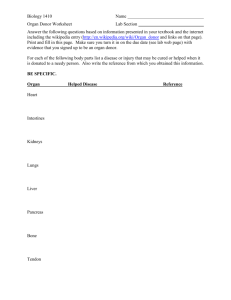
Organs & Tissues That May Be Transplanted
advertisement

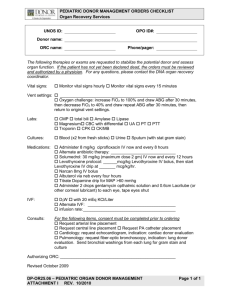
Donor Management of the Consented Donor Presented by Adam J. Teller, CPTC Procurement Transplant Coordinator Ms. Anne Gulatto Overview • • • • • OneLegacy UNOS ( United Network for Organ Sharing) Collaborative Practice Donor management Success stories OneLegacy • Founded in 1977 • Not for profit • Federally funded and designated by CMS as an OPO • Licensed by California as a tissue bank • Serving 220 hospitals, 14 transplant centers & 18.1 million residents • Serve seven counties in Southern California Umbrella Organizations • United Network for Organ Sharing • Maintains the National Organ Transplant Waiting List under contract with the U.S. Department of Health and Human Services • American Association of Tissue Banks • Provides tissue banking standards to promote quality and safety in tissue transplantation • Association of Organ Procurement Organizations • Recognized as the national representative of organ procurement organizations (OPOs) • The EBAA is the nationally recognized accrediting body for eye banks United Network for Organ Sharing (UNOS) • Maintains U.S. organ transplant waiting list • Determines national organ donation policy • Private, non-profit organization that operates the Organ Procurement & Transplantation Network & U.S. Scientific Registry of Transplant Recipients • Under contract with Center for Medicare & Medicaid Services (CMS) of the U.S. Dept. of Health & Human Services Collaborative Practice • OPO and hospital will identify the Best Practices and implement them collaboratively • Best Practices include – – – – – – Early Referral Effective Request Process Donor councils Education Tracking of hospital performance Consistency of donor management Patients on the UNOS Waiting List Heart Lung Heart/Lung Liver Kidney Kidney/Pancreas Pancreas Intestine Local 218 174 12 3,407 17,273 445 120 26 National 3,158 1,839 72 15,951 84,331 2,196 1,469 245 TOTAL 21,675 106,916 Source: UNOS April 9th 2010 UNOS Organ Allocation Policy Potential recipients are ranked by these criteria: Urgency of Need For heart & liver patients, the sickest at the top of the list Blood Type ABO must be compatible Size Height and weight must be compatible Tissue Typing For kidneys & pancreas OneLegacy Donor Service Area • Local – Seven-county area • Regional – We are in Region 5 • National – A total of 11 UNOS Regions in the U.S. Organs & Tissues That May Be Transplanted ◄ ORGANS ◄ ◄ ◄ ● Kidneys ● Liver ● Heart ● Lungs ● Pancreas ● Sm. Intestine TISSUES ● ● ● ● ●◄ ● ◄ ◄ Cornea/Eyes Heart Valves Skin Bone Tendons Cartilage Veins ◄ ◄ ◄ ◄ ◄ ◄ ◄ Donor Management • Procurement Transplant Coordinator (PTC) discontinues all previous orders and writes new orders – The PTC is responsible for the management of the multiple organ donor from the consent through the operating room recovery process. – This first set of orders will be one or two full pages, (standardized orders) and yes, everything is STAT….have I said how much we appreciate your hard work? Donor Management • Central line and A-lines are inserted if not already done • Central lines: IJ or SC for accurate readings of CVP measurement. Donor Management General Goals • • • • • • • • • • SBP 90-110 mmHg U/O 1-3 cc/kg HR 60-140 PAWP 7-12 Serum electrolytes WNL-Checked q 6 hours and prn CBC and coags WNL-Hct at least 30 SPO2 >95% PaO2 90-110 torr pH 7.35-7.45 PCO2 35-45 torr General Goals • • • • • Frequent ABG’s (q 2-4 hours) PIP <32 mm Hg Lowest possible Fio2 Turn, bag and suction q 2 hours Antibiotic coverage – Zosyn 3.375 grams, Levaquin 750 mg, Vanco1 gram • Control of DI Donor Management • PCXR after line placement – If lungs are being procured, a PCXR is required at least every 6 hours • Fluid deficit correction • Evaluation of pressors and possible addition of T-4 (levothyroxine) drip • First dose of 1 gram Solumedrol IVP • Electrolyte, base deficit correction • Addition of broad spectrum antibiotics Vasopressin • Aka: Pitressin • Used as hormone replacement of ADH from posterior pituitary gland in brain dead patient • Very effective in treating DI related hypotension • May or may not give 1-2 units IV bolus of Vasopressin before starting drip • Drip rate is 0.5-2 units/ hour • Closely observe Urine Output—don’t make the donor anuric DI Treatment • Look at total I/O –since admission – Output mismatch with increased Na and decreased K+ suggests DI • Treat with Vasopressin/DDAVP • Calculate total volume deficit and replace with 0.9% or 0.45NS FORMULA: • 0.6 x body weight in kg = 1X • Serum Na x 1X divided by normal Na = X2 • X2 – X1 = total volume deficit in liters • Note that this may be 10 or 12 liters so give replacement over 12 to 24 hours Electrolyte Imbalances • ~40% of brain dead patients experience hypokalemia of less than 2.5 mEq/liter • Hypocalcemia, Hypophostemia may also ensue and may lead to myocardial depression • Hypernatremia and hypomagnesemia may occur, especially with DI Coagulopathy • Frequently seen in head trauma patients – GSW, SAH, Blunt trauma – Probably due to large amounts of tissue fibrinolytic agent (native tPa) from the necrotic brain into systemic circulation • Treat with appropriate blood products – Platelets, FFP, Cryoprecipitate, PRBC’s (leukocyte reduced) • Hct should be at least 30 for multiple organ recovery Donor Management Heart – 12 Lead EKG (serial) – Echocardiogram (serial) – Cardiac Enzymes CPK / MB, Troponin levels – Hormone replacement (T-4,Vasopressin, Steroids) – Cardiac Cath • Usually done on heart donors > 45 years old • May be necessary if pt is < 45 years old and has significant risk factors Echocardiogram • Effective in screening for anatomic abnormalities • Determine the physiological and hemodynamic stability / function • Tool to measure effectiveness of management – Hormone replacement – Fluid management Donor Management Lung • Changes after brain death occurs • Absence of bronchospasm due to death of brain stem and medulla oblongata • Declining function of bronchial submucosal glands • Decreased or absent function of cilia – These changes result in accumulation of mucus in the dependent lobes of the lungs • Potential for neurogenic pulmonary edema – Thought to occur as a result of dysfunction of neuroepithelial bodies found in the epithelium of the alveoli and distal bronchioles Donor Management Lung • • • • • • • • Maintain pCo2 35-45, pH 7.35-7.45 Keep patient warm Maximize tidal volume; 12-15cc/kg Aggressive chest PT Maintain CVP 6-10 Use colloid vs. crystalloid for fluid replacement Humidify at 100% relative humidity Over inflate ETT cuff Donor Management Lung • • • • Initiate pressure control ventilation and 1:1 I:E ratio PEEP of at least 5 Keep PIP < 32 Lowest possible FiO2 – Goal is PO2 of >125 on 40% and/or PF ratio >300 • Bag and Suction q2 hours • Chest PT, postural drainage, • ABG’s q 2 hours and prn Donor Management Lung • Possible use of Narcan 8-10 mg IVP • Alveolar Recruitment Maneuvers – CPAP of 30 for 1 or more minutes – Gradual increase of PEEP to 15-20 over 1-2 minutes • Pressure Control ventilation • Antibiotic coverage: Levaquin 500mg q 24h and Zosyn 3.375 grams q 8 hour, Vancomycin 1 gram q 24 hours Donor Management Lung • Chest X-Ray (serial) • Bronchoscopy (serial) – Sputum gram stain and C&S • ABG on 40% and 100% • Possible Chest CT – Usually for Trauma Patients and patients with significant history Donor Management Liver • Maintain Na < 150 • Correct Electrolyte Imbalances • Serial Liver Enzymes • Tap water NG Lavage • Possible Abdominal Ultrasound / CT Donor Management Kidney • Avoid DI • Serial UA with micro • Renal dose dopamine 2-5 mcg/kg/min • Serial BUN/ Creatinine Donor Management Pancreas • Serial Amylase, Lipase • Blood glucose ( <150 mg/dl ) • Minimize usage of IV dextrose • Tight glucose control Donor Management Continued “ 92% of organs that fail to meet transplantation criteria on initial evaluation can be functionally resuscitated.” Zaroff, JZ. Et al. Consensus Conference Report: Maximizing use of organs recovered from the cadaver donor: Cardiac recommendations”. Circulation 2002;106:836. The Gift of Life For many families: • The gift of organ and tissue donation is the only positive experience in the tragic chain of events surrounding the loss of their loved one. • It can help give meaning to an otherwise senseless event that has occurred. Donor Management Remember! The survival of transplanted organs depends heavily on pre donor and donor management implementations Lily 2008 1984 Liver tumor, awaiting transplant Matthew Bemis, Lily’s donor 1985 Tong Tong Hao (Recipient) “She runs, jumps and plays everyday instead of sitting in the stroller.” – Yehong & Frost, Tong Tong’s parents Ms. Anne Gulatto Additional Resources • UNOS Critical Pathway for the Organ Donor: http://www.unos.org/resources/pdfs/CriticalPathwayPoster.pdf • Zaroff, JZ. Et al. Consensus Conference Report: Maximizing use of organs recovered from the cadaver donor: Cardiac recommendations”. Circulation 2002;106:836. • Zaroff, JZ. Echocardiographic evaluation of the potential cardiac donor. J Heart Lung Transplant 2004; 23(95):S250. • • The Role of Thyroid Hormone in Donation, Transplantation and Cardiovascular Disease (Medical Management to Optimize Donor Organ Potential February 23-25, 2004 California Health and Safety Code, sections 7150-7156.5, 7180-7184.5 and 71887195.