Practical Considerations for Design and Analysis of Thorough QT
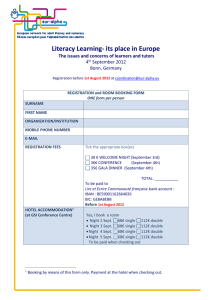
advertisement

Practical Issues to Consider:
Design and Analysis of Thorough
QT/QTc Study
Venkat Sethuraman
FDA/Industry Workshop, 14-16 Sept., 2005
Outline
Introduction
ICH E14; QT correction methods
Study Design Considerations
Choice of Baseline; positive control; # of ECG replicates
Crossover versus Parallel group
Disease specific Considerations
Hypotheses & Sample Size
Analysis
Central Tendency & Categorical Analysis
Summary of issues/resolutions
2 V Sethuraman/FDA-Industry Workshop/14-16 Sept., 2005
Background – QT interval
QT Correction: QT and RR
are correlated so a need for
correction.
QTcP =QT/RRb
bi
QTc
50 i =QT
60 i/RR
70 i
80
340
Individual Correction:
380
Pooled correction:
420
HR = (60/RR), with RR in sec
QTcB =QT/RR0.5
40
Model: QT= 535.57 -2.44 * HR
460
Bazett’s correction:
QT (msec)
380
340
F:Placebo
0.33
QTcF = QT/RR
Model: QT= 540.95 -2.44 * HR
420
460
E:Moxifloxaxin
400mg
Fridericia’s
correction:
90
HR (bpm)
100
40
50
60
70
HR (bpm)
80
90
QTcF & QTci are generally preferred correction for ‘thorough’ QT study.
3 V Sethuraman/FDA-Industry Workshop/14-16 Sept., 2005
100
Background - Impact on Type I Error (Simulation)
5
10
1.0
0.8
5
10
H R c hange
5
10
H R c hange
1.0
0.6
0.8
Assume QTcB is
the true QT-RR
relationship
0.0
0.2
0.4
Type I error
0.8
0.6
0.4
0.2
0.0
H R c hange
0
Mixed Model
1.0
Individual Data-driven
5
0.6
0.2
0.0
0
H R c hange
0
0.4
Type I error
0.8
0.6
0.0
0.2
0.4
Type I error
0.8
0.6
0.4
0.0
0.2
Type I error
0
Type I error
Pooled Data-driven
1.0
Fridericia
1.0
Bazett
10
4 V Sethuraman/FDA-Industry Workshop/14-16 Sept., 2005
0
5
H R c hange
10
Background
ICH E14 – Step 4 (25May2005): “a negative ‘thorough QT/QTc study’ is one
in which the upper bound of the 95% one-sided confidence interval for the
largest time-matched mean effect of the drug on the QTc interval excludes
10 ms.”
Timing of ‘thorough’ QT study is usually flexible but required for all new
products.
This study plays a critical role in determining the intensity of ECG data
collection during later stages of drug development.
Usually conducted in healthy volunteers but in some instances cannot be
conducted due to safety or tolerability concerns (e.g., cytotoxic cancer
drugs).
ECGs should be manually read. Readers should be blinded to time,
treatment and subject (one reader should read all the ECG recordings from
a given subject).
Cost can be anywhere between $60-100/ECG.
5 V Sethuraman/FDA-Industry Workshop/14-16 Sept., 2005
Study Design Consideration
Placebo-controlled study in normal healthy volunteers with a
positive control.
Parallel versus Crossover Designs
Crossover: smaller numbers of subjects; Facilitate QT correction
Parallel Group: long half-life drugs; multiple dose
Randomization & Blinding
Thorough study should it be handled in a same manner as any other
pivotal trial.
Moxifloxacin visits should not be un-blinded (or single-blind) while keeping
all other treatments blinded. This may induce HR differences or cause
“habituation effects”.
A crossover study should be period-balanced in all treatments. Do not
randomize subjects to receive Moxifloxacin in the first period and in
subsequent periods randomized to active treatments.
In a parallel group, it is not required to have all subjects receive
Moxifloxacin prior to being randomized to active treatments
6 V Sethuraman/FDA-Industry Workshop/14-16 Sept., 2005
Study Design Consideration
Crossover Design Example
4-period Williams’ design with Active (therapeutic & supra-therapeutic
dose), placebo and positive control.
If active drug is administered under repeat dose conditions (say 5 days of
dosing) then, the positive control can be 4 days of placebo + 1 day of
moxifloxacin 400 mg.
Adequate washout between treatment groups (say at least 1 week)
Sample size usually ~50 subjects
Parallel Group
Subjects randomized to one of 4 treatments
Baseline: recommended to have a 0-24 hr profile with time-match for
post-dose
Sample size usually >~60 / arm
Adequate ECG sampling around tmax of active drugs.
Appropriate to consider at least 3 replicate ECG’s at each time point
7 V Sethuraman/FDA-Industry Workshop/14-16 Sept., 2005
Endpoint: Change from Baseline QTc
Baseline definition:
Time-matched: Baseline for each session (or
treatment) is the avg. of values at a time point (on
baseline day) corresponding to the post-dose time
point.
Pre-dose averaged: Baseline for each session (or
treatment) is the average of pre-dose values (~1hr prior
to dosing).
Time-averaged: Baseline for each session (or
treatment) is the average of all values on baseline day.
8 V Sethuraman/FDA-Industry Workshop/14-16 Sept., 2005
Endpoint: Change from Baseline QTc
Figure obtained from > Cornel Pater., Methodological considerations in the design of trials for safety assessment of
new drugs and chemical entities Current Controlled Trials in Cardiovascular Medicine 2005, 6:1
9 V Sethuraman/FDA-Industry Workshop/14-16 Sept., 2005
Study Design Consideration
Choice of Positive Control
Moxifloxacin 400 mg (single dose) is usually used as a positive control
Any other positive control? quinolones like, gatifloxacin, etc.
Effect of Moxifloxacin: The positive control should have an effect on the mean
QT/QTc interval of about 5 ms (i.e., an effect that is close to the QT/QTc effect that
represents the threshold of regulatory concern, around 5 ms). Detecting the positive
control’s effect will establish the ability of the study to detect such an effect of the study
drug. Absence of a positive control should be justified and alternative methods to
establish assay sensitivity provided.
Factors that affect the estimation of Moxifloxacin Effect
effects similar for Time-matched, time averaged or pre-dose averaged baseline ?
the upper bound of the 95% one-sided confidence interval for the largest timematched mean effect of the moxi relative to placebo OR Max. mean QTc effect of
Moxi (unadjusted for placebo)?
Effects using QTci tends to be smaller than QTcF or QTcB.
10 V Sethuraman/FDA-Industry Workshop/14-16 Sept., 2005
Impact of Positive Control
– Positive control shows >5ms effect (say QTcF) and active
treatment shows or does not show effect
– Outcome: the study results are valid.
– If effect of Moxi>12-15ms, are the study results still valid?
– depends on subject population, correction method, baseline,
days of separation from baseline to post-dose, etc.
– Positive control shows <5 ms effect
– If active treatment shows no effect, then it is a “failed” study or
need to show alternate means of establishing assay sensitivity.
If active treatment shows a positive effect (say >15ms), does the
effect of study drug still valid?
11 V Sethuraman/FDA-Industry Workshop/14-16 Sept., 2005
Treatment Estimates from Crossover
Baseline
Method
Trt (QTci)
Point
Estimate*
90% CI
Time-avg.
Placebo
-5
(-7, -2.7)
Moxi
3.5
(1.3, 5.7)
Moxi-Placebo
8.5
(7.6, 9.3)
Placebo
-5.8
(-8.9, -2.8)
Moxi
6.8
(3.8, 9.8)
Moxi-Placebo
12.6
(9.7, 15.6)
Placebo
-3.8
(-5.6, -2.1)
Moxi
5.0
(3.3, 6.8)
Moxi-Placebo
8.8
(8.0, 9.7)
Time-match
(occurred at 1hr)
Pre-dose avg.
* Arth. Mean or LS mean difference
12 V Sethuraman/FDA-Industry Workshop/14-16 Sept., 2005
Categorical Results
Increase in QTc> 30, 60 msec
Categorical results might be affected if a diurnal variation
in QTc is ignored.
Time-matched
Time-averaged
/pre-dose avg.
Category
CFB QTc >30 ms
Placebo
<1%
Moxi
3.5%
Placebo
0%
Moxi
0%
*Subjects were included if they had both baseline and post-dose
measurements; ECG values at a time point was an average of 3 replicate
measurement.
13 V Sethuraman/FDA-Industry Workshop/14-16 Sept., 2005
Moxifloxacin Treatment Estimates Published
Parameter
Comparison
Point Estimate
90% or 95% CI
QTcF1 *
Moxifloxacin 400 mg
13.9 (SD=15)
QTcF2 *
Moxi 400mg – Placebo
12.7
(8.6, 16.8)
QTci2 *
Moxi 400mg – Placebo
11.1
(7.2, 15)
QTcF3 ^
Moxi 400mg – Placebo
8
(6, 9)
QTci3 ^
Moxi 400mg – Placebo
7
(5, 8)
QTcF4 +
Moxi 400mg – Placebo
11,
12,
16
(7, 14)
(8, 17)
(12, 21)
1: Moxifloxacin SBA: Mean (SD) change from baseline QTc at Cmax using corresponding time on
Placebo Day as baseline
2 . Alfuzosin QT study, and 3. Vardenafil QT study
http://www.fda.gov/ohrms/dockets/ac/03/briefing/3956B1_01_FDA-alfuzosin.htm
4. Vesicare QT study: http://www.vesicare.com/pdf/vesicare_prescribing_info.pdf
14 V Sethuraman/FDA-Industry Workshop/14-16 Sept., 2005
415
410
405
Baseline QTci by Period
420
425
Baseline Differences in a Crossover (An Example)
400
Period 1
Period 2
Period 3
0
5
10
15
Time(hrs)
15 V Sethuraman/FDA-Industry Workshop/14-16 Sept., 2005
20
Impact of Baseline on QT correction
Pre-dose data used for QT correction
3 pre-dose per period x 3-period
Estimates of QT correction may be unreliable
Difference can be as high as 40-50 ms for some subjects
Pre-dose + placebo treatment (crossover only)
All pre-dose + 12 post-dose time points (placebo)
Assume that placebo occurs equal number of times/period
Estimates could be different for placebo on period 3 (?)
Baseline day profile (0-24 hr)
All 12 baseline time points (each 3 ECG/time point)
16 V Sethuraman/FDA-Industry Workshop/14-16 Sept., 2005
1200
1400
500
300
600
800
1400
600
800
1000
1200
1400
800
1000
1200
1400
600
1400
1000
1200
1400
1200
1400
500
QT(ms)
500
300
300
RR(ms)
1200
1400
RR(ms)
400
QT(ms)
500
400
1000
800
RR(ms)
300
800
1200
300
600
RR(ms)
600
1000
500
QT(ms)
500
300
600
800
RR(ms)
400
QT(ms)
400
300
QT(ms)
1200
RR(ms)
500
RR(ms)
1000
400
1000
400
800
400
QT(ms)
300
400
QT(ms)
400
300
QT(ms)
600
QT(ms)
Pre-dose + placebo
500
Pre-dose
500
Time-match
600
800
1000
RR(ms)
1200
1400
600
800
1000
RR(ms)
Impact on QT Correction Method
50
Percent of Total
40
30
20
10
0
-50
0
QTci difference (profile vs pre-dose)
18 V Sethuraman/FDA-Industry Workshop/14-16 Sept., 2005
50
Impact on QT Correction Method
40
Percent of Total
30
20
10
0
-40
-20
0
QTci difference (profile vs pre-dose with placebo)
19 V Sethuraman/FDA-Industry Workshop/14-16 Sept., 2005
20
Endpoint and Hypotheses
From E14: “... The upper bound of the 95% one-sided confidence interval
for the largest time-matched mean effect of the drug on the QTc interval
excludes 10 ms.”
To construct a CI for ‘largest time-matched difference” is a difficult
statistical problem
Impact on type II error (sponsor’s risk) while planning these trials
Intersection-Union Hypothesis
H o : { S (i ) p (i ) } 10, i 1,2,.....k
H1 : { S (i ) p (i ) } 10, i 1,2,.....k
S ( i ) , p ( i ) -Mean CFB QTc for study drug and placebo &
-k refers to # of time points
20 V Sethuraman/FDA-Industry Workshop/14-16 Sept., 2005
Hypotheses
Hochberg and Thamane (1987) - Multiple time points does
not have any impact on the type I error rate (public risk).
I-U Test does not assure overall power of the test (sponsor’s
risk), i.e., the more time points you test, the higher the chance
of type II error.
Since observations within same subject (time points) are
possibly correlated, it is expected that K hypotheses are also
correlated.
Not aware of statistical methodology to obtain sample size
accounting for the correlation.
Result from Simulation accounting for correlation.
21 V Sethuraman/FDA-Industry Workshop/14-16 Sept., 2005
Hypotheses and Sample Size
Need to an understand the correlation
structure and a prior estimate of .
From Simulation
Assume AR(1) =0.1
True treatment difference (activeplacebo) = 2 ms.
Impact on sample size minimal if k>5.
60
40
20
Sample size decreases to n=70 if
correlation is assumed to be =0.5
Power
Sample size increases from n=62 per
arm to 80 per arm to maintain power
at 90%.
80
Number of time points = 5
20
40
60
Sample Size
22 V Sethuraman/FDA-Industry Workshop/14-16 Sept., 2005
80
100
Disease Specific Consideration (e.g., cytotoxic
cancer drugs).
It may not be feasible to include positive control or even
placebo
Limited baseline values
May not be possible to study in healthy volunteers
Uncertain in terms of positive control effects
May not be possible to achieve supra-therapeutic dose
Use PK-QT modeling to predict at higher dose
Use Monte Carlo simulation to simulate models with fixed
and random effects to determine the expected value of the
model.
23 V Sethuraman/FDA-Industry Workshop/14-16 Sept., 2005
Disease Specific Consideration
An example using PK-QT
simulation
Consider a ‘thorough’ QT study
conducted at therapeutic dose in
healthy volunteers
Due to toxicity of drug, a supratherapeutic dose is not possible in
healthy but PK exposure available
from DDI study in patients.
Develop PK-QT models & use
simulation to predict QT effects at
higher exposure.
24 V Sethuraman/FDA-Industry Workshop/14-16 Sept., 2005
PK ij i ij
QTcij Si ij
Conclusion
‘Though’ QT study should be treated as any pivotal trial
and should use robust design features.
In general, Crossover designs are preferred.
Proper attention should be given to the choice of positive
control and expected effect size.
Baseline should be adequate to address both the central
tendency analysis and categorical analysis.
Sample size should be adequately powered to protect type
II error in the I-U hypothesis testing.
PK-QT modeling is highly recommended for all ‘thorough’
QT study.
25 V Sethuraman/FDA-Industry Workshop/14-16 Sept., 2005
Reference
1. Bazett JC. An anlysis of time relations of electocardigrams. Heart 1920; 7:353367.
2. Fridericia LS. Die Systolendauer im Elektrokardiogramm bei normalen Menschen
und bei Herzkranken. Acta Medica Scandinavia 1920; 53:469-486
3. Malik M. Problems of heart rate correction in the assessment of drug-induced QT
interval prolongation. Journal of Cardiovascular Electrophysiology 2003; 12:411420
4. Evaluation of Vardenafil and Sildenafil on Cardiac Repolarization, Morganroth J,
Ilson BE, Shaddinger BC, Dabiri GA, Patel BR, Boyle DA, Sethuraman VS,
Montague TH, - The American Journal of Cardiology, 2004
5. Leslie Kenna, et. al., Clinical Pharmacology Subcommittee of the Advisory
Committee for Pharmaceutical Science (2003)
6. ICH E14: The Clinical Evaluation Of Qt/Qtc Interval Prolongation And Proarrhythmic
Potential For Non-antiarrhythmic Drugs
(http://www.emea.eu.int/pdfs/human/ich/000204en.pdf)
7. Patterson S., et al. (2003). Investigating drug-induced QT and QTc prolongation in
the clinic: statistical design and analysis considerations. Report from the
Pharmaceutical Research and Manufacturers of America QT Statistics Expert
Working Team
26 V Sethuraman/FDA-Industry Workshop/14-16 Sept., 2005
Acknowledgements
Timothy Montague, GSK
Tianyu Li, Fox Chase Cancer Center, PA.
GSK QT Steering committee
Novartis QT sub-group
Joel Morganroth, eRT, PA
Lixia Wang, Novartis, NJ
Organizers: Sue Walker, George Rochester and Tim
Montague
27 V Sethuraman/FDA-Industry Workshop/14-16 Sept., 2005