Paper on fructose vs. glucose absorption
advertisement

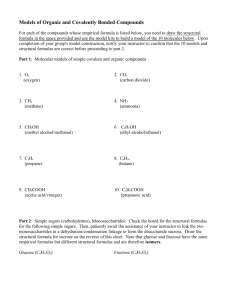
This paper begins by explaining a little about carbohydrates, looking at how the consumption of refined carbohydrates has increased in the past 30-40 years and how that increased consumption has led to some metabolic syndromes, such as type 2 diabetes. This paper goes on to explain the different biochemical pathways in which glucose and fructose are absorbed, and how this might lead to metabolic syndromes, especially for fructose. Lastly, this paper looks at two conditions that are indicators of type 2 diabetes – nonalcoholic fatty liver disease and increased blood levels of uric acid – and the role that fructose plays in their development. The Dietary Reference Intakes recommends humans receive about half of their caloric intake from carbohydrates, which come in the form of monosaccharides, disaccharides, oligosaccharides and polysaccharides. These recommendations for caloric intake are set because carbohydrates are an important source for energy, which also includes the other two macronutrients -- fat and protein. Carbohydrates are an important source of fuel for the brain and nervous system, compared to fat and protein, and can be broken down more efficiently than protein as an energy source. Fat’s job is to store energy for later use. Constructed from the atoms of carbon, oxygen and hydrogen, carbohydrates are polyhydroxy aldehydes or ketones. Monosaccharides are the simplest form of carbohydrates. Monosaccharides cannot by hydrolyzed to a simpler compound, whereas disaccharides are two monosaccharides joined together by a glycosidic bond that can be separated into monosaccharides. The three types of monosaccharides are fructose, glucose and galactose, while the three types of disaccharides are sucrose, maltose and lactose. Oligosaccharides, which can come from legumes, are chains of 310 monosaccharides and polysaccharides, which are starches stored in plants, are long chain polymers of monosaccharides. Fructose and glucose are the primary sources of sugar in the diet and naturally come from fruits and vegetables, respectively, but fructose and sucrose, which is made up of fructose and glucose, have been added to Western diets over the last 100 years in the production of beverages and packaged foods. As a result, one focus of recent research and public health is on fructose and glucose because of the changes in public consumption of these sugars and their effects on health. From 1909 to 1963, carbohydrate consumption in America dropped from about 500 grams per day to 374 grams per day.1 At the same time, fiber intake decreased by nearly 40 percent. But, carbohydrate consumption went back up to 500 grams per day from 1963 to 1997, while fiber intake did not increase. Researchers concluded the increase in carbohydrate intake from 1963 to 1997 and the lack of increase in fiber intake from 1963 to 1997 shows there was an increase in consumption of refined sugars, mainly high fructose corn syrup, over this time frame. Refined sugars are thought to have replaced whole grains in the U.S. diet during this time. Additionally, the refining of carbohydrates increases caloric density and decreases dietary fiber. Commercial production of high fructose corn syrup began in 1967 and as of 2002, HFCS, which is used in many produced beverages and packaged food products, represented about 56 percent 1 of the sweetner market in the U.S. The total per capita use of these sweeteners has increased by 86 percent from 1909 to 1997. These changes in diet, researchers believe, correlate with the rise of obesity and its associated health problems. The rate of obesity went up by 80 percent from 1980 to 1997 and the prevalence of type 2 diabetes increased by 47 percent. Current tallies say nearly 26 million Americans have diabetes and about 79 million are pre-diabetic, those with blood-sugar levels higher than normal but not high enough to be diagnosed with type 2 diabetes. Several health problems may be attributed to this change in diet and researchers have begun trying to understand the difference between the metabolism of fructose and glucose in hopes of confirming the above correlational findings. Digestion of some carbohydrates begins in the mouth, where they are acted upon by the enzyme alpha-amylase, and continues in the stomach until the hydrochloric acid in the stomach deactivates the enzyme. Most of the digestion and absorption of carbohydrates occur in the small intestine. Carbohydrates are broken down into monosaccharides and are absorbed by enterocyte cells in the small intestine and transported to the blood stream via an intricate process. The villi and microvilli structures on the surface of the small intestine facing the bolus – the lumen side or apical membrane side -- increase the surface area of the gastrointestinal tract to allow for better absorption. The absorption of glucose differs from fructose. Glucose uses a sodium-glucose cotransporter protein and a facilitative transporter to get from the apical side of the enterocyte to the blood.2 The sodium-glucose cotransporter (SGLT1) is embedded in the apical membrane and takes up glucose and sodium. The sodium and sugar are released into the enterocyte, where the facilitative transporter protein GLUT2 picks up the glucose and transports it across the cell to the side next to the blood and releases the glucose into the blood. The protein GLUT2 can also embed in the apical membrane and transport glucose to the basolateral memembrane (blood side of the cell). Fructose, however, is transported across the apical membrane by a different facilitative transporter called GLUT5. Researchers believe GLUT5 is specific only to fructose such that fructose’s transport across the enterocyte is not inhibited by glucose, but that GLUT2 can transport both glucose and fructose in helping to keep these monosaccharides from leaving the small intestine unabsorbed. The protein GLUT2 moves to the apical membrane in response to glucose in the lumen. The job of SGLT1, as the only transporter capable of moving glucose against a concentration gradient, is to get glucose into the enterocyte. As the concentration of glucose increases in the lumen, SGLT1 transports glucose into the enterocyte and GLUT2 moves to the apical membrane to also pick up glucose. The GLUT2 in the apical membrane can become the major route of glucose absorption from the lumen. But GLUT2 is not a protein that moves glucose against a concentration gradient so it moves away from the apical membrane during times of low glucose levels in the lumen, otherwise it would allow glucose to leak out of the enterocyte and into the lumen. The job of GLUT2 is to put glucose into the blood to send glucose to the liver and muscles or take glucose out of the blood to provide energy for the enterocyte. Research into GLUT2 may have 2 implications for the study of diabetes. Kellett and Brot-Laroche speculated that eating foods high on the glycemic index might result in high levels of GLUT2 in the apical membrane, which would increase levels of glucose in the blood. They found that during starvation (to the point at which the body uses protein for energy) SGLT1 protein increased threefold and that GLUT2 in the apical membrane was abolished. Another study3 suggests that a 65 percent fructose-enriched diet inhibited GLUT2 by 50 percent. The role of GLUT2 may be just one of many in the study of diabetes. Moving along, however, glucose and fructose leave the enterocyte, get taken up in the blood and are headed for the next important step in their metabolism, the liver. Glucose and fructose are transported from the enterocytes to the liver via the hepatic portal vein, the primary blood supply to the liver. Some glucose is stored in the liver as glycogen or used for energy in the liver, while the rest returns to the blood and is distributed to skeletal muscle, kidney and adipose tissues. As with absorption in enterocytes, glucose requires protein transport carriers to get into cells. Most cells use a carrier called GLUT1, while liver and beta cells use GLUT 2 and skeletal and cardiac muscle cells and adipose tissue cells use GLUT4 transporters.4 In skeletal muscle and adipose tissue, glucose uptake by the cells is dependent upon insulin, a hormone that stimulates enzymatic activity for the synthesis of glycogen, as well as the macronutrients fat and protein, and works to regulate blood-glucose levels. Insulin stimulates GLUT4 transporters to concentrate on a cell membrane so it can move glucose into the cell.5 Beta cells in the pancreas release insulin when blood glucose levels rise. The release of insulin stimulates the uptake of glucose by cells in the body. The goal of this dynamic is to maintain a blood-glucose concentration of 5mM. If blood-glucose levels fall below 5mM, insulin production is inhibited and the pancreas releases the hormone glucagon to activate the generation of glucose from glycogen. Glycogen can be stored in muscle tissue so it can be used quickly as an energy source upon demand. Glycogen is also stored in the liver and is used to help maintain blood-glucose levels. In type 2 diabetes, tissues lose their sensitivity to insulin and the tissues no longer respond to insulin by taking glucose out of the blood stream and into the cell. Blood glucose levels don’t drop so the pancreas keeps making insulin and rises to high levels with little effect on glucose levels. Over-worked, the pancreas eventually starts to fail, reducing insulin output. Chronic excessive glucose can cause vision problems, damage blood vessels and nerves and disrupt blood flow to the kidney. Damaged blood vessels can lead to loss of circulation, as well as heart disease. Therefore, the healthy regulation of blood-glucose levels is of great importance. When glucose enters a muscle cell, glycolysis begins as an enzyme called hexokinase phosphorylates glucose – using ATP to add a phosphate (taken from ATP) to glucose to make glucose-6-phosphate.6 In liver cells, glycolysis begins as glucose and is phosphorylated by glucokinase. The difference in enzymes is notable in that glucokinase has the ability to phosphorylate glucose quickly so that blood-sugar levels can be maintained in times of carbohydrate-rich meals. Hexokinase slows down its phosphorylation when the cell has enough 3 glucose-6-phosphate. In both locations, glucose is phosphorylated again and then split into two molecules of glyceraldehyde 3-phosphate. Another series of phosphorylation steps eventually convert these two molecules into pyruvate. Also, when glyceraldehyde 3-phosphate is initially phosphorylated, it happens via the reduction of NAD+ to NADH. While it took 2 ATP to make two molecules of glyceraldehyde 3-phosphate, the conversion to pyruvate generated 4 ATP for a net gain of 2 ATP at the end of glycolysis. Glycolysis also required an NAD+. What happens next to pyruvate depends on the body’s needs. Pyruvate can be reduced into lactate, which enters the CORI cycle in the liver to make glucose and generate NAD+ for glycolysis. The rate of lactate production equals the rate of glycolysis. Pyruvate can also enter a cell’s mitochondria to be reduced to Acetyl-CoA by the enzyme Pyruvate Dehydrogenase. Acetyl-CoA enters the Krebs Cycle, where much of the energy in the chemical bonds of carbohydrates is used to form ATP to fuel cellular functions. The oxidation of Acetyl-CoA nets 36-38 ATP. The Krebs Cycle also produces 3 NADH and one FADH2, which are electron transporters, that are used in the electron transport chain. NADH and FADH2 in the matrix go to a protein in the inner membrane of the mitochondria and send hydrogen ions out into the intermembrane space. As more and more hydrogen ions gather in the intermembrane space, they become more concentrated out there and want to flow back into the matrix, where the concentration of hydrogen ions is much less. To get back into the matrix, the hydrogen ions pass through the ATP-synthase, which is a kind of pump that generates ATP. The final step of ATP production is the end-game for glucose. But, overall, the conversion of glucose to ATP is done to meet the body’s demand for energy. Fructose is a different story as its conversion to energy is not regulated by the body’s demand for energy. Insulin does not regulate the uptake of fructose as it does with glucose. In the liver, the enzyme fructokinase phosphorylates fructose into fructose-1-phosphate, which is then acted upon by aldolase to make a glyceraldehyde and dihydroxyacetone phosphate.6 Triokinase phosphorylates glyceraldehyde into glyceraldehyde 3-phosphate, which can be made into pyruvate. Dihydroxyacetone is phosphorylated into glycerol-3-phosphate, which is made into lipoproteins or triglycerides.7 Notable in this is that fructokinase is specific to fructose because fructose is a ketohexose and fructokinase is a ketohexokinase, whereas glucose is an aldohexose, meaning that the two monosaccharides are different and require different enzymes for phosphorylation. Meanwhile, as fructose ends up as glyceraldehyde 3-phosphate its path to this point was different than glucose’s path in that fructose skipped glycolysis. This means that fructose can be made into pyruvate much quicker than glucose.7 There is also more fructokinase in the liver, which helps extract fructose in the liver and turn it into glycogen or fat. Another interpretation of the difference between fructose and glucose is that glucose is regulated so that ATP demand can be met when needed, whereas fructose uses ATP to make fructose-1-phosphate and doesn’t generate ATP, compared to the glycolysis of glucose, which generates two ATP.8 When ATP is phosphorylated, it loses a phosphate and becomes ADP and ADP becomes AMP 4 after another round of phosphorylation. If fructose decreases phosphate levels by using two phosphates without replenishing them, then adenosine monophosphate is broken down by adenosine monophosphate deaminase, which eventually generates uric acid. Uric acid impacts on diabetes will be discussed later. In general, however, research shows that fructose metabolism in the liver is faster than that of glucose and that more of fructose than glucose is put into liver glycogen stores.9 Obtaining 25 percent of energy needs from fructose-sweetened beverages compared to the same amount of glucose-sweetened beverages over 10 weeks led to other concerns in one study for older, obese adults.10 Fructose consumption led to a much bigger weight gain in visceral adipose tissue and abdominal fat compared to glucose consumption. Greater abdominal fat initially was linked to increases in risk for type 2 diabetes (but more on that later), while visceral fat increases in the liver will be discussed later. Increased fructose consumption also led to an increase in de novo lipogenesis (DNL -- the making of fatty acids from carbohydrates in the liver) and a huge increase in lipid (fat) and lipoproteins (cholesterol) in the blood compared to glucose. The role of fructose in increasing DNL, which leads to high levels of triglycerides that contribute to fatty liver, and increased lipid in the blood is of concern considering it is a component of type 2 diabetes. This study also found that triglycerides didn’t clear out of the blood stream as fast for the fructose group compared to the glucose group. Generating uric acid and a nonalcoholic fatty liver from an increase in DNL and lipids in the blood due to increases in fructose intake have implications when looking at how much fructose has been added to a typical Western diet since the 1970s and the correlational incidences in type 2 diabetes. Setting aside uric acid for the moment, this next section will look at nonalcoholic fatty liver disease (NALFD) and its link to fructose. The condition of NALFD is similar to alcoholinduced liver damage, but occurs in those who do not drink too much alcohol.11 The condition of NALFD can progress to end-stage liver disease and is associated with obesity, type 2 diabetes and hyperlipidemia – all of which have been linked to excessive intakes of fructose or sucrose. Increased levels of triglycerides in hepatocytes (liver cells) are believed to be linked to NAFLD. But insulin resistance is another factor in the development of this condition. Between 30 and 100 percent of patients with NALFD were reported to be obese. Those inflicted with NALFD showed a prevalence of type 2 diabetes of between 10 and 75 percent. Hyperlipidemia prevalence was between 20 and 92 percent in NALFD patients. Those with this condition report no symptoms or signs of liver disease when diagnosed. But many report fatigue and feeling full or discomfort on the right side of their upper abdomen. A liver beyond its normal size is the only physical finding in most patients. Nonalcoholic fatty liver disease can lead to nonalcoholic steatohepatitis, a liver disease which may lead to liver cirrhosis and hepatocellular carcinoma, the most common type of liver cancer. 5 Fructose plays a role in nonalcoholic fatty liver disease.12 Fat buildup in the liver through excess intakes of fatty acids can occur from increased DNL. It can also occur from impaired triglyceride clearance and the reduction of VLDL clearance. Because fructose metabolism is unregulated, it as a big source of glycerol 3-phosphate and acetyl-CoA, which increases lipogenesis. When excess acetyl-CoA can’t be metabolized in the mitochondria, the extra acetylCoA leaves the mitochondria and goes to the cytosol in the form of citrate, which leads to DNL. Two proteins mediate DNL called carbohydrate response element binding protein (ChREBP) and sterol regulatory element binding protein 1c (SREBP-1c). Fructose activates ChREBP and acts with SREBP-1c to stimulate lipogenic genes. Fatty acids are converted into triglycerides, which then leave the liver in VLDLs. The VLDLs are made and incorporate triglycerides on the inside with apolipoprotein B (apoB) on the outside. The degradation of apoB is reduced when fatty acid supply is increased. When apoB degradation is reduced, the excess apoB goes into the endoplasmic reticulum, which stresses the ER. Stressing the ER is thought to stimulate two enzymes that induce hepatic insulin resistance. Nomorua and Yamanouchi reported that ER stress may contribute to DNL, as well, since an ER stress reduction marker was shown to alleviate hepatic triglyceride levels and improve insulin activity. Insulin in the liver, meanwhile, activates an enzyme called insulin receptor kinase. Insulin receptor kinase phosphorylates insulin receptor substrate-1 (IRS-1) and IRS-2, which leads to the activation of two other enzymes – phosphatidylinositol 3-kinase (PI3K) and Akt2. These two enzymes stimulate glycogen synthesis and reduce gluconeogenesis (the production of glucose from macronutrients fat or protein). The whole effect is as if it’s a snowball rolling downhill growing bigger and more destructive. Insulin resistance increases glucose synthesis in the liver, which increases fasting glucose and insulin levels, which continues in an endless cycle unless regulated. In the end, all of these steps increase lipid accumulation in the liver, which is only the first step in the formation of fatty liver disease. Step two of fatty liver disease occurs when the liver is inflamed.12 Inflammation is caused by oxidative stress. Among other factors, some researchers have shown that increased fructose intakes cause bacterial overgrowth in the small intestine. The bacteria increase endotoxin (a toxin kept within a bacterial cell that is released only after the destruction of the cell wall) levels in the portal vein. This is believed to contribute to NAFLD because studies on mice show this situation was reduced by antibodies. Overall, it seems as if a reduction in fructose-sweetened beverages would address step one of NAFLD, but the understanding the mechanism of oxidative stress as it relates to NAFLD was still uncertain to these authors at that time. An earlier study conducted in Helsinki discovered that fat accumulation in the liver led to insulin resistance, but the men in this group weren’t obese and didn’t have type 2 diabetes.13 This study showed that men with relatively normal body weight, but with high liver fat content, were insulin resistant. This finding led to the thought that abdominal fat accumulation is not linked to insulin resistance, but rather insulin resistance is linked to upper body fat in general or liver fat. 6 Since the Helsinki study was conducted, researchers were further able to establish that insulin resistance was linked to fat accumulation in the liver. One study of nonalcoholic fatty liver disease found that protein kinase C epsilon worked to prevent insulin resistance in NAFLD.14 These researchers found the substrate linking fat in the liver with insulin resistance in that PKC epsilon activation was associated with insulin resistance. In this study, rats were fed a high-fat diet for three days to cause fat buildup in the liver and incite insulin resistance. Researchers found that preventing fat accumulation in the liver prevented the activation of PKC epsilon. They also gave rats antisense oligonucleotides (ASO) to stop the activation of PKC epsilon. They found ASO reduced PKC epsilon in the liver and white adipose tissue, but not in the muscles. The results showed this treatment didn’t reduce liver fat, but did lower plasma insulin by 50 percent and helped improve liver and adipose insulin action. Thus, they concluded, decreasing PKC epsilon activation protects against liver insulin resistance and improves adipose insulin action. The authors suggest PKC epsilon inhibition in humans may be a therapeutic tool for treating insulin resistance in the liver in patients with fatty liver disease and type 2 diabetes. An even more recent study found a link between the enzyme AMP-activated kinase and the accumulation of fat in the liver and the opposing effects of the enzyme AMP deaminase 2.15 The activity of AMPK is reduced in a fatty liver. Stimulating AMPK can prevent fatty liver buildup by stimulating fat oxidation and inhibiting lipogenesis. But AMPD2 activation inhibits AMPK activity in the liver. It appears these two enzymes regulate each other in that inhibiting AMPK activity leads to an increase in AMPD2 production, and vice versa. Not only that, but researchers found that dominant stimulation of AMPD2 compared to stimulation of AMPK led to fructose-induced fatty liver. This is because they showed that fructose engages AMPD2 rather than AMPK to cause fat accumulation. Recalling from the earlier discussion about how fructose uses up phosphates, as well as a substrate similar to ATP called GTP, and this reduction in phosphate levels stimulates AMPD2 production. Researchers also found that fructose-treated cells in the liver increased AMPK activity, but that AMPD2 limits the activity of AMPK. The sum of all this is that fructose led to fat accumulation in the liver, which leads to insulin resistance, which leads to type 2 diabetes. The study of AMPK and AMPD2 also found a connection with another condition related to excessive fructose intakes mentioned earlier, which was uric acid. The two conditions may be linked as elevated uric acids levels are often found in subjects with NAFLD. Not only can uric acid lead to gout and kidney stones, it is viewed as having a role (as is NAFLD) in the development of metabolic syndrome, a series of cardiovascular disease risk factors linked to obesity and type 2 diabetes, among other factors. Once again, fructose plays a significant role in the development of uric acid. As mentioned earlier, fructokinase phosphorylates fructose by using a phosphate from ATP to make fructose-1-phosphate. But fructokinase does not contain a feedback system to stop 7 it from continually phosphorylating fructose, a system that depletes ATP.16 With the consumption of ATP, AMP accumulates. This action stimulates AMP deaminase, which eventually results in uric acid production in the circulation. Uric acid levels can rise quickly after ingesting fructose and long-term fructose intake increases fasting levels of uric acid. Another report17 looked into how uric acid activates fructokinase in response to fructose ingestion in rats. The rats given a 15 percent fructose solution showed higher levels of fructokinase and to a lesser extent, aldolase (the second enzyme involved in phosphorylating fructose). This lead to the suggestion that fructose leads to the increase in fructokinase. Additionally, a control group was given fructose plus a xanthine oxidase inhibitor called allopurinol, which would reduce the production of uric acid. This study found that fructoseinduced regulation of fructokinase was prevented by allopurinol. This suggested to the authors that uric acid may regulate fructokinase in the liver. Similar experiments were conducted on human hepatocytes and the results showed that uric acid regulates fructokinase. Since fructose ingestion increases uric acid levels, which then stimulates fructokinase to metabolize more fructose, this leads to even more triglyceride production, a system seemingly spiraling out of control. But the drug allopurinol could put a stop to all of this by reducing excess uric acid levels in the blood. Given the body of knowledge on the effects of fructose and its link to nonalcoholic fatty liver disease and increased uric acid plasma levels, which lead to metabolic syndromes such as type 2 diabetes, it seems as if high fructose corn syrup should be outlawed. The American Diabetes Association reported this spring that total costs of diagnosed diabetes rose to $245 billion in 2012 from $174 billion in 2007.18 Of the $245 billion in costs, $176 billion was spent on direct medical costs and $69 billion was lost in reduced productivity. Seeing as how many Americans are concerned about the high costs of health care, addressing the impacts of fructosesweetened beverages and foods would be a good place to start. 8