File - Lindsey Northup
advertisement

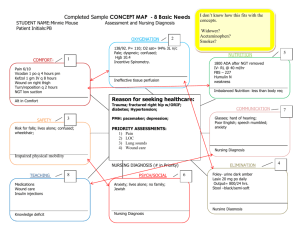
Running head: CLIENT CASE STUDY 1 Critical Care Client Case Study Lindsey Northup Old Dominion University CLIENT CASE STUDY 2 Critical Care Client Case Study The purpose of this case study is to discuss a patient from the clinical setting that we cared for and to incorporate nursing knowledge and theory to discuss planning, providing, and evaluation of holistic care interventions on the patient. The patient that I will be discussing is S. T., a 44-year-old male in the CCU who came to the ED with complaints of prolonged and worsening shortness of breath (SOB) due to an acute congestive heart failure (CHF) exacerbation. Medical Diagnosis: Patho The ultimate reason that my patient ended up in the CCU was due to CHF. His heart failure was due to a combination of mechanisms that failed including being morbidly obese with Pickwickian Syndrome, which is basically weight induced respiratory distress that can cause CHF, which causes pressure on the heart and decreases the hearts ability to adequately pump blood to the body. This damage to the heart also caused the patient to experience acute pericarditis, which is inflammation around the heart, and acute pericardial effusion which is an accumulation of fluid around the heart. In the acute CHF patient, blood backs up into the lungs known as pulmonary edema which causes respiratory complications and a lowered cardiac output. The sympathetic nervous system reacts by increasing catecholamines to compensate for the low cardiac output. This causes a shunting of blood to vital organs, decreasing peripheral tissue perfusion and increasing oxygen demand, which causes further respiratory complications and increases the patients risk for DVT. It also causes vasoconstriction and signals the body to hold onto fluids thinking that volume load is low. Due to the pulmonary edema my patient experienced as a result of his acute CHF, he developed pneumonia which was evidenced by his productive cough of white frothy sputum. The patient also had a history of COPD which was CLIENT CASE STUDY 3 exasperated due to his illness and caused respiratory failure leading to his intubation (Nettina, 2014). Related Signs & Symptoms As a result of the disease process, my patient experienced several signs and symptoms that confirmed diagnosis of his illnesses. With the respiratory system, he experienced shortness of breath, dyspnea, tachypnea, productive cough with white frothy sputum, and had rales and crackles. From the hearts inability to pump to the peripheral area well, the patient experienced wide spread third spacing known as anasarca with 4+ pitting edema. He also had ascites in his abdomen, making it hard to palpation and was very distended. His appetite was decreased, he was fatigued, had lymphedema due to the fluid retention, low urine output, a temporary alteration in mental status due to electrolyte dilution, and was hypercarbic. Due to the third spacing, the patient eventually became septic from bacteremia caused by enterococcus fecalis as well and was found to have a pulmonary emboli from the increased risk of DVT from low peripheral blood flow. Eventually from the hearts pressure, his heart rhythm showed up as atrial fibrillation. Related Symptoms: Labs & Tests The patient’s signs and symptoms also include lab values and tests. Hemoglobin was low at 11.8 due to fluid retention leading to dilution of blood contents. BUN was elevated with a regular creatinine indicating that the patient was dehydrated due to third spacing and had decreased renal perfusion from low peripheral perfusion. PaCO2 was also elevated at 64.3, PaO2 was low at 55, and O2 sats were very low at 87% as a result of having COPD and ineffective breathing and gas exchange from respiratory complications. Chest CT showed that CLIENT CASE STUDY 4 the patient had cardiomegaly and infiltrates as a result of the inflammation and fluid around the heart so a pericardialcenthesis was ordered and drained 250cc from around the heart. Patient Top 5 Nursing Diagnosis The patient S. T. has a complex array of diseases that lead to several health complications. These processes are interrelated and directly affect the other processes. The NANDA nursing diagnosis used will be put in order according to the order of cause of illness. Since the patient’s heart failure is what precipitated the other illnesses, decreased cardiac output is the first diagnosis. Following the heart failure, the nursing diagnosis that follow are ineffective breathing pattern/ airway clearance/ gas exchange, excess fluid volume, anxiety, and actual/ risk for infection. Priority Nursing Diagnosis The priority nursing diagnosis for S. T. is decreased cardiac output related to impaired contractility and increased preload and afterload, fluid around the heart, swelling around the heart, chronic heart diseases, hypertension, obesity, and family history of heart disease. This diagnosis is priority according to the dynamic nurse-patient relationship by Orlando because it states that the role of the nurse is to find out and meet the patient’s immediate needs for help. Since the heart failure and its related signs and symptoms are what caused all the other patients issues, this is the obvious immediate choice. Fix the main issue, then other issues will resolve and the nurse can reprioritize the patient’s needs. Secondary Nursing Diagnosis The next nursing diagnosis pertains to the respiratory system which had several maladaptations. The diagnosis is a combination of ineffective breathing pattern related to need for mechanical ventilation, inability to wean, history of COPD, increased oxygen demand, CLIENT CASE STUDY 5 breathing regulated by CO2, compensatory breathing pattern of pursed lip breathing, and Pickwickian syndrome which caused pressure on the lungs. The next diagnosis is ineffective airway clearance related to respiratory failure, lymphedema swelling of neck, and blocked airway due to increased retained thick secretions. Finally, the diagnosis of impaired gas exchange also works here related to the alveolar edema, elevated ventricular pressures, fluid in the lungs, inflammation of airway, alveolar collapse, and accumulation of fluid in alveoli. The nursing theory that best dictates this as the next priority diagnosis is Henderson’s Nursing Need theory. Her focus is on providing basic human needs so that the patient can care for themselves. Establishment of an airway is highly important for the patient to live and begin to heal. The care team was going through the struggle of trying to wean the patient from the ventilator so that he could be possibly extubated so he could breathe on his own and care for himself. Breathing normally is the first of her fourteen components of human needs theory which is why it is such an important diagnosis. Tertiary Nursing Diagnosis The third priority nursing diagnosis for S. T. is excess fluid volume related to sodium and water retention, third spacing, renin system release to prevent the kidney from releasing fluids as a response to lowered cardiac output, lowered preload, and low volume. This nursing diagnosis is also deemed important in the Henderson Need Theory. The second of fourteen human needs components is the ability to eliminate body fluids which with the lowered cardiac output causing the renin response, prevents the patient to properly eliminate wastes. Pressure from the water retention also affects the lung expansion which thus impairs the number one component of breathing normally. The pressure also alters other components such as rest since it is CLIENT CASE STUDY 6 uncomfortable, protection of the integument due to stretching of edemous skin, and eating due to pressure on the bowel causing anorexic like behavior. Quaternary Nursing Diagnosis The patient’s fourth nursing diagnosis is anxiety related to his inability to communicate with staff due to OG tube and ventilator, difficulty of patient to wean from invasive treatments, recent separation from wife, acute illness, invasion of privacy, difficulty breathing, and inability to move from bed or perform normal ADL’s by self. The patient’s priority anxiety is best described in Orem’s Self-Care Deficit theory. It describes that individuals should be self-reliant and able to perform self-care tasks. When these abilities are taken away it prevents normalcy and return of health which is definitely the case with this patient’s anxiety. He is frustrated with care, communication, family, and future plans for himself and it has caused him to remain in a state of illness. Final Nursing Diagnosis The last priority nursing diagnosis for this patient is the actual and risk for infection that he has going on related to his fluid in the lungs, positive sputum cultures, positive bacterial cultures from his blood, presence of several lines of potential infection, immobility, increased hospital stay, and long-term antibiotic therapy. Neuman’s holistic theory describes how there are many known and unknown universal stressors to a person’s health that can cause further distress and illness by breaking the patients line of defense and immune system. Modes of infection follow along the line of this theories premise by stating that infections can happen any time anywhere and with the patient’s present state, he is at an increased risk to those pathogens. CLIENT CASE STUDY 7 Outcomes for Top 2 Nursing Diagnosis Decreased Cardiac Output There are several expected outcomes with the patient for his cardiac dysfunction. First, it is expected that the patient’s blood pressure will be back to its baseline within one week of treatments. Second, the patient’s heart rate will be back within normal limits an hour after administering cardiac dysrhythmia drugs. Third, the patient will return to normal sinus rhythm after 3 days of cardiac interventions. Fourth, the patient will have a weight loss of 2.2lbs every two days as evidence of decrease in retention of fluid around heart, lungs, and body. Finally, the patient will tolerate getting out of bed before leaving the hospital without complications. Ineffective Breathing/ Airway Clearance/ Gas Exchange For the respiratory complications there are also several expected outcomes. These include, first, that the patient will be weaned to a tracheostomy collar within 1 week. Second, the patient will be able to wean from the ventilator all together within one month. Third, the patient’s O2 sats will remain above 90% while in the hospital. Fourth, the patient will have unlabored respirations at 12-20 breaths a min within one week. Finally, within one week the patient will be able to begin tolerating a daily decrease in PEEP without desating. Interventions for Top 2 Nursing Diagnosis The top two nursing diagnosis for S. T. are decreased cardiac output and several respiratory complicated diagnosis. For the patient S. T. with heart failure, interventions are the same for both diagnosis because when you treat the heart defect you in turn tend to impact the respiratory complications. There are minor differences which I will discuss, but for the most part, interventions will be based on current recommendations for treatment of a patient with CHF. CLIENT CASE STUDY 8 Collaborative Interventions Collaborative interventions are the key for patients with long-term heart failure who have continued cardiac output issues. As stated in many articles, multidisciplinary approaches when caring for the CHF patient include coordination with general doctors, nurses, pharmacists, nutritionists, physical therapists, and cardiologists and when done this way have been shown to reduce medical costs, length of stay in the hospital, and lowered readmission rates as well (Paul & Hice, 2014). Collaborative interventions for decreased cardiac output include monitoring cardiac rhythms, enzymes, and electrolytes. Collaborative interventions for controlling respiratory function include managing vent and PEEP settings with respiratory care, administering O2 per doctor titrated orders, and changing patient position every 2 hours with physical therapy or care partners to promote drainage of secretions (Nettina, 2014). Working with the lab, BNP, CBC, urinalysis, metabolic panels, liver function tests, renal function tests, and serum electrolyte levels need to be evaluated and acted upon with doctors orders for treatment. Scans should also be done with xray techs, MRI staff, and then be read by a cardiologist to determine treatment. Other interventions include placement of intra-aortic balloon pumps, heart transplantation, and ventricular assist devices (Paul & Hice, 2014). Dependent Interventions Dependent interventions rely on other members of the team to manage the patients cardiac output. Examples of these interventions include doctor prescribing of cardiac management drugs. Current recommendations for drugs include ACE inhibitors, ARB’s, beta blockers, and in some cases, loop diuretics, hydral-nitrates, and aldosterone antagonists. Surgical interventions and assistive devices could also be considered dependent intervention. Without the help of dependent interventions, nurse led interventions would not be as successful CLIENT CASE STUDY 9 for the patient with heart failure. Symptom management is the key in the acute setting, and nursing led education is the preventive measure that will keep the patient healthy once they leave the hospital (Yancy, C. W., Jessup, M., Bozkurt, B., et al., 2013). Independent Interventions Nursing independent interventions are the heart of patient care. Turning the patient every two hours helps to drain respiratory secretions that could be contributing to respiratory illness. Other interventions that are nurse led include keeping the head of bed elevated to reduce pressure on the lungs and decrease venous pressure, assessing vitals, suctioning the patient and the most important, is patient education. Nurses in one study were studied for their effectiveness of utilizing the nursing process and NANDA diagnosis to guide their practice with evidence based ways. When nurses chose to do interventions for these heart failure patients, improved ventilation, nutritional status, hydration, gas exchange, and ambulation all were improved (Scherb, Head, Hertzog, Swanson, Reed, Maas, Moorhead, Conley, Kozel, Clarke, Gillette, & Weinberg, (2011). Patient education on cardiac issues with CHF are a critical component of the nurses obligation to their patients. According to Yancy, C. W., Jessup, M., Bozkurt, B., et al. (2013), with just one hour of nurse educator led education intervention at discharge, patient health and outcomes were vastly improved in the long run and those patients who received the information had a better knowledge of their condition in a long term study. Education on cardiac risk for heart failure patients includes explanation of the disease along with signs and symptoms associated with lowered cardiac output as well as the signs that should bring them to see their doctor (Nettina, 2014). One nurse led systematic review on teaching strategies for CHF patients included 2,686 patient reviews with 19 studies. The most common educational intervention by CLIENT CASE STUDY 10 nurses was a one-on-one didactic education session which was found to be a critical part of the educational experience. Distractions from other staff, family, and interventions proved ineffective as a learning tool and it was also found that several sessions over a period of a week was better than one long loaded teaching session (Boyde, Turner, Thompson, & Stewart, 2011). Evaluation For S. T. the plan or care is a slow progressing progress due to his difficulty weaning and non-compliance to suggested health regimens. The patient’s cardiac issues were stabilized thus completing the underlying issues, but respiratory interventions are slow going. Due to the patient’s body habitus, weaning the patient to the trach. collar causes desaturations in O2 levels and level of consciousness. Excess fluid volume is slowly improving with diuretic therapy although the patient still has a large amount of pitting edema in his abdomen and extremities. The patient’s anxiety is also still a point of concern since he has difficulty communicating and is often confused about medical procedures due to a lack of education and teaching. Overall, it would seem that my patient will have to move to a skilled care facility to be able to stay on a vented support system since weaning trials are going so poorly. Conclusion For S. T., a 40-year old African American male with acute congestive heart failure that led to respiratory complications, fluid retention, required intubation, widespread infection, and more, his outcomes are slowly being processed. The heart failure patient is a complex patient which as multi-system issues that requires an intense amount of education on the nurses part to help the patient understand their process. With just one hour of nursing research led education, patient outcomes were significantly increased allowing patients to stay healthier and out of the hospital acute care setting. Interventions should be holistic and individualized, and the nurse CLIENT CASE STUDY should be prepared to collaborate interventions with several departments to care for the complexity of the patients needs. 11 CLIENT CASE STUDY 12 References Boyde, M., Turner, C., Thompson, D. R., & Stewart, S. (2011). Educational interventions for patients with heart failure: A systematic review of randomized controlled trials. The Journal of Cardiovascular Nursing, 26(4), E27-E35. doi: 10.1097/JCN.0b013e3181ee5fb2 Nettina, S. M. (2014). Lippincott manual of nursing practice (10th ed.). Ambler, PA: Lippincott Williams & Wilkins. Paul, S. & Hice, Amber. (2014). Role of the acute care nurse in managing patients with heart failure using evidenced-based practice. Critical Care Nursing Quarterly, 37(4), 357-376. Doi: 10.1097/CNQ.0000000000000036 Scherb, C. A., Head, B. J., Hertzog, M., Swanson, E., Reed, D., Maas, M. L., Moorhead, S., Conley, D. M., Kozel, M., Clarke, M., Gillette, S., & Weinberg, B. (2011). Evaluation of outcome change scores for patients with pneumonia or heart failure. Western Journal of Nursing Research, 35(1), 117-140. Doi: 10.1177/0193945911401429 Yancy, C. W., Jessup, M., Bozkurt, B., et al. (2013). ACCF/AHA guideline for the management of heart failure: A report of the american college of cardiology foundation/american heart association task force on practice guidelines. Journal of the American College of Cardiology, 62(16), e147-e239. doi:10.1016/j.jacc.2013.05.019.