File
advertisement

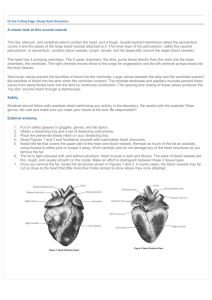
Physical Therapy for Cardiovascular disorders RHPT 482 Credit hours: 2T+1C Course Instructor: Ahmad Osailan Course Description • The course is designed to teach and perform clinical practice for the management of CVD. Anatomy and physiology of the cardiovascular system • Objectives : • Be familiar with the anatomy of the heart and vascular system Size of the heart Location of the heart Layers of the heart Chambers of the heart Vascular system and its layers Brief physiology of cardiovascular system Cardiovascular system • Consist of : Heart Blood vessels Lymphatic Overview of the heart • Heart Definition: “a pump that moves the entire body volume to and from the lungs and tissues.” • In Humans, Heart is 250 g in Male to 350 in Female. (Size of a fist) • It produces ~ 5 Litres of Blood every minute • Myogenic: ability to generate its own contraction Location of the heart • • • • • • posterior to sternum medial to lungs anterior to vertebral column base lies beneath 2nd rib apex at 5th intercostal space lies upon diaphragm • posterior to sternum • medial to lungs • anterior to vertebral column • base lies beneath 2nd rib • apex at 5th intercostal space • lies upon diaphragm Heart Structure • • • • • Consist of : Pericardium Walls of the heart Four champers Four valves Covering of the Heart • Pericardium: • Def: Is a fibrous sac surrounds the heart and roots of great vessels. • Divided to : • Serous pericardium: smooth inner • Fibrous pericardium: Tough fibrous tissue outer pericardiun Serous pericardium Parietal layer Fibrous pericardium Visceral layer Pericardium • Serous pericardium Parietal layer: lines the inside of fibrous pericardium Visceral layer: adheres to the surface of the heart. • Fibrous pericardium: Protects the heart and serous membrane Heart Wall layers • Epicardium: outer layer • Myocardium: Middle layer • Endocardium: Inner layer Endocardium • Inner lining • Smooth (Endothelial) surface that permits blood to move easily through the heart • Continuous with lining of blood vessels Myocardium • Middle layer made of cardiac muscle (Myocardium) • Forms the bulk of the heart wall • Contains the septum- a thick muscular wall that completely separates the blood in the right side of the heart from the blood in the left side. Epicardium • • • • Protective, outer layer of the heart wall same as the visceral pericardium The coronary blood vessels that nourish the heart wall are located here Champers of the Heart • • • • Heart has Four Champers 2 atria (atrium) 2 ventricles 2 atria separated by interatrial septum 2 ventricles separated by interventricular septum. Champers • • • • Right Atrium Thinner wall than ventricles Receives deoxygenated blood from vena cava Passes blood through tricuspid valve into right ventricle Right Ventricle • Thicker wall than atria • Comprises most of anterior surface of heart • Circulates deoxygenated blood to lungs through the pulmonic valve into pulmonary trunk Left atrium • Receives freshly oxygenated blood from pulmonary vein • Passes blood to left ventricle through mitral valve Left ventricle • Receives blood from left atrium • Thickest myocardial wall • Forms apex of heart • Sends blood to systemic circulation via aorta Valves of the heart • Function- prevent blood from flowing backwards • Responds to changes in pressure • Two types of valves in heart Atrioventricular valves (AV) Semi-lunar valves • Semilunar valves • Located at exit of ventricles, originiate from endothelial lining of veins • Heart contains two semilunar valves • Pulmonic • Aortic (Frequently damaged by Htn) Atrioventricular Valves • Valve cusps are connected to papillary muscles • Chordae tendineae tiny collagen cords • that anchor cusps of valve to papillary muscles Atrioventricular Valves • Left AV valve (Mitral, bicuspid) • Contains 2 cusps • Subject to abuse • Right AV valve (Tricuspid) • Contains 3 cusps • Not subjected to great abuses Blood circulation • There are 2 circulatory pathways: Pulmonary circuit Systemic circuit Blood circulation • Pulmonary circuit: Deoxygented Blood received by Right Atrium from Superior and inferior vena cava-> pass through Tricuspid V-> Right Ventricle -> through Pulmonary V -> pulmonary trunk -> pulmonary arteries -> R + L Lung. Blood Circulation • Systemic Circuit: Oxygenated blood returns from lungs to heart through -> pulmonary veins -> Left Atrium -> pass through Mitral V -> Left ventricle -> pass through Aortic V -> aortic arch -> whole body Blood Vessels • • • • Function: Distribution of blood Exchange of materials with tissues Return of blood to heart • Structure: • Most have 3 layers surrounding a hollow lumen Blood Vessels • Arteries Veins • Arteriole Venule • Capillary network General structure of Blood Vessels • • • • Arteries and Veins Have 3 Tunics: Tunica Externa ( Adventetia ) Tunica Media Tunica Intema • Capillaries composed of endothelium ( tunica intema) Blood vessels • Tunica Intema: • Inner smooth layer • Simple squamous epithelium • Continous with endocardium • Present in all vessels Blood Vessels • • • • Tunica Media: Layer of smooth Muscles Contain Elastin Supplied by Sympathetic division of ANS • Area of vasoconstriction and Vasodilatation Blood Vessels • Tunica Externa • Layer of Connective tissue • Elastic and has collagen fibres Arteries • • • • • Characteristics: Thick walled Lots of Elastin in all tunics Stretchable wall to recoil and propel blood Withstand and regulate BP Fluctuations Veins • • • • Characteristics: Thin walled Lumen is larger than arteries Less stretchable than arteries Capillaries • • • • • Characteristics : Smallest vessel Large enough for 1red cell One tunica only (tunica intema) Very thin, Why? Blood supply to heart Coronary arteries • 2 Main Coronary Arteries •Right CA- branches into some marginal arteries; supplies RV and posterior of heart •Left CA- branches into • AIA (LAD) and • circumflex; supplies LV Arterial supply to heart • Originates from the base of aortic artery • Only 5% of ejected blood is received through to innervate the heart (Myocardium) • Many branches directed to the Left ventricle, Why? • Coronary arteries traverse the heart forming a vast network of capillaries Venous drainage • Transport deoxygenated blood to coronary sinus • Coronary Sinus drains into RA Discussion • • • • Which chamber among ventricles is thicker? Which one is thicker among blood vessels? How many layers surrounding the heart? How many valves and what is the type of each one? • How many Circuit in cardiovascular system? Physiology of cardiovascular system • Mainly the heart is a pumping machine. • To pump it require force to generate contraction. • Since the heart is mainly composed of cardiac muscles (myocyte), • it has similar functions and structure like skeletal muscles with some variations Myocyte • • • • • • Characteristics: Striated cells Short cells Mononucleus (one nucleus only) Very large mitochondria (Many ATP) Has intercalated disks Types of cells in the heart • 2 types: 1. Contracting cells (Myocytes) - concept of Actin and myosin for contraction - depends on presence of Ca - action potential is 30X longer than skeletal Muscles 2. Conducting cells (intercalated disks, SA node…) Conduction system • Non-contractile cells, • self-excitable, • generate spontaneous action potentials, • Trigger heart contractions. Conduction system is located in: SA node AV node AV bundle Purkinje fibres Conduction system • Three potential areas capable of beginning cardiac conduction • SA Node- Located in right atria; 60-100 bpm • AV Node- Located at AV junction; 40-60 bpm • Ventricular System- Ventricles; < 40 How Heart beat is initiated • Through Action potential of SA node How the myocardium is contracting • Through action potential of cardiac muscles Cardiac cycle • • • • • • What is cardiac cycle: Is a series of events occur when heart beats Mainly consist of: Systole period: Ventricles contract Diastole Period: Ventricles relaxed Duration: last for 0.8 Seconds Cardiac Cycle Cardiac output • Cardiac output: is the amount of blood pumped by each ventricle in one minute • CO= HR x SV • Heart rate: is the number of beats per minute • Stroke volume: is the amount of blood pumped by one ventricle with each beat. Stroke Volume • SV= End Diastolic volume – End systolic volume • EDV= amount of blood in a ventricle during diastole before contraction • ESV= amount of blood remaining in a ventricle after contraction. • Ejection Fraction (EF): percentage of blood ejected from a ventricle. Regulation of Heart rate • • • • • • • Chemicals. Na, K Autonomic nervous system Positive chronotropic factors. HR Atropine Dopamine Epinephrine Negative chronotropic factors. HR Beta blockers such as Acetylcholine Digoxin Discussion How the blood is travelling through Heart chambers? What is Early filling and atrial filling? How to detect the electrical activity of the heart?