs, symptoms or behaviors consistent with a concussion, at rest or with exertion; – b. the student is asymptomatic during, or following periods of supervised exercise that is gradually intensifying; and – c. the student receives a written medical release from a licensed health care provider. The Zurich Consensus Statement (November 2008) return to play guidelines and the American Academy of Pediatrics (AAP) Concussion Guidelines (August 2010), are available online to assist healthcare providers, student athletes and their families, and school divisions, as needed. What is Concussion? • Zurich 2012 - As Defined by “Concussion in Sport” Group – Concussion is a brain injury and is defined as a complex pathophysiological process affecting the brain induced by biomechanical forces. Several common features that incorporate clinical, pathologic and biomechanical injury constructs that may be utilized in defining the nature of a concussive head injury include: What is Concussion, cont. ? 1. Caused by either a direct blow to the, face, neck, or elsewhere on the body with an “impulsive force transmitted to the head”. 2. Concussion typically results in rapid onset of short-lived impairment of neurological function that resolves spontaneously. However in some cases, symptoms may evolve over a number of minutes to hours. 3. Concussion may result in neuropathological changes, but the acute clinical symptoms largely reflect a functional disturbance rather than a structural injury and, as such, no abnormality is seen on standard structural neuroimaging studies. 4. Concussion results in a graded set of clinical symptoms that may or may not involve loss of consciousness. Resolution of the clinical and cognitive symptoms typically follows a sequential course. However, it is important to note that in some cases symptoms may be prolonged. Symptoms • • • • • • • • • • • Headache “Pressure in Head” Neck Pain Nausea/Vomiting Dizziness Blurred Vision Balance Sensitivity Light Sensitivity Noise Feeling Slowed Down Feeling Like “in a fog” • • • • • • • • • • • (SCAT 3) “Don’t Feel Right” Difficulty Concentrating Difficulty Remembering Fatigue/Low Energy Confusion Drowsiness Trouble Falling Asleep More Emotional Irritability Sadness Nervous or Anxious Common Signs and Symptoms • SCAT3 Sports Concussion Assessment Tool-3rd Edition • Child-SCAT3 Sports Concussion Assessment Tool-Children 5-12 Age: A Factor in Recovery • Younger age - prolonged recovery – High school athletes had prolonged recovery times compared to college athletes (Field et al, J. Pediatrics, 2004) – High school athletes demonstrated longer lasting memory deficits compared to college athletes (Sim et al, J. Neurosurgery, 2008) – High school athletes had prolonged recovery times compared to NFL athletes (Pellman, Lovell, et al, Neurosurgery 2003) Mild TBI: Gender and Recovery • Females may be at greater risk compared to males – Based on NCAA and high school data, in sports played by both sexes, females sustained a higher rate of mild TBI than males (Comstock et al, JAT, 2007) – Large sample of junior high, high school, and collegiate soccer athletes, females had longer recover times than males (Colvin, Lovell et al, AOSSM, 2008) Effects of Repetitive Injury • Studies have suggested that repetitive trauma in athletes is associated with poorer outcomes – Athletes with 3 or more mild TBI’s are 3 times more likely to have an additional injury (Guskiewicz et al, JAMA, 2003) – Athletes with 3 or more prior mild TBI’s were more likely to demonstrate markers of concussion during the period of our study (Collins, Lovell, et al, Neurosurgery, 2002) Concussion Management • Acute Management – Athletic Trainer and/or Physician – Rule out more serious intracranial pathologyMental Status Exam and/or Neurologic Examination (Focal) • Post Injury Management – Prevent against Second Impact Syndrome – Prevent against cumulative effects of injury – Prevent presence of Post-Concussion Syndrome Pediatric Practices ATC in Schools Sports Medicine School Nurses Primary Care Physicians Neurology Emergency Department Neurosurgery Carilion Sports Concussion Clinic Trauma PM&R Psychiatry Parents/ Pediatric Neurology School Vestibular/ PT Psychology Neurosurgery Neuroradiography Behavioral NeuroOptometr y Core Team: • Neuropsychologist “Point Guard” • Physiatrist medical expertise • Physical Therapy vestibular therapy Support Personnel: • • • • • Athletic Trainers Physical Therapists Guidance Counselors School Nurses Parents Initial Interview • • • • • • • • • • Reason For Referral History Risk Factors School History Psychological History Medical History Social History Medications Treated Now By Concussion History • SCAT3 • Dizziness Handicap Inventory • Neuropsychological Testing • Vestibular/Visual-Ocular Screening • Education • Health Behaviors • Recommendations/ Referrals Neurocognitive Testing (NCT) • Cogsport • Headminders (CRI) • ANAM- Automated Neuropsychological Assessment Matrix • IMPACT- Immediate Post-Concussion Assessment and Cognitive Testing • CNS Vital Signs Vestibular / Ocular Motor Screening (VOMS) Mucha, Collins et al (2014) • • • • • Smooth Pursuit Horizontal and Vertical Saccades Near Point Convergence Distance Horizontal Vestibular Ocular Reflex (VOR) Visual Motion Sensitivity (VMS) Rate: Headache, dizziness, nausea, fogginess Convergence: ≥5cm Treatment • Cognitive Rest-giving your brain a rest – If symptoms are not too severe you may go to school. – Phone calls in moderation and soft music may be used for relaxation. – Using a computer for school work is acceptable, but you may need to limit usage if working on computer increases symptoms. – Limit or cease use of electronic devices (for example, video games, TV, texting, internet) Treatment • Physical Rest- giving your body a rest – Take extra naps as needed, no staying up late. – General physical rest until you have no symptoms (headache, nausea, attention/memory problems, and visual problems etc.). – No activities of physical exertion. This includes no physical education and no participation in organized sports. The most important thing is for you not to engage in any activity that puts you at risk for having another head injury until you have completely recovered. Other Interventions • • • • • Sleep Diet Hydration Stress Exercise Treatment Process • After 2 weeks (14-21 days from concussion) difficult patients who are not improving (dizziness, vestibular problems, headaches, sleep and attention symptoms) are referred to: • Physiatrist: Medical Evaluation • Physical Therapist: Vestibular Evaluation • Goal= Return to School and Return to Play Extended Care To Others • • • • • • • • • • • • • Primary Care Physician Physical Therapy Physical Medicine & Rehabilitation Pediatric Neurology Family Sports Medicine Sports Medicine/Orthopedics Neurosurgery Neurology Psychiatry Athletic Trainers Massage Therapy Sports Concussion Specialists- UVA and UNC Behavioral Neuro-Optometrist Accommodations No School Attend School ½ Time School Full Time Homebound Instruction School Flex-time (Student at School in a quiet Room) No tests for Grade until Prepared No Exams, No standardized Tests (SATs, ACTs, SOLs etc.) No Sports or Activities of Physical Exertion No Sports Until caught up with School Work Testing in a Quiet Room Extra Time on Tests and Projects Extra Time For Summer Reading Requirements Other Accommodations (McGrath, 2010) • • • • • • • • Excused Absence from Class Rest Periods During School Day Excuse From Specific Tests and Assignments Accommodations for Light Sensitivity (lights, caps, visors, or sunglasses Use of a Reader-Books on tape Use of a Note Taker Preferential Seating to Lessen Distraction Temporary Assistance From Tutor Graduated Return To Play Protocol Zurich Concussion In Sport, (2014) • • • • • • No Activity Light Aerobic exercise Sport-Specific Exercise Non-Contact Training Drills Full Contact Practice Return To Play Stepwise Progression/Typically 1 Week Clinical Recovery • No self (or other) reported symptoms of concussion. • Performance on neurocognitive testing should be equal to his/her abilities or within Reliable Change Index of his estimated abilities. • When above criteria is met the athlete should go through a 5-step gradual Return To Play Protocol under the supervision of an athletic trainer or medically-supervised parent that includes Light, Medium, and Aerobic Exercise. The idea is to increase exertion, with movement, and finally with controlled contact. When the athlete goes through each step on subsequent days without symptoms he is then cleared to return to sports activities. Typically takes 5-7 days. Return to Sport Multiple Concussions/Complex Cases • Must meet clinical recovery guidelines – Other factors to consider include: • Age • History of ADD, LD, psychological problems etc. • Grades/performance in school back to pre concussion level • History- suggesting increased vulnerability to concussion • Multiple Concussions – and the likely need for retirement from contact sports • Does it seemingly take less biomechanical force to cause another concussion? Return to Sport • Does it take longer to recover with each additional concussion? • With the occurrence of subsequent concussions do concussions occur more frequently? • Does the athlete have persisting functional problems (headaches, attention/learning problems, increased emotional issues) NOTE: In the evaluation and treatment of concussions we are making advances but there is still more we don't know than what we know! Physical Therapy: Evaluation For Vestibular and Ocular Motor Problems • Treatment- Static/Dynamic Visual Training and Home Exercises, Heat /Ultrasound Sound, Soft Tissue Mobilization • Return to Function – School – Play – Work Medical Treatment • Sleep is always addressed- Sleep Hygiene, and Medication-Melatonin and Trazodone • Neck pain, usually muscular, Flexeril then Zanaflex . Consider PT. • Dizziness and Neck Pain-refer to PT for Vestibular Therapy • Headaches-Type with Appropriate TreatmentMusculoskeletal, Cervicogenic, Rebound, Nerve Injury, Post-Traumatic Migraine and Fatigue Related Migraine • Fogginess, Attention/Concentration- Amantadine and Methylphenidate Summary • Heterogeneous Population • Individualized Plan of Care • Multidisciplinary Treatment (Takes a Village) • Specific Trajectories to Pathways Collins et. al (2014) Clinical Trajectories • • • • • • Cognitive/Fatigue Vestibular Ocular Motor Post Traumatic Migraine Cervical Anxiety/Mood Collins et. al (2014) Recent Advances To Rest or Not to Rest • Silverberg and Iverson (2013) raised the question “Is rest after concussion the best medicine?” • Prior to 1940’s complete bed rest was recommended for loss of consciousness of any duration. • Zurich Consensus Guidelines (2008) highlighted rest as the “cornerstone of concussion management” • Exact nature and duration of rest period not definitive. Along a spectrum from complete bed rest to partial activity. • Zurich Consensus Statement (2008) until asymptomatic then institute graded resumption of activities. Problems With Rest • Benefits of rest largely assumed not evidence based. • Ongoing inactivity in chronic stage more detrimental than therapeutic. Other Medical Problems • Rest initially recommended for back pain • Chronic Fatigue Syndrome- rest does not alleviate chronic fatigue. Thought to contribute to maintenance. • Vestibular Disorders- patients avoid activities that require head movement which limits adaptation and resolution of symptoms. • Limited Activity- long thought to be causal mechanism in depression. • Anxiety- may be a cause and consequence of excessive activity. • Avoidance of feared activities maintaining or strengthens negative predictions and self evaluations. Human Studies • Gagnon et al (2009) Children slower to recover after sport concussion. Symptoms greater than 4 weeks. Participated in a controlled/closely monitored rehabilitation program. – Sub-maximal (50-60% maximal capacity) aerobic trainingtreadmill and bicycle – Light coordination exercises – Home program – Visualization • Results- All children were able to resume their normal physical activity at end of program. Recovery was rapid. Human Studies • Gagnon et al (2015). A pilot study of active rehabilitation for adolescents who are slow to recover from sport-related concussion. 10 athletes. Symptomatic more than 4 weeks. • Intervention – – – – – Gradual closely monitored light aerobic exercise Coordination exercises Mental imagery Reassurance/normalization of recovery Stress/anxiety reduction strategies • Results: – Significant decrease in symptoms – Participants reported significant decrease in fatigue – Cognitive function was significantly improved in visual motor processing speed. – Leddy et al (2010) Controlled aerobic exercise rehabilitation after establishing symptom-free exercise capacity via treadmill testing has helped athlete and non-athlete post concussion symptom patients recover. Other Evidence • Thomas et al (2015) Benefits of strict rest after acute concussion – Study of 5 days of strict rest vs. control group (1-2 days with gradual return in physical activity) – Results- recommending strict rest from the ED did not improve symptom, neurocognitive, and balance outcomes in youth diagnosed with concussion. Adolescents recommended strict rest after injury reported more symptoms over course of study. Animal Research • Griesbach (2004) In study with rats, findings suggest that premature exercise compromises compensating responses to the injury. In their studies, early physiological stimulation through voluntary exercise reduced the capacity for neuroplasticity. Rats that exercised 2 weeks after injury benefited. • Iverson et al (2012) Animals allowed to exercise too soon after injury do not show exerciseinduced increases in molecular markers of neuroplasticity. Summary • Silverberg and Iverson (2013) Complete rest exceeding 3 days is probably not helpful. Gradual resumption of pre-injury activities should begin as tolerated (with the exception of activities that have a high MTBI exposure risk) and supervised exercise may benefit patients with persistent symptoms. Revision of Virginia Law-2015 • Return to Learn- Academic Concussion Management Plan • Graduated phases to promote recovery • Instructional modifications • Progressive – Goal: Allowing student athletes to participate in classroom activities without worsening of symptoms – Phases: • • • • Cognitive/Physical Rest Light cognitive mental activity Maximum, moderate, and minimal modifications Full-time classroom participation – 504 plan considered if student-athlete is without significant evidence of improvement at 3-4 weeks Thank You wrwellborn@carilionclinic.org to Our Guests!