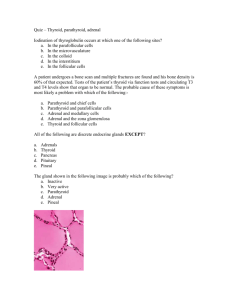
Endocrine quiz explanations
advertisement

Here are the explanations for questions on the endocrine quiz. 1. Acromegaly is a chronic metabolic disorder of adults caused by an overabundance of: A. Parathyroid hormone B. Growth hormone * C. Epinephrine D. Thyroid hormone Easy one. 2. A 58-year-old female has had a 20-pound weight gain over the past two years. She has noticed increasing cold intolerance and sluggishness. On physical exam her heart rate is decreased, and her reflexes are delayed. Her serum TSH is 11.8 mU/L (normal = 0.3 - 3.0), and her T4 is 2.3 micrograms/dL (normal = 4.5 - 12.5). A year ago, anti-TSH-receptor antibodies were detected at high titer. Which of the following diseases does she most likely have? A. Papillary thyroid carcinoma B. Hashimoto thyroiditis * C. Goiter D. Graves disease The symptoms this patient is having are consistent with hypothyroidism, and her T4 level confirms this. It must be a case of primary hypothyroidism, since the TSH is elevated. Among the choices give, only Hashimoto's leads to hypothyroidism. A couple other clues to the diagnosis: the patient is female (not definitive, of course, but Hashimoto's - like other autoimmune diseases - tends to happen more frequently in females), and she has had elevated anti-TSH-receptor antibodies. Anti-TSH-receptor antibodies can be seen in both Hashimoto's and Graves disease (weird; they do totallly opposite things in the two diseases). There is another type of antibody called the anti-peroxidase antibody which is more specific for Hashimoto's. 3. Extreme hypothyroidism in adults is called: A. Addison disease B. Graves disease C. Myxedema * D. Rickets By the way, the term for severe congenital hypothyroidism is "cretinism", from the French Cretin, or Christ-like. It was coined many many years ago, when these children were thought to be so severely mentally retarded that they were incapable of sinning. 4. All of the following are true regarding type I diabetes EXCEPT: A. It accounts for 90% of all cases of diabetes * B. The body makes little or no insulin C. Daily injections of insulin are required to sustain life D. Long-term complications may include: hyaline arteriolosclerosis, proliferative retinopathy, nodular glomerulosclerosis, and peripheral neuropathy E. It is usually diagnosed in childhood or early adulthood The point of the question is to remind you that type I diabetes (insulin-dependant, or juvenile, diabetes) is much less common than type II diabetes (non-insulin dependant, or adult-onset, diabetes). Type I is usually much more severe, too, with little or no insulin secretion at all. Patients rely on insulin injections for their entire lives. 5. Addison disease is caused by damage to the: A. Pancreatic islets B. Thyroid gland C. Parathyroid glands D. Adrenal cortex * Hopefully the case we look at in class will help you remember some things about Addison disease. 6. Positive Chvostek and Trousseau signs indicate: A. Botulism B. Rickets C. Tetany * D. Bell's palsy Tetany is a general name for a bunch of clinical symptoms related to hypocalcemia. These include mild things, like muscle twitches and carpal spasm, and severe things, like laryngospasm and seizures. Chvostek sign is elicited by tapping or stroking the facial nerve (above the mandibular angle, adjacent to the earlobe); facial twitching or spasm results. Trousseau sign occurs when you apply a blood pressure cuff to the patient's arm; carpopedal spasm results. I remember which is which by remembering that to elicit Chvostek sign, you stroke the cheek. 7. A 55-year-old patient presents with recently diagnosed diabetes. He also has front teeth that are more widely spaced than normal and have recently begun to flare. Which undiagnosed disease does this patient most likely have? A. Gigantism B. Hyperparathyroidism C. Paget's disease of bone D. DiGeorge syndrome E. Acromegaly * Sometimes, in patients with acromegaly, the tongue gets so big that it pushes the anterior teeth foward, so that they flare out. Another dental sign that may occur is wide spacing of the teeth (as the jaw grows bigger and bigger). 8. A patient presents with osteomalacia, loss of the lamina dura around the teeth, brown tumors in bone, and duodenal ulcers. His family reports his personality has changed. Which of the following disorders should you suspect him of having? A. Hyperparathyroidism B. Hypoparathyroidism Dr. Koutlas will talk about the "stone (kidney stones), bone (brown tumors), groan (GI symptoms) and moan (mental changes)" symptoms in hyperparathyroidism. When you have too much PTH around, your serum calcium goes down. Osteoclasts chew up bone at a greater rate, leading to lamina dura loss, demineralization of alveolar bone, and - if severe enough - brown tumors. These are not tumors at all, but just areas of bone that have cystic degeneration and hemorrhage - hence the brown color - to such an extent that it shows up as a tumor-like mass on x-ray. 9. All of the following statements regarding multiple endocrine neoplasia II are true EXCEPT: A. Patients have increased incidence of thyroid carcinoma B. Patients have increased incidence of pheochromocytoma C. Patients have increased incidence of mucosal neuromas D. It is autosomal recessive * E. Differential diagnosis includes von Recklinghausen's disease The Multiple Endocrine Neoplasia (MEN) syndromes are genetic syndromes that predispose patients to developing endocrine tumors. Endocrine tumors occuring in patients with MEN syndromes tend to be more aggressive and occur at younger ages than their sporadic counterparts (i.e., the prognosis of medullary carcinoma of the thyroid is pretty bad when it occurs sporadically, but when it occurs in the context of MEN, it happens at a younger age and has an even worse prognosis). There are two main kinds of MEN syndromes (MEN 1 and MEN 2); MEN 2 is further split into 2a and 2b. While both types 1 and 2 increase the patient's risk of developing multiple endocrine tumors (hence the "MEN" name), there are some differences in the specific kinds of endocrine tumors commonly seen in each syndrome. In class, we will boil it down to the simplest possible terms. The big thing about MEN 2 is that patients have a markedly increased risk of developing medullary carcinoma of the thyroid. These patients can get other things too (like pheochromocytoma, and occasionally parathyroid hyperplasia), but the thing that virtually all patients end up getting is medullary carcinoma of the thyroid. Patients with MEN 1 don't have an increased risk of medullary carcinoma of the thyroid - but they do have an increased risk of a whole bunch of other things, including parathyroid hyperplasia, pancreatic carcinoma, and pituitary adenoma (the three Ps). So, to simplify it to a ridiculous degree: MEN 2 = medullary thyroid carcinoma. MEN 1 = everything else. It's more complicated than that, of course. One of the details that this question addresses is the division of MEN 2 into two subtypes. MEN 2a is as described above (medullary thyroid carcinoma in virtually all patients, sometimes pheochromocytoma, and occasionally parathyroid hyperplasia). MEN 2b is like MEN 2a, except (1) patients usually do not develop parathyroid hyperplasia, and (2) they often have other unusual findings, like neuromas (benign tumors of nerves) or a Marfanoid habitus (very tall, with long fingers, arms, and legs). Okay, so back to the question. A is true. B is true (not everyone gets this, like medullary thyroid carcinoma, but the incidence is increased). C is true in MEN 2b. D is not true. In MEN 1, the genetic mutation is in the MEN gene, which is a regular old tumor-suppressor gene. A tumor suppressor gene puts brakes on cell growth, and if you get a genetic mutation that inactivates the gene, the brakes will come off and the cell will grow like crazy. Like any tumor suppressor gene, you have to lose both alleles to get disease (so you'd call it autosomal recessive). It's your basic run-of-the-mill old tumor suppressor gene, just like old run-of-the mill Brad Pitt. You have to inactivate the gene to get tumors, just like big old inactive Brad Pitt. (Sorry Brad, but we need an analogy and you’re it.) In MEN 2, the genetic mutation is in the RET gene, which is a proto-oncogene. An oncogene is a normal gene that encodes something that makes a cell grow (like a growth receptor or something). If you mutate an oncogene in such a way that it has a gain of function (meaning it's always turned on), then it becomes a proto-oncogene, and you get uncontrolled cell growth. You only need to mutate one copy of a proto-oncogene to get malignancy (unlike tumor suppressor genes), so you'd call MEN 2 autosomal dominant. This is unusual! Most genetic syndromes that predispose people to getting cancers have abnormalities in tumor suppressor genes, not proto-oncogenes! So - the genetic abnormality in this syndrome is very unique (just like John Cleese, who is truly one-of-a-kind). And not only that, but the gene is always turned on in this syndrome (just like John Cleese - at least when he's holding my picture. This will make sense after class). Whew. Finally, E is true. Wait a minute, you're saying - didn't you say von Recklinghausen's disease was that disease with all the brown tumors? Osteitis fibrosa cystica? Yes, I did say that. It just so happens that there are TWO von Recklinghausen's diseases. How crazy is that? One von Recklinghausen's disease is caused by hyperparathyroidism and manifests with brown tumors. It's also called osteitis fibrosa cystica. The other von Recklinghausen's disease is a hereditary disorder that manifests with multiple, diffuse neurofibromas (a benign tumor of nerves) and many other abnormalities. It is one of two diseases called neurofibromatoses. Wikipedia has good articles about the bone-related von Recklinghausen's disease, the neurofibromatosis type of von Recklinghausen's disease, neurofibromatosis in general (types 1 and 2), von Recklinhhausen himself, and the elephant man (who was thought until recently to have suffered from the neurofibromatosis form of von Recklinghausen's disease). 10. Which of the following symptoms would be most likely in a patient with pheochromocytoma? A. Headache * B. Hypotension C. Bradycardia D. Dry skin E. Hypoglycemia Pheochromocytoma is a tumor of the catecholamine-producing cells of the adrenal medulla. The catecholamines (epinephrine and norepinephrine) do a bunch of things; they are the "flight or fight" hormones that get released under severe stress. One of the main things they do is increase blood pressure - so that's why people with pheochromocytoma can present with hypertension. Because the catecholamines may be released in waves, the hypertension may be paroxysmal. And because it doesn't respond well to normal blood pressure medications, it can be termed persistent. Other things catecholamines do in real life (not so much in this tumor, though) are: increase the basal metabolic rate and raise the blood glucose level. By the way, neuroblastoma is another tumor we will talk about in the context of adrenal medulla. It's a tumor of neural crest cells, and it's the most common malignant tumor of childhood. It can sometimes secrete hormones (weird - it's composed of neural-type cells, not hormone-producing cells - but tumors can do whatever they want) including catecholamines, which can result in increased heart rate and blood pressure. Most neuroblastomas, however, present with an abdominal mass (or a sense of fullness or pain in the abdomen), not with hypertension or tachycardia. Back to the question. Pheochromocytoma can present with a lot of different symptoms, the most common of which is hypertension. If you want another mnemonic (who doesn't?), remember the 6 Hs (all of which are related to high catecholamine levels): Hypertension Headache Hyperhidrosis (sweating) Heart palpitations (tachycardia) Hypermetabolism Hyperglycemia 11. Cushing Syndrome may be caused by all of the following EXCEPT: A. An adrenal cortex tumor B. A posterior pituitary tumor * C. A paraneoplastic syndrome D. Iatrogenic factors Sneaky - Cushing Syndrome may be caused by an anterior pituitary tumor, not a posterior one. 12. Patients with Graves Disease may show all of the following EXCEPT: A. Decreased appetite * B. Exophthalmos C. Heat intolerance D. Tachycardia E. Irritability Patients with Graves Disease show some or all the symptoms of hyperthyroidism (including tachycardia, heat intolerance, sweating, weight loss, diarrhea, mental changes, etc.). Many patients also show exophthalmos, and a few have a dermopathy. 13. Which of the following is associated with Addison disease? A. Central obesity B. Diabetes C. Osteoporosis D. Hypotension * E. Increased appetite Patients with Addison disease have little or no aldosterone and cortisol secretion. Therefore, there are problems with blood pressure and salt regulation (patients get hyponatremic and hypotensive, and crave salty foods), and problems related to the low cortisol level (like hypoglycemia and a decreased immune response to infections). Remember that patients with Addison disease will also show hyperpigmentation because the pituitary responds to the low glucocorticoid levels in the blood by making more ACTH, and ACTH comes from a larger precursor molecule that gives rise to melanocyte-stimulating hormone! The hyperpigmentation may manifest as diffuse skin bronzing, or it may show up in focal areas, like skin folds, or in the mouth, as seen in this patient: 14. Patients with hypothyroidism may show all of the following symptoms EXCEPT: A. Short stature B. Retention of deciduous teeth C. Stunted skeletal growth D. Hair in the oral cavity * E. Mental slowness Eww. If anything, hair growth would slow down. Everything slows down in hypothyroidism. 15. Which of the following is a function of the parathyroid glands: A. Secrete calcitonin B. Decrease serum calcium C. Stimulate osteoclasts * D. Increase renal reabsorption of phosphate Easy one.