Clinical trials - Department of Neurology
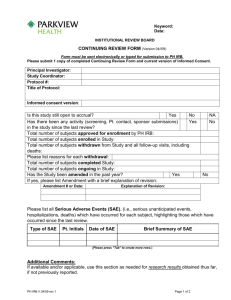
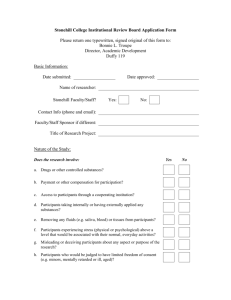
advertisement

Clinical trials: unique aspects of clinical-based grants Grant-Writing Series June 12, 2012 Marian Limacher, MD Senior Associate Dean for Faculty Affairs and Professional Development AHA Endowed Professor of Cardiovascular Research The challenges of patient oriented research • Complex, hard to do – lots of regulations • Takes a long time • High cost • You will underestimate your ability to recruit subjects • You will overestimate your effect size Human Subjects Research • What is “clinical research”? NIH Director's Panel on Clinical Research, 1997 • (a) Patient-oriented research. Research conducted with human subjects (or on material of human origin such as tissues, specimens and cognitive phenomena) for which an investigator (or colleague) directly interacts with human subjects. This area of research includes: – – – – Mechanisms of human disease Therapeutic interventions Clinical trials. Development of new technologies • (b) Epidemiologic and behavioral studies • (c) Outcomes research and health services research. Not “clinical research”: • in vitro studies that utilize human tissues but do not deal directly with patients. • In other words, clinical or patient-oriented research is research in which it is necessary to know the identity of the patients from whom the cells or tissues under study are derived. • For funding, the emphasis is on research concerned with examining patients. • Mixed grant applications, as in program projects in which one element of the proposal is an animal model and one is a human model, may also be classified as clinical research Spectrum of Research What is a clinical trial? • a clinical trial is a "research study to answer specific questions about vaccines, new therapies or new ways of using known treatments. Clinical trials (also called medical research and research studies) are used to determine whether new drugs or treatments are both safe and effective. • Carefully conducted clinical trials are the fastest and safest way to find treatments that work in people." Source: Clinicaltrials.gov Types of Clinical Trials • • • • • Treatment trials test new treatments, new combinations of drugs, or new approaches to surgery or radiation therapy Prevention trials look for better ways to prevent disease in people who have never had the disease or to prevent the disease from returning. Approaches may include medicines, vitamins, vaccines, minerals or lifestyle changes Screening trials try to find a better way to detect certain diseases or health conditions Quality of life trials explore ways to improve comfort and quality of life for individuals with chronic illness Nontherapeutic trials hope to answer specific research questions without using any type of treatment on participants. This may be accomplished by reviewing medical records, doing certain types of medical tests or asking participants questions in a survey. Design Issues • What type of study will best answer the question? • What type of study will I be able to do? Observational Studies • Is there a comparison or “control” group? Yes = “analytical” No = “descriptive” • For analytic studies -- determine time sequence What is a control? • "a control is the standard by which experimental observations are evaluated. In many clinical trials, one group of patients will be given an experimental drug or treatment while the control group is given either a standard treatment of the illness or a placebo." Source: Clinicaltrials.gov Cohort Study looking forward, aka “prospective” Exposure (Risk Factor) Outcome (Disease) Time Cohort Studies • May establish -– Incidence of the outcome over time – Risk factors – Protective factors • Downsides – Not useful for rare diseases – Expensive – May contain biases Case-Control Study Exposure (Risk Factor) Outcome (Disease) Time Case-Control Example • Investigating a food-borne illness on a ship • Question all those who became ill • Identify what they ate, medicines, underlying conditions • Identify a number of other shipmates and ask same questions • Analyze what was more common among those who became ill • Final result: it was the German potato salad Case-Control • Useful for – Rare diseases – Conditions that develop over a long time (heart disease) – “easier” than cohort studies, less time, effort and fewer subjects needed • Downside – Appropriate “control” group can be difficult to identify – Recall bias (relies on subject memory of some risk factors) Cross-Sectional Study Exposure (Risk Factor) “Snapshot” In time Outcome (Disease) Time Other research reports • Case study – Report of a single case (patient) with unusual, interesting findings that illustrate a lesson in diagnosis, treatment or outcome • Case series – Several case studies of the same condition – Consecutive cases, e.g. reporting outcome with a new surgical technique Deciding which study to answer the question(s) • Descriptive studies – Describe the features of a new disease – Frequency of the condition – Determinants of the condition • First description of Legionnaire’s disease • First report of Toxic Shock syndrome • No comparison or control group • No ability to determine associations or causes Randomized, Controlled Clinical Trial (RCT) • Considered the “gold standard” among clinical research designs • Can best identify whether “X” results in improved outcomes • Rather than some characteristic(s) of the participants and not the intervention itself – Reduces bias • Selection • Confounding • informational Sample size • Do it! • Consult a statistician – at the design phase • Include an analysis plan in your methods Planning for Drop out • Increase sample size • Decide in the analysis plan how they will be handled • Another issue for your statistician The Regulatory Aspects • • • • IRB RAC HIPAA Reporting Fundamentals of Human Subject Protection and the IRB Process Ensuring That All Research Involving Human Subjects Meets Federal, State, and Institutional Guidelines Tiffany Danielle Pineda Education Coordinator tiffany.danielle@ufl.edu (352) 273-9604 Responsibilities in Research • Institutional Responsibilities • Institutional Review Board Responsibilities • Investigator Responsibilities Institutional Responsibilities – Federalwide Assurance • Under Federal regulations, any institution engaged in Federally-supported human subjects research must commit itself in writing to the protection of those subjects. • UF guarantees adherence to Title 45, Part 46, of the Code of Federal Regulations. • UF will review ALL research involving human subjects. IRB Responsibilities • UF Utilizes 4 IRBs IRB01: Health Science Center IRB02: Behavioral/Non-Medical IRB03: Jacksonville IRB04: Western IRB (Industry Sponsored) • Review all proposed human subject research at the University of Florida in accordance with established guidelines. IRB Responsibilities Cont. • Authority to approve, request modification in, and/or disapprove research. • Authority to suspend or terminate previously approved research that is not being conducted in accordance with the IRB’s requirements, or that has been associated with unexpected serious harm to subjects. • To observe, or have a third party observe, the conduct of the research. • To observe, or have a third party observe, the consent process. Investigator Responsibilities Investigators have the primary responsibility for protecting the rights and welfare of human research subjects and are responsible for complying with all applicable provisions of their institution's Assurance. Investigator Responsibilities Cont. Investigators are expected to be knowledgeable about the requirements of the Federal regulations, applicable state law, their institution's Assurance, and institutional policies and procedures for the protection of human subjects. Investigator’s Responsibilities Cont. • Conducting their research according to the IRB approved Protocol. • Ensuring that each potential subject understands the nature of the research. • Providing a copy of the IRB-approved Informed Consent document to each subject at the time of consent. Investigator Responsibilities Cont. • Promptly submitting proposed changes for review prior to implementation. • Promptly reporting any unanticipated problems and adverse events. • Submitting the continuing review and study closure forms. Research Requiring IRB Approval All research that involves intervention/interaction with human subjects or their identifiable protected health information must be reviewed by the IRB BEFORE it is conducted. Ethical and Regulatory Considerations • Would I let a family member take part in the study? • Is the study design ethical? • Are the risks worth taking? • Why is a special population or site included or excluded? Study Procedures • In ample detail, establish what really happens, and the risk to subjects. – – – – – – – Time commitment. Setting or site. Are “routine” agents used? How is the data analyzed? Logical, chronological, rationalized, and prioritized. Make sure the Consent and Protocol match. Consent form is written at 8th grade reading level. Qualifications of the Staff • Confirm the study staff’s duties, qualifications, and roles. Subject Selection/Enrollment • How are subjects identified ? Ads, charts, referrals, own clinic, support groups, public • How many subjects are needed? Is there enough to answer the question records, etc. posed? • How, when and by whom are subjects first contacted about the study? Letter? In person? By whom? Safety Monitoring • How is data monitored and by whom? – Every study needs a safety monitoring PLAN! – Provide objective criteria for withdrawal of subject for safety reasons! – Make sure to have stopping rules. – Submit necessary reports to IRB! (adverse events, deviations/non-compliance, unanticipated problems, revisions, and such) Risks and Discomforts • Listed clearly, quantitatively, and in order of seriousness. • Also consider: – The costs and risks of withdrawal of current medications! – The non-medical risks (social and psychological). – Always guard against potential loss of confidentiality. Benefits • Monetary compensation is NOT a benefit. • State the benefits to individual then to society. Consent • Consent is a process not a form but the Form is the formal record/document • Consent is ongoing • Timing is important - the details should be submitted • Anyone who signs a Consent form is considered formally enrolled or whose records are accessed under an approved Waiver Consenting Cont. • Adults >18 years of age, sophisticated teens may read adult Form. ( Must be written at the 8th grade reading level) • All minors require parent/guardian to sign Consider who you have doing the Consenting • Consent for activities corresponds with their typical clinical practice in medicine. • Examples: – (Breast Study) Mammogram Technologist. – (Investigational drugs/devices) Licensed MD - 8 Mandatory ICF Elements • A statement that the study involves research, an explanation of the purposes of the research and the expected duration of the subject's participation, a description of the procedures to be followed, and identification of any procedures which are experimental; • Description of Risks; • Description of Benefits; • Alternatives to Participation; • How Privacy and Confidentiality of records will be maintained; ICF Mandatory Elements Cont. • An explanation as to whether any compensation and medical treatments are available if injury occurs and, if so, what they consist of, or where further information may be obtained; • Who to contact for answers about the research, research subjects' rights, and research-related injury; and • A statement that participation is voluntary, refusal to participate will involve no penalty or loss of benefits to which the subject is otherwise entitled, and the subject may discontinue participation at any time without penalty or loss of benefits to which the subject is otherwise entitled. IRB Submission http://irb.ufl.edu/ Research Administration & Compliance Health Science Center Research Billing Risks Edy Zettler, BS Education & Training Coordinator Broad Building, Room 102-H (1300 Center Drive at Mowry Road) ezettler@ufl.edu 352-273-6244 Health Science Center (HSC) Policy – All research conducted in the HSC will be in compliance with applicable State & Federal regulations. – All PIs & their designees will provide necessary information to appropriate service personnel to ensure proper billing procedures. Why is this Pertinent? Clinical Research Study Policy addressing billing/claims established by Center for Medicare and Medicaid Services (CMS) in 2000! Audits (internal and external) – refunds. Institution can be liable for damages & fines. PI, institution, billing providers subject to a fraud investigation. HSC Research Billing Risks Two areas of risk: Billing Claims Fiscal Language Billing Claims Risks Cannot bill out items that are paid for or provided by sponsor – Tracking essential! Care must be taken to ensure billable items can be billed out per Medicare Rules. Fiscal Language Informed Consent Language must accurately reflect Study’s fiscal obligations (cannot conflict with protocol, contract, budget). Discrepancies can have financial implications for PI’s department, UF, Shands and/or the participant. Patient Costs Subject Injury What Does RAC Do? Research Administration & Compliance (RAC) Responsibilities Multiple reviews of HSC studies that involve Human Subjects and Services. Education & Training to promote billing compliance. Financial Language Assessment (FLA) Forms. Audit research activity & provide guidance for reconciliation. Investigate/address billing noncompliance allegations. Where can I get help? Resources & Contact Information – RAC Liaisons (273-5398) – RAC Education & Training Staff (273-5946) – DSR Representative in RAC (273-5392) – RAC Auditors (273-5946) – Monthly Roundtables & AD Hoc Meetings – RAC Newsletters Where can I get help? Websites – http://ctc.health.ufl.edu/ – http://www.med.ufl.edu/research/rac/ Where can I get help? Training & Classes – Mandatory Online Training Module – Research Billing Crash Course: The Essentials – To Bill or Not to Bill: What is the Difference? – Service Provider Communication – Building a Great Detailed Budget – Navigating the Clinical Trials Compliance Website – Why Track Services Now? Save Time and Money Later! – Study Registration & Initiation Sign up through MyUFL UF Resources • Clinical and Translational Science Institute National Consortium of 60 Academic Health Centers The UF CTSI is supported in part by NIH awards UL1 RR029890, KL2 RR029888 and TL1 RR029889 A Catalyst for Collaboration CTSA consortium Corporate Partners 16 UF Colleges UF CTSI University Partners Health Care Systems Community Partners The UF CTSI is supported in part by NIH awards UL1 RR029890, KL2 RR029888 and Regulatory Knowledge and Research Support • Overarching goal – To increase accessibility of information by providing expert investigator assistance via Research Project Navigators, and provide prompt access to research and training resources ensuring rapid activation of research • Services provided – – – – – – – – Trial design and database (RedCap) Quality assurance Clinical and research ethics Regulatory affairs IRB assistance Contract negotiations Billing and budgeting Technology transfer The UF CTSI is supported in part by NIH awards UL1 RR029890, KL2 RR029888 and TL1 RR029889 Wajeeh Bajwah, PhD Research Design and Analysis • Overarching goal – Consult, collaborate and conduct research and educate on study design and biostatistical issues in CTS. • Activities – Study Design – clinical trials, observational studies, cohort, chart review, qualitative, epidemiologic – Power Analysis – Study Analysis – Data presentation and visualization The UF CTSI is supported in part by NIH awards UL1 RR029890, KL2 RR029888 and TL1 RR029889 Jon Shuster, PhD CTSI web portal • www.ctsi.ufl.edu • To request a consultation on any topic related to clinical and translational science or any of the programs, services or activities of the UF CTSI, please call 352-273-8700. • Research Project Navigators: – Teresa D’Angelo, RN, BSN, CCRC (danget@shands.ufl.edu) – (352) 265-0032 H. Robert Kolb, RN, BS, CCRC (kolbhr@ufl.edu) – (352) 2738882 Douglas Theriaque, MS (theriaqu@ufl.edu) – (352) 273-8877 Key recommendations • Background: – Demonstrate experience with recruitment – Provide convincing evidence of an adequate, suitable population • Methods: – Provide the complete subject protocol – Organize by time – provide table, which interventions at which time/visit – Also provide a full study timeline – Work with a statistician, include an analysis plan • Have IRB approval at the time of submission, if possible • Must include a safety and monitoring plan • Address possible pitfalls - honestly Want more? • • • • • • • Introduction to Clinical/Translational Research 2 week course: July 13-27, 2012 2:00 – 5:00 pm Didactics – covering the spectrum of CTR Small group projects Check CTSI website to register Or contact: Eve Johnson 273-9307