CSA12-2011
advertisement

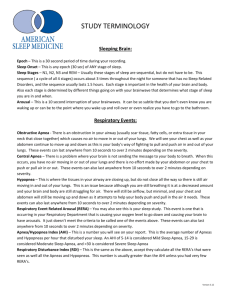
CENTRAL SLEEP APNEA/ HYPOVENTILLATION SYNDROME By Mohamed EL gamal Assistant Lecturer of chest medicine CENTRAL SLEEP APNEA • Def: central apnea occurs when both airflow and ventilatory effort are absent. at least 10 seconds or more .Previously used terms include diaphragmatic apnea or arrhythmic apnea (Iber et al., 2007). • central apnea and hypoventilation syndromes together they have many similar aspects of pathophysiology and treatment. • The central sleep apnea (CSA) syndromes include a diverse group of disorders associated with the presence of central apnea during sleep In some of the disorders the patients have primarily nocturnal hypoventilation (increased arterial partial pressure of carbon dioxide [PaCO2]) due to inadequate tidal volume and/or respiratory rate with relatively few discrete central apneas. • Demographics • CSA is estimated to represent about 5% to 10% of patients with sleep-related breathing disorders. • CSA also accounts for up to 12% of adult patients with insomnia. • Prevalence of CSA is greater among men • and increases adults. in middle-aged and older • CSA can result from a failure of ventilatory drive (idiopathic form) or may be due to secondary causes such as CHF or neurologic disorders. • The idiopathic form is less common than secondary causes. • Central apneas can also occur during sleep-onset in otherwise healthy individuals and during sleep at high altitude. • Pathophysiology of Central Sleep Apnea During the waking state respiration is controlled by three processes, Metabolic (automatic) Wake-related drive to breathe and Behavioral (voluntary) systems. During NREM sleep, the wake-related drive to breathe and behavioral control systems are abolished, and respiration is controlled entirely by the metabolic control system, primarily by the hypercapnic ventilatory drive (ie, ventilation is stimulated by hypercapnia) and to a lesser degree by the hypoxic ventilatory drive (ie, ventilation is stimulated by hypoxia). A PaCO2 above the apneic threshold stimulates ventilation, whereas a PaCO2 below this threshold leads to a central apnea that continues until PaCO2 increases and once again exceeds the apneic threshold. Metabolic Consists of chemoreceptors for hypoxia (carotid body) and hypercapnia (carotid body and medulla) as well as brainstem systems that regulate ventilation to maintain stable levels of pH, PaO2 and PaCO2 Risk Factors • High CO2 ventilatory drive • Sleep disturbance: Increased frequency of sleep-wake transitions • Gender: Men are more likely to have central apneas due to a higher hypocapnic apneic threshold during NREM sleep. The lower apneic threshold in women than in men could be mediated by both female and male hormones • Age: Central apneas are more common in older adults due to the increased prevalence of underlying medical disorders (eg, CHF), neurologic disorders, or greater sleep disturbance and awakenings • Altitude: Central apneas can developacutely following ascent to high altitudes • Heart failure Stroke, hypothyroidism , acromegaly , renal failure , methadone ttt Clinical Features • • • • • • • • asymptomatic Excessive sleepiness Insomnia Sleep disturbance with repeated nocturnal awakenings Nocturnal sensation of dyspnea Morning headaches Inattention Poor concentration Associated features • Nocturnal hypoxemia and hypercapnia • • • • Cardiovascular disorders Systemic hypertension Pulmonary hypertension,Cor pulmonale Cardiac arrhythmias (sinus arrhythmia [with bradycardia occurring at apnea termination], bradycardia, sinus arrest, premature ventricular contractions, or ventricular tachycardia) • • • • Polycythemia Depression Cognitive impairment Impotence Diagnosis: • Primary CSA exists when symptoms or signs of disturbed sleep are accompanied by more than five central apneas plus hypopneas per hour of sleep, and normocarbia during wakefulness (Iber et al., 2007). • Secondary CSAS requires frequent central apneas that are attributable to a medical condition, such as heart failure. (AASM, 2005). Polysomnographic features of central apneas • Pauses in respiration and absent ventilatory effort lasting 10 seconds or longer • Loss of chest and abdominal movement ( respiratory inductance plethysmography) • No electromyographic (EMG) activity of the respiratory muscles including diaphragm • No change in intrathoracic (esophageal balloon) pressures • Associated with oxygen desaturation (generally mild) and, occasionally, arousals • In patients with obstructive, central and mixed apneas, at least 50% of the respiratory events are central in nature • At least five central apneas per hour of sleep • Snoring may occur (less obstructive sleep apnea) prominent Changes in sleep architecture • Increased NREM stages 1 and 2 sleep • Decreased NREM stages 3 and 4 sleep than in • False Classification of Apneas as Central • Even with RIP, an obstructive apnea may appear to be a central apnea. • The RIP rib cage and abdominal band tracings are nearly flat but persistent respiratory effort is definitely noted in the esophageal pressure tracing. In central hypopnea, the flow falls in proportion to the respiratory effort. The airflow profile shows a round contour. In obstructive hypopnea, there is evidence of airflow limitation (flat airflow shape) and flow falls even though respiratory effort stays the same or increases. In mixed hypopnea, there is a fall in respiratory effort but the fall in flow is proportionately greater and there is evidence of airflow limitation • Central sleep apnea can be classified based on: • 1.Underlying level of ventilation hypercapnic or non-hypercapnic • 2. Idiopathic or Secondary Hypercapnic Associated with daytime hypoventilation (high waking PaCO2) Diminished response to hypercapnia Hypoventilation continues during sleep. Includes patients with 1. Won’t breathe A. Central hypoventilation • Congenital central hypoventilation syndrome • Idiopathic central hypoventilation syndrome • Brain tumors, cerebrovascular disease • Structural brain disorders—Chiari’s syndrome • Apnea of infancy B. Medication-induced central sleep apnea (narcotics/opiates) • Central sleep apnea with normal or increased daytime PCO2 • Complex sleep apnea (treatment emergent or persistent central sleep apnea) C. Obesity hypoventilation syndrome 2. “Can’t Breathe” • A. Restrictive thoracic cage disorders • B. Neuromuscular disorders i.Motor neurone disease including poliomyelitis ii.Neuropathy iii.Neuromuscular junction disorders (myasthenia gravis) iv.Myopathy (muscular dystrophy) Nonhypercapnic • Not associated with daytime hypoventilation (normal or low waking PaCO2) • Increased ventilatory response to hypercapnia • PaCO2 levels increase during sleep; brief arousals are accompanied by a hyperventilatory “overshoot” that decreases PaCO2 levels below the apneic threshold and leads to central apneas Includes patients with: 1- Idiopathic CSA 2- Post-arousal CSA. 3- Congestive Heart Failure 4- Sleep At High Altitude 5-Complex sleep apnea persistent sleep apnea) (treatment emergent or .The International Classification of Sleep Disorders, 2nd edition (ICSD-2) lists five CSA syndromes:• 1. Primary central sleep apnea • 2. Cheyne-Stokes breathing pattern • 3. High-altitude periodic breathing • 4.Central sleep apnea due to drug or substance • 5. Primary sleep apnea of infancy • Etiology Medical disorders Congestive heart failure Endocrine disorders (eg diabetes mellitus, acromegaly, or myxedema) Nasal obstruction, Neurologic disorders • Autonomic dysfunction Parkinson disease, Shy-Drager syndrome, or diabetes mellitus) • Brainstem (medulla) tumors, infarctions, or hemorrhage • Encephalitis, Head injury, Amyotrophic lateral sclerosis • Neuromuscular diseases (myasthenia gravis, myopathy) • Poliomyelitis and postpolio syndrome • Stroke Miscellaneous • At sleep onset • Following therapy of OSA with CPAP or tracheotomy • After ascent to high altitude • Medication use (eg, opiates) Cheyne Stokes breathing-central sleep apnea CSB occurs most commonly in patients with left ventricular systolic dysfunction but also can occur in patients with diastolic CHF or neurologic disorders. The mechanism: Instability of the control of ventilation long circulation time, lower daytime and sleeprelated PaCO2 levels (< 45 mm Hg), Greater hypercapnic respiratory drive (leading to an “overshoot” of ventilation, as well as a fall in PaCO2 below the apneic threshold) In patients with CHF, hyperventilation can also arise from stimulation of pulmonary vagal receptors by pulmonary congestion • Cycle length is related inversely to cardiac output, and directly to circulation time. • There is typically also a delay in the nadir of oxygen desaturation following the apneic events. • Arousals, if frequent, result in sleep fragmentation, insomnia, or daytime sleepiness. Patients may also report nocturnal episodes of dyspnea. • The development of CSR in patients with CHF is correlated with ejection fraction and is associated with a worse prognosis (ie, increased risk of death and higher frequency of transplantation). • Males are affected more commonly than women • In addition to CHF in which CSR can be seen in up to 40% to 50% of patients • CSR can also be caused by neurologic disorders (eg, prevalence of about 10% in strokes), renal failure, or occur in an idiopathic form without any identifiable underlying cause. AASM score Cheyne-Stokes Respiration • if there are at least 3 consecutive cycleal crescendo-decrescendo change in breathing amplitude and at least one of the following: • – Five or more central apneas or hypopneas / hour sleep. – The cyclic crescendo-decrescendo change in breathing amplitude has duration of at least 10 cosequtive minutes. – Note that Cheyne-Stokes breathing has varible cycle length that is most commonly in the range of 60 seconds. the majority of patients do not complain of subjective excessive daytime sleepiness. During PSG, CSR generally occurs during the transition from wakefulness to sleep and during NREM stages 1 and 2 sleep. It attenuates or resolves during NREM stages 3 and 4 sleep and REM sleep During a subsequent PAP titration, pure CSB-CSA may emerge when upper airway obstruction is eliminated Therapy: • Optimize medical management • Supplemental oxygen • CPAP (effective in ~40–50%) • BPAP with backup rate (BPAP-ST) • ASV • Transplant Sleep-Onset Central Apneas • repetitive episodes of central apneas may occur if PaCO2 fluctuates above or below the apneic threshold. • Sleep-onset central apneas are generally transient, disappearing once stable sleep is attained • Frequency of central apneas is normally less than five episodes per hour of sleep. • Repetitive sleep onset central apneas can result in sleep-initiation insomnia Periodic Breathing Secondary to High Altitude • Periodic breathing, or cycles of central apneas and hyperpneas, can occur on ascent to high altitude (usually > 4000 to 7600 meters). • Severity of symptoms is influenced by elevation, speed of ascent, and individual predisposition. Persons with increased hypoxic ventilatory chemoresponsiveness appear to have a greater risk for developing high-altitude–related periodic breathing. • Men may be affected more commonly than women. Polysomnographic features altitude periodic breathing of high- Repetitive central apneas 10 seconds or longer in duration occurring about every 12 to 34 seconds primarily during NREM sleep • Can be associated with oxygen desaturation • Can result in arousals • Respiration is more regular during REM sleep Sleep architecture • No change in total sleep time • Increased frequency of arousals • Increased NREM stages 1 and 2 sleep Therapy • consists of either oxygen therapy or administration of acetazolamide (250 mg /6h) reduce central apnea over 1-2 weeks Central Sleep Apnea Related to Medication Use • Central apneas can develop during administration of opiate drugs. Aside from central apneas, other respiratory pattern abnormalities, such as • periodic breathing, • Biot respiration, and • obstructive hypoventilation, can develop due to receptor-related depression of the hypercapnic ventilatory drive and increase in hypoxic ventilatory drive. CompSA is defined as a form of CSA identified by the persistence or emergence of central sleep apneas or hypopneas upon exposure to CPAP or BPAP without a backup rate when obstructive events have disappeared. These patients have predominantly obstructive or mixed apneas during the diagnostic portion of the study occurring 5/hr or more. CAUSES An elevated loop gain in combination with a narrow upper airway Activation of Hering-Bruer reflex by increased lung volume on CPAP produces prolonged expiration to the point of central apnea in some patient Maladaptation to the device,with frequent arousals causing hyperventilation and sleep onset apnea • Hypoventilation in Adults • Hypoventilation during wakefulness is usually defined as an arterial partial pressure of carbon dioxide (PaCO2) equal to or greater than 45 mm Hg. • During sleep, there may be periods of time in which the SpO2 is reduced without associated events that meet criteria for apnea or hypopnea. • Hypoventilation Rule (AASM Scoring Manual ) • Score hypoventilation during sleep if there is a ≥10 mm Hg increase in PaCO2 during sleep in comparison with an awake supine value. The ICSD-2 lists five categories Hypoventilation Syndromes of Sleep 1. Sleep-related non obstructive alveolar hypoventilation, Idiopathic Rare, usually case reports 2. Congenital central alveolar hypoventilation syndrome Example: Central congenital hypoventilation syndrome 3. Sleep-related hypoventilation due to medical condition A. Sleep-related hypoventilaton/hypoxemia due to lower airways obstruction Examples: Hypercapnic COPD, bronchiectasis, or cystic fibrosis B. Sleep-related hypoxemia due to pulmonary parenchymal or vascular pathology Example: Sleep-related hypoventilation with idiopathic pulmonary fibrosis or other interstitial lung diseases or pulmonary vascular disease associated with end-stage lung disease C. Sleep-related hypoventilation/hypoxemia due to neuromuscular and chest wall disorders Examples: Obesity hypoventilation syndrome, neuromuscular disease, kyphoscoliosis Treatment Summary 1-Central apnea due to hyperventilation • CPAP • Bilevel positive airway pressure (BIPAP) with a set backup respiratory rate • Adaptive servo-ventilation (ASV) • SUPPLEMENTAL OXYGEN • SUPPLEMENTAL CARBON DIOXIDE • Hypnotic 2-Central apnea due to hypoventilation • • NIPPV PHARMACOLOGIC THERAPY HOME MESSAGES Distinguishing central sleep apnea from obstructive sleep apnea may be difficult. Central apneas can also occur during sleep-onset in otherwise healthy individuals Central apneas one cause of insomnia CSA classification Cardiac pt + symptoms of sleep disturbance >>>>> CSA Central apnea and hypoventilation syndromes together they have many similar aspects of pathophysiology and treatment When prescribe CPAP we must assess clinicaly and by PSG The best ttt is >>>> ASV then BIPAP with back up rate But you can give CPAP with strict follow up Thank you