The anterior tibial artery
advertisement

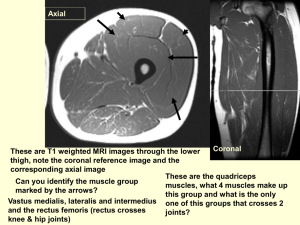
The Knee Joint • • • • • • Knee joint Largest joint in body. Very complex. Primarily a hinge joint. Tibia bears most of the weight. Consists of three articulations. Bones • Femur • Lateral & Medial Condyle. • Lateral & Medial Epicondyle. • Intercondylar Fossa. • Serves as the attachment point for the Gastrocnemius, Popliteus & 3 of the Quadriceps. Bones • Tibia- (Medial) • Medial & Lateral Condyle. • Intercondylar eminence. • Tibial Tuberosity. • Support most of the weight • Attachment point for all of the Quadriceps and all of the hamstrings (except Biceps Femoris) Bones • Fibula - (lateral) • Serves as the attachment for Biceps Femoris. • Does not articulate with femur or patella. • Not part of knee joint. • Acts as support for the Tibia Bones • Patella • Largest sesamoid (floating) bone. • Imbedded in quadriceps & patellar tendon • Serves as a pulley in improving angle of pull, resulting in knee extension. Movements • Flexion – bending or decreasing angle between femur & leg, characterized by heel moving toward buttocks • Extension – straightening or increasing angle between femur & lower leg Muscles • Quadriceps muscle group – extends knee – located in anterior compartment of thigh – consists of 4 muscles • Rectus Femoris- hip flex, knee extension • Vastus Lateralis- knee extension • Vastus Intermediusknee extension • Vastus Medialis- knee extension Quadriceps Muscles • Rectus Femoris (two-joint), Vastus Medialis, Vastus Intermedius, Vastus Lateralis (largest) • All attach to patella then to tibial tuberosity via patellar tendon • All superficial & palpable except Vastus Intermedius (under Rectus Femoris) • Strength & endurance is essential for maintenance of Patellofemoral stability • Generally desired to be 25% to 33% stronger than hamstring group Rectus Femoris Muscle Flexion of hip O. Anterior inferior iliac spine Extension of knee I. Tibial Tuberosity Vastus Lateralis Muscle Extension of knee O. Linea Aspera I. Tibial tuberosity via patellar tendon Vastus Intermedius Muscle Extension of knee O. Anterior Femur I. Tibial Tuberosity via patellar tendon Vastus Medialis Muscle Extension of knee O. Linea Aspera I. Tibial Tuberosity via Patellar tendon Knee Extension • Agonists – Rectus Femoris – Vastus Lateralis – Vastus Intermedius – Vastus Medialis Muscles • Hamstring muscle group – located in posterior compartment of thigh – responsible for knee flexion – consists of 3 muscles • Semitendinosus – extend hip, flex knee • Semimembranosus – extend hip, flex knee • Biceps Femoris – long head- extend hip, flex knee. Short head- flex knee Hamstring Muscles • • • • • • • Hamstring muscle strains very common “Running muscles” function in acceleration Antagonists to quadriceps muscles at knee Named for cordlike attachments at knee All originate on ischial tuberosity of pelvis Semitendinosus inserts on anteromedial tibia Semimembranosus inserts on posteromedial tibia • Biceps Femoris inserts on lateral tibial condyle & head of fibula Biceps Femoris Muscle Flexion of knee O. Long head-Ischial tuberosity Extension of hip O. Short headLateral lip Linea Aspera I. Head of Fibula Semitendinosus Muscle Flexion of knee Extension of hip Semimembranosus Muscle Flexion of knee Extension of hip Knee Flexion • Agonists – Biceps Femoris (Long & Short Head) – Semitendinosus – Semimembranosus Muscles • Gastrocnemius – Origin- posteriorly on medial & lateral femoral condyles – Insertion- posterior calcaneus – assist with knee flexion, ankle plantar flexion • Popliteus – Origin- lateral condyle of the femur – Insertion- posterior medial condyle of Tibia – assist medial hamstrings in knee internal rotation Popliteus Muscle Flexion of knee O. Lateral condyle of Femur I. Posteriorly on the medial Condyle of the Tibia Surface Anatomy Surface Anatomy Tendons vs Ligaments • Tendon: dense regular connective tissue that attaches muscle to bone. • Ligament: elastic dense regular connective tissue that attaches bone to bone. • Quadriceps tendon: – Formed by the tendons of four muscles. • Rectus Femoris • Vastus Lateralis • Vastus Medialis • Vastus Intermedialis – Inserts into patella QuickTime™ and a TIFF (Uncompressed) decompressor are needed to see this picture. • Patellar Ligament: – Distal part of quadriceps tendon. – Adjoins patella to tibial tuberosity. QuickTime™ and a TIFF (Uncompressed) decompressor are needed to see this picture. Patellar Ligament • Tibial Collateral Ligament (TCL): – Flat band – Medial epicodyle of femur to medial/superior condyle of tibia. • Fibular Collateral Ligament (FCL): – Cord-like – Lateral epicondyle of femur to lateral surface of head of fibula. QuickTime™ and a TIFF (Uncompressed) decompressor are needed to see this picture. • Anterior Cruciate Ligament (ACL): – Weakest of the two – Anterior intercondylar of tibia to posterior/medial lateral condyle of femur. – Prevents poserior displacement of femur & hyperextension of the knee. • Posterior Cruciate Ligament (PCL): – Posterior intercondylar of tibia to anterior/lateral of medial condyle of femur. – Prevents anterior displacement of femur and hyper flexion of knee. QuickTime™ and a TIFF (Uncompressed) decompressor are needed to see this picture. • Arcuate Popliteal Ligament: – Posterior fibular head – Spreads over surface of posterior knee joint. – Reinforces joint capsule posteriorly. • Oblique Popliteal Ligament: – Part of semimembranosus tendon. – Strengthens joint capsule posteriorly. QuickTime™ and a TIFF (Uncompressed) decompressor are needed to see this picture. • Transverse Ligament: – Slender fibrous ban – Joins menisci for movement QuickTime™ and a TIFF (Uncompressed) decompressor are needed to see this picture. Bursae • Flattened fibrous sacs • Fluid filled • Occur where ligaments, muscles, skin, tendons or bones rub together. QuickTime™ and a TIFF (Uncompressed) decompressor are needed to see this picture. •Suprapatellar: -Anterior femur and deep quadriceps femoris. -Movement of quadriceps tendon over femur. •Patella: Suprapatellar Bursa -Patella and Skin -Movement of skin over patella. •Deep Infrapatella: -Upper part of tibia and patellar ligament. -Movement of patellar ligament over tibia. •Subcutaneous Infrapetallar: -Patellar ligament and skin -Movement of skin Patella Bursa QuickTime™ and a TIFF (Uncompressed) decompressor are needed to see this picture. Deep Infrapatellar Bursa Subcutaneous Infrapatellar Bursa Cartilage • Medial Meniscus: – C-Shaped – Anterior horn attaches to anterior intercondylar of tibia, anterior to ACL. – Posterior horn attaches to posterior intercondylar, anterior to PCL. – Adheres to tibial collateral ligament. • Lateral Meniscus: – Circular – Smaller & moves easily – Adheres to popliteus tendon. QuickTime™ and a TIFF (Uncompressed) decompressor are needed to see this picture. Torn Meniscus – Either or both menisci may be torn in several different areas from a variety of mechanisms, resulting in varying degrees of problems – A torn meniscus is one of the most common knee injuries. Any activity that causes you to forcefully twist or rotate your knee, especially when putting the pressure of your full weight on it, can lead to a torn meniscus. – Conservative treatment — such as rest, ice and medication — is sometimes enough to relieve the pain of a torn meniscus and give the injury time to heal on its own. In other cases, however, a torn meniscus requires surgical repair. Torn ACL • • • • • • • • Torn Anterior Cruciate Ligament (Torn ACL) Facts The anterior cruciate ligament (ACL) is one of four ligaments that help stabilize the knee. It is the most commonly injured knee ligament. ACL injury usually occurs when the knee is hyperextended (straightened) and a pivot occurs simultaneously. The injury may occur with or without contact. Women have an increased risk of ACL injury because of differences in anatomy, muscle mass, and training. Symptoms of ACL tear include hearing a loud pop as the ligament tears, pain, knee swelling, and difficulty walking. Diagnosis is made clinically by physical examination and usually confirmed by MRI. Surgery and rehabilitation is the most commonly suggested treatment, though in patients who are sedentary or do little sports activity, a nonoperative approach is a possibility. Postoperative rehabilitation may take six to nine months to return to full activity. From http://www.emedicinehealth.com/torn_acl/article_em.htm Nerves - Posterior FEMORAL L2, L3, L4 • • The femoral nerve arises from the 2nd, 3rd, & 4th lumbar nerves. The nerve emerges from the from the lateral border of the psoas major and innervates the iliacus and passes deep into the inguinal ligament of the anterior thigh supplying the flexors of the hip and extensors of the knee. Innervates: Rectus Femoris, Vastas intermedialis, Vastas lateralis, Vastas medialis, Nerves Sciatic Nerve • The sciatic nerve is the largest nerve in the body and is in continuation of the main part of the sacral plexus L4-S3. Descends deep into the biceps femoris; bifurcates into the tibial and common fibular nerves at apex of popliteal fossa. • The tibial nerve is the larger of the two terminal branches of the sciatic nerve. Its runs through the popliteal fossa with the popliteal artery and vein. The nerve supplies all muscles in the posterior compartment of the leg. Tibial Nerve Nerves - Anterior • • The superficial fibular (peroneal) nerve is one of the terminal branches of the common fibular nerve. It descends anterior to the fibula. It supplies the fibularis longus and brevis (and sometimes the extensor digitorum brevis) and provides cutaneous branches to usually all five toes. Section of the superficial fibular nerve may result in impairment and loss of eversion. The deep fibular (peroneal) nerve is one of the terminal branches of the common fibular nerve. It continues around the neck of the fibula and descends on the interosseous membrane in company with the anterior tibial artery. It supplies the tibialis anterior, extensor digitorum longus, extensor hallucis longus, fibularis tertius, and extensor digitorum brevis muscles, and it gives off dorsal digital nerves to the first two toes. Damage to the deep fibular nerve may result in footdrop and a "steppage" gait, owing to paralysis of the dorsiflexors of the foot and the extensors of the toes. This gait is characterized by lifting the knee high in order to allow the drooping toes to clear the floor. Right anterior view of knee Superficial fibular Nerve Deep Fibular (peroneal) Nerve Sciatic Nerve • The largest and longest nerve in the body. The sciatic nerve leaves the pelvis via the greater sciatic notch, descends deep to the gluteus maximus muscle, and continues down the posterior aspect of the thigh. There it supplies the hamstring muscles and part of the adductor magnus. The sciatic nerve divides immediately above the knee to give rise to the peroneal nerve and tibial nerve. • The sciatic nerve innervates the skin on the posterior aspect of the thigh and gluteal regions, as well as the entire lower leg (except for its medial aspect). • Muscles it innervates: Rectus femoris, vastas intermedialis, vastas lateralis, vastas medialis. Arteries Femoral Artery • • • The femoral artery is first known as the common femoral artery, because it has not yet given off branches. It gives off a branch known as the deep artery of the thigh (profunda femoris) while continuing down the thigh medial to the femur. After giving off other branches, the femoral artery goes behind the knee and becomes the popliteal artery. The popliteal artery is the extension of the "superficial" femoral artery after passing through the adductor canal and adductor hiatus above the knee. The termination of the popliteal artery is its bifurcation into the anterior tibial artery and posterior tibial artery. The popliteal artery supplies blood to the knee joint and muscles in the thigh and calf. It is accompanied, along its length, by the popliteal vein. The posterior Tibial Artery of the lower limb carries blood to the posterior compartment of the leg and plantar surface of the foot, from the popliteal artery. It is accompanied by a deep vein, the posterior tibial vein, along its course. Right Knee Anterior View Popliteal Artery Posterior Tibial Artery Anterior Tibial Artery Arteries • The anterior tibial artery branches off from the popliteal artery just below the knee area. The anterior tibial artery supplies vital oxygenated blood and nutrients to the anterior shin or lower leg area. Blood flows from the common iliac artery to the external iliac artery, the femoral artery, the popliteal artery, and finally the anterior tibial artery. • Dorsalis Pedis artery (dorsal artery of foot), it carries oxygenated blood from the dorsal surface of the foot. It arises at the anterior aspect of the ankle joint and is a continuation of the anterior tibial artery. Along its course, it is accompanied by the dorsalis pedis vein. Arteries Tibial Nerve Posterior tibial artery Artery • The fibular artery (also known as the peroneal artery) supplies blood to the lateral compartment of the leg and is typically a branch of posterior tibial artery. Inferior gluteal artery • • • The inferior gluteal artery (sciatic artery), the larger of the two terminal branches of the anterior trunk of the internal iliac artery, is distributed chiefly to the buttock and back of the thigh. It passes down on the sacral plexus of nerves and the Piriformis, behind the internal pudendal artery, to the lower part of the greater sciatic foramen, through which it escapes from the pelvis between the Piriformis and Coccygeus. It then descends in the interval between the greater trochanter of the femur and tuberosity of the ischium, accompanied by the sciatic and posterior femoral cutaneous nerves, and covered by the Glutæus maximus, and is continued down the back of the thigh, supplying the skin, and anastomosing with branches of the perforating arteries. Lateral and Medial circumflex femoral arteries • Lateral circumflex femoral artery The lateral femoral circumflex artery arises from the lateral side of the profunda femoris artery, passes horizontally between the divisions of the femoral nerve, and behind the sartoriusand rectus femoris, and divides into ascending, transverse, and descending branches. Innervates: Rectus femoris, Vastas intermedialis, Vastas lateralis, Vastas medialis. • Medial circumflex femoral artery The medial femoral circumflex artery arises from the medial and posterior aspect of the profunda femoris artery, and winds around the medial side of the femur, passing first between the pectineus and iliopsoas muscles, and then between the obturator externus and the adductor brevis muscles. - helps supply blood to the neck of the femur Veins . The anterior tibial vein of the lower limb carries blood from the anterior compartment of the leg to the popliteal vein which is forms when it joins with the posterior tibial vein. Like most deep veins, the anterior tibial vein is accompanied by an artery of the same name, the anterior tibial artery, along its course. • The Popliteal vein is formed at the distal border of the popliteus as a continuation of the posterior tibial veins. The vein lies superficial to the fibrous sheath as the popliteal artery. Superiorly, the popliteal vein becomes the femoral vein. The femoral vein is the continuation of the popliteal vein. The vein lies posterior to the femoral artery. Eventually the femoral vein becomes the external illiac vein. • Veins • Posterior tibial vein of the lower limb carries blood from the posterior compartment and plantar surface of the foot to the popliteal vein which it forms when it joins with the anterior tibial vein. Like most deep veins, the posterior tibial vein is accompanied by an artery of the same name, the posterior tibial artery, along its course. • Fibular (Peroneal) vein The fibular veins are deep veins that help carry blood from the lateral compartment of the leg. They drain into the posterior tibial veins, which will in turn drain into the popliteal vein. The fibular veins accompany the fibular artery. Greater and lesser saphenous veins • Lesser saphenous vein originates where the dorsal vein from the fifth digit merges with the dorsal venous arch of the foot, which attaches to the great saphenous vein. The vein and is subcutaneous (just under the skin). From its origin, it courses around the lateral aspect of the foot and runs along the posterior aspect of the leg, passes between the heads of the gastrocnemius muscle, and drains into the popliteal vein, approximately at or above the level of the knee joint. • Greater saphenous vein originates from where the dorsal vein of the first digit merges with the dorsal venous arch of the foot. After passing anterior to the medial malleolus (where it often can be visualized and palpated), it runs up the medial side of the leg. At the knee, it runs over the posterior border of the medial epicondyle of the femur bone. The great saphenous vein then courses medially to lie on the anterior surface of the thigh before entering an opening in the fascia lata called the saphenous opening. It joins with the femoral vein in the region of the femoral triangle at the saphenofemoral junction. References • http://medchrome.com/wp-content/uploads/2010/06/ligamentsof-knee.jpg • http://www.hughston.com/hha/a.extmech.htm • http://classroom.sdmesa.net/eschmid/F07.11.L.150.jpg • http://www.gla.ac.uk/ibls/US/fab/tutorial/anatomy/kneet.html • http://www.riversideonline.com/health_reference/DiseaseConditions/DS01031.cfm • Wikipedia • Essential Clinical Anatomy 4th edition. Wolters Kluwer • http://www.genericlook.com/anatomy/Lower-Extremity-Veins/