Med List – Care Plan Version (1)
advertisement
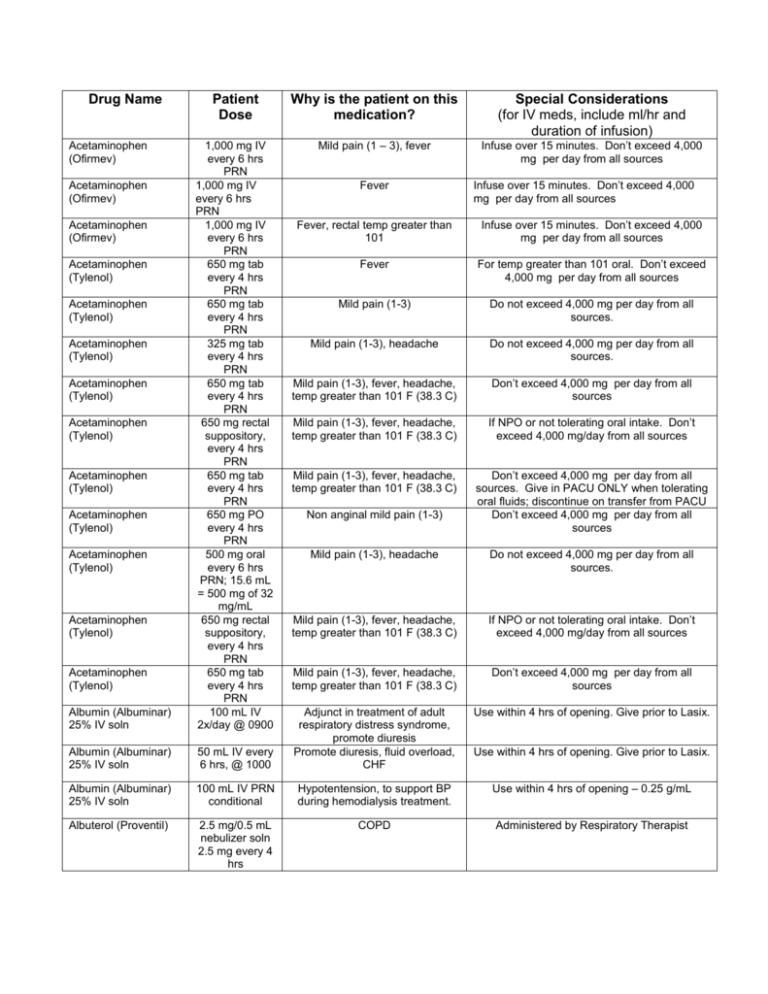
Drug Name Patient Dose Why is the patient on this medication? Special Considerations (for IV meds, include ml/hr and duration of infusion) Mild pain (1 – 3), fever Infuse over 15 minutes. Don’t exceed 4,000 mg per day from all sources Albumin (Albuminar) 25% IV soln 1,000 mg IV every 6 hrs PRN 1,000 mg IV every 6 hrs PRN 1,000 mg IV every 6 hrs PRN 650 mg tab every 4 hrs PRN 650 mg tab every 4 hrs PRN 325 mg tab every 4 hrs PRN 650 mg tab every 4 hrs PRN 650 mg rectal suppository, every 4 hrs PRN 650 mg tab every 4 hrs PRN 650 mg PO every 4 hrs PRN 500 mg oral every 6 hrs PRN; 15.6 mL = 500 mg of 32 mg/mL 650 mg rectal suppository, every 4 hrs PRN 650 mg tab every 4 hrs PRN 100 mL IV 2x/day @ 0900 Albumin (Albuminar) 25% IV soln Acetaminophen (Ofirmev) Acetaminophen (Ofirmev) Acetaminophen (Ofirmev) Acetaminophen (Tylenol) Acetaminophen (Tylenol) Acetaminophen (Tylenol) Acetaminophen (Tylenol) Acetaminophen (Tylenol) Acetaminophen (Tylenol) Acetaminophen (Tylenol) Acetaminophen (Tylenol) Fever Infuse over 15 minutes. Don’t exceed 4,000 mg per day from all sources Fever, rectal temp greater than 101 Infuse over 15 minutes. Don’t exceed 4,000 mg per day from all sources Fever For temp greater than 101 oral. Don’t exceed 4,000 mg per day from all sources Mild pain (1-3) Do not exceed 4,000 mg per day from all sources. Mild pain (1-3), headache Do not exceed 4,000 mg per day from all sources. Mild pain (1-3), fever, headache, temp greater than 101 F (38.3 C) Don’t exceed 4,000 mg per day from all sources Mild pain (1-3), fever, headache, temp greater than 101 F (38.3 C) If NPO or not tolerating oral intake. Don’t exceed 4,000 mg/day from all sources Mild pain (1-3), fever, headache, temp greater than 101 F (38.3 C) Don’t exceed 4,000 mg per day from all sources. Give in PACU ONLY when tolerating oral fluids; discontinue on transfer from PACU Don’t exceed 4,000 mg per day from all sources Non anginal mild pain (1-3) Mild pain (1-3), headache Do not exceed 4,000 mg per day from all sources. Mild pain (1-3), fever, headache, temp greater than 101 F (38.3 C) If NPO or not tolerating oral intake. Don’t exceed 4,000 mg/day from all sources Mild pain (1-3), fever, headache, temp greater than 101 F (38.3 C) Don’t exceed 4,000 mg per day from all sources Use within 4 hrs of opening. Give prior to Lasix. 50 mL IV every 6 hrs, @ 1000 Adjunct in treatment of adult respiratory distress syndrome, promote diuresis Promote diuresis, fluid overload, CHF Albumin (Albuminar) 25% IV soln 100 mL IV PRN conditional Hypotentension, to support BP during hemodialysis treatment. Use within 4 hrs of opening – 0.25 g/mL Albuterol (Proventil) 2.5 mg/0.5 mL nebulizer soln 2.5 mg every 4 hrs COPD Administered by Respiratory Therapist Acetaminophen (Tylenol) Acetaminophen (Tylenol) Use within 4 hrs of opening. Give prior to Lasix. Albuterol (Proventil) 2.5 mg/0.5 mL nebulizer soln 2.5 mg every 2 hrs PRN 5 mg/mL neb soln every 4 hrs when awake 2.5 mg/0.5 mL nebulizer soln, 2.5 mg every 4 hrs when awake 2.5 mg every 4 hrs PRN For wheezing, shortness of breath Administered by Respiratory Therapist Pneumonia, bronchodilator, history of asthma Administered by respiratory therapist As needed for shortness of breath Administered by Respiratory Therapist. Dilute in 3 ml of NS Dyspnea/wheezing Administered by respiratory therapist. Dilute in 3 mL NS. 90 mcg/actuation inhaler 2 Puff. Every 4 hrs PRN 1 mg every 8 hrs PRN For wheezing, shortness of breath Administered by Respiratory Therapist Anxiety Adverse effects: drowsiness, sedation. Atrial fibrillation, atrial flutter Crush to admin via NG tube. One possible cause of interstitial lung disease. Peak 2-7hr Antiarrhythmic, Antianginal. (prevention or suppression of cardiac arrhythmias) Antiarrhythmic, Antianginal Admin over 10 mins Amiodarone (Cordarone) 0.25-.05 mg PO every 8 hrs PRN 200 mg tab, NG Tube, 2x/day @ 0900 150-300 mg IVP over 10 mins 360 mg IV over 6 hrs. Amiodarone (Cordarone) 540 mg IV over 18 hrs. Antiarrhythmic, Antianginal Maintenance infusion (over 18 hrs) Amlodipine (Norvasc) 5 mg tab daily Antihypertensive (calcium channel blocker) Monitor blood pressure (no parameters given) Amlodipine (Norvasc) 5 mg tab daily Antihypertensive, calcium channel blocker Hold for Systolic BP < 110 Amlodipine (Norvasc) Antihypertensive, calcium channel blocker Hold for Systolic BP < 90. Admin via G tube Amlodipine (Norvasc) 5 mg tab, 2x/day, due @ 0900 10 mg tab daily Antihypertensive (calcium channel blocker) Monitor blood pressure (no parameters given) Ascorbic acid (Vitamin C) 500 mg tab, oral, daily Vitamin C deficiency Ascorbic acid (Vitamin C) 500 mg tab, oral, daily, due @0900 325 mg tab @ 0900 Vitamin C deficiency Albuterol (Proventil) Albuterol (Proventil) Albuterol (Proventil) nebulizer solution Albuterol HFA (Proventil HFA) Alprazolam (Xanax) Alprazolam (Xanax) Amiodarone (Cordarone) Amiodarone (Cordarone) Aspirin Aspirin 325 mg tab @ 0900 Anxiety Atrial fibrillation, atrial flutter Patient on ventilator, NG Tube Acute MI May be administered with food to avoid GI upset. Aspirin Aspirin Aspirin (Bayer children’s aspirin) Atorvastatin (Lipitor) Atorvastatin (Lipitor) Atropine Enteric coated 325 mg tab daily 325 mg tab @ 0900 81 mg chewable tab @ 0900 10 mg tab daily 80 mg tab daily, at bedtime 1mg IVP Azithromycin (Zithromax) 1200 mg tab Azithromycin (Zithromax) Benazepril (Lotensin) 500 mg in D5W 250 mL injection IV every 24 hrs 500 mg in D5W 250 mL injection IV every 24 hrs due @ 1300 1g in D5W 100 mL IVPB at 200 mL/hr every 8 hrs, due @ 0900 Topical ointment applied 2x/day to affected areas, @0900 Topical ointment applied 2x/day to affected areas, @0900 10 mg tab daily Benazepril (Lotensin) Benzocaine-menthol (Cepacol sore throat) (max strength) Benzonatate (tessalon perles) Azithromycin (Zithromax) Aztreonam (Azactam) Bacitracin (Baciguent) Bacitracin (Baciguent) Acute MI, Antiplatelet May be administered with food to avoid GI upset. Atrial fibrillation, suspected MI Patient on ventilator, NG Tube. May be administered with food to avoid GI upset Acute MI, NSTEMI May be administered with food to avoid GI upset. Intubated. To reduce LDL cholesterol and triglyceride levels (Antilipemic), prevention of cardiovascular disease (pt. has had MI) To reduce LDL cholesterol and triglyceride levels (Antilipemic), history of hyperlipidemia, pt. has had MI Bradycardia, complete heart block, or escape rhythms with symptoms of hemodynamic compromise. (Anticholinergic, Antiarrhythmic) Suspected infection Avoid grapefruit juice Notify health care provider Cautious use in debilitated patients. UTI COPD, possible lung infection. Suspected infection Antibiotic, prophylaxis for infection Prevent bacterial infection of scalp laceration. Polypeptide antibiotic ointment, inhibits cell wall synthesis, effective against many gram pos. organisms. Prevent bacterial infection laceration. Polypeptide antibiotic ointment, inhibits cell wall synthesis, effective against many gram pos. organisms. Antihypertensive, ACE inhibitor Apply to scalp laceration only 20 mg tab daily Hypertension, antihypertensive ACE inhibitor Check BP before giving 1 Lozenge every 6 hrs PRN 100 mg cap every 8 hrs Sore throat Cough suppressant Apply to affected area Hold for Systolic BP < 110 Swallow whole, don’t crush or chew Bisacodyl (Dulcolax) Bisacodyl (Dulcolax) Bisacodyl (Dulcolax) Bupropion (Wellbutrin) 10 mg rectal suppository daily PRN 5 mg tab 2x/day PRN 10 mg rectal suppository every other day PRN 100 mg tab daily constipation Constipation Swallow whole, do not crush, chew, or split. constipation Antidepressant Buspirone (Buspar) 10 mg tab daily Antianxiety Calcium chloride 1g in NS 50 mL IV PRN conditional rate: 50 mL/hr 2g in NS 100 mL IV PRN conditional rate: 50 mL/hr 3g in NS 150 mL IV PRN conditional 1 g in D5W 100 mL injection, PRN conditional 12.5 mg PO every 8 hrs Calcium replacement For ionized Ca of 4.1-4.5, infuse over 1 hr. Calcium replacement For ionized Ca of 3.7-4.0, infuse over 90 mins. Calcium replacement For ionized Ca less than 3.7, infuse over 2-3 hours. Calcium replacement Ion Ca 4.1 to 4.5. Max infusion rate NOT TO EXCEED 1 g per hour Antihypertensive Hold for SBP < 110. Common adverse effects: cough, maculopapular rash. Life threatening adverse effects: Agranulocytosis, Angioedema 350 mg tab 4x/day Fibromyalgia Carvedilol (Coreg) 3.125 mg tab due @ 0800, 2x/day w/ meals For CHF. Antihypertensive, Adrenergic blocker Cefazolin (Ancef) 2g/20 mL IV, dose: 2g, every 8 hrs, @ 0800 Cefepime (Maxipime) 2g in D5W 100 mL IVPB Ceftriaxone (Rocephin) 2 g, 200 mL/hr, IVPB, every 12 hrs 1 g in D5W 100 mL IVPB @ 200 mL/hr every 24 hrs 1 g in D5W 100 mL IVPB @ 200 mL/hr every 24 hrs, due @ 1200 Antibiotic, prevention of infection after surgery, cephalosporin antibiotic. Inhibits cell wall synthesis. Antibiotic Calcium chloride Calcium chloride Calcium gluconate in D5W Captopril Carisoprodol (Soma) Ceftriaxone (Rocephin) Hold for HR less than 50 bpm. Hold for Systolic BP less than 100 mmHg. Administer with food if not NPO. Alpha and Beta-Adrenergic antagonist. Decreases myocardial O2 demand and lowers cardiac workload. Common adverse effect: dizziness. Life threatening: thrombocytopenia (low patelets). Cautious use: Coagulopathy. Peak: 5 mins IV, half-life: 90-130 mins. Promptly report onset of diarrhea, possible sign of pseudomembranous colitis. Infuse over 30 mins Pneumonia Infuse over 30 mins, do not infuse thru same IV line as Calcium containing IV solutions (including LR and TPN) E. Coli Pneumonia. Broad spectrum cephalosporin antibiotic. Broad spectrum against gram pos, gram neg coverage Infuse over 30 mins, do not infuse thru same IV line as Calcium containing IV solutions (including LR and TPN) Ceftriaxone (Rocephin) Clindamycin (Cleocin) Clonidine (Catapres) Clonidine (Catapres) Clonidine (Catapres) Clonidine (Catapres) Clopidogrel (Plavix) 2 g in D5W 100 mL mini-bag IVPB @ 200 mL/hr every 12 hrs, due @ 1600 600 mg in NS 50 mL IV, every 6 hrs, due @ 0930 0.1 mg tab every 6 hrs PRN 0.2 mg tab every 4 hrs PRN 0.1 mg tab every 6 hrs PRN 0.1 mg tab every 6 hrs PRN 75 mg tab @ 0900 COPD, possible lung infection. Broad spectrum cephalosporin antibiotic. Broad spectrum against gram pos, gram neg coverage Infuse over 30 mins, do not infuse thru same IV line as Calcium containing IV solutions (including LR and TPN) Antibiotic, prophylaxis for infection Hypertension For systolic BP greater than 160 or diastolic BP greater than 100. Hypertension, SBP > 170, or DBP > 110 For systolic greater than 170 or diastolic greater than 110. High BP, administer if systolic BP > 170 mm Hg Only give if meets parameters for high BP HTN, administer if systolic BP > 170 mm Hg Only give if meets parameters for high BP, check BP prior to admin. Blood thinner, helps prevent MI, stroke Adverse effects: hemorrhage, severe neutropenia, thrombotic thrombocytopenia purpura Adverse effects: hemorrhage, severe neutropenia, thrombotic thrombocytopenia purpura Apply to affected area 300 mg PO 1st dose, then 75 mg PO daily Topical, daily (time not stated) 5 mg tab 3x/day PRN Blood thinner, helps prevent MI, stroke. (Antiplatelet, Antithrombotic) Pressure ulcers, skin abrasions D10W 1,000 ml IV soln 10-125 mL/hr IV PRN conditional Fluid intake D10W 1,000 ml IV soln 10-125 mL/hr IV PRN conditional Fluid intake D10W 1,000 ml IV soln 10-125 mL/hr IV PRN conditional Fluid intake, glucose intake D5 ½ NS – KCL 20 mEq 1,000 mL IV soln @ 75 mL/hr continuous 100 mL/hr continuous Fluid intake, nutrition, electrolyte balance 1,000 mL IV soln @ 125 mL/hr continuous 25 g IV push, QID AC & HS PRN Nutrition, potassium, and fluid intake (electrolyte replacement) Hypervolemia and hyperkalemia, monitor blood glucose Hypoglycemia Admin SLOW IV push as needed for blood glucose less than 70 mg/dL (if unable to tolerate oral glucose). Recheck glucose after 15 mins, and repeat D50W 25 g if blood glucose is less than 80 mg/dL. Continue to Clopidogrel (Plavix) Collagenase (Santyl) topical ointment Cyclobenzaprine (Flexeril) D5 ½ NS 1,000 ml IV soln D5 LR with KCL 20 mEq/L D50W injection 25 g Muscle spasm If tube feeding is held. Begin at same mL/hr rate as tube feeding. Discontinue when tube feeding resumes AND blood glucose is greater than 100 mg/dL If tube feeding is held. Begin at same mL/hr rate as tube feeding. Discontinue when tube feeding resumes AND blood glucose is greater than 100 mg/dL. Pt. has fluid volume overload. If tube feeding is held. Begin at same mL/hr rate as tube feeding. Discontinue when tube feeding resumes AND blood glucose is greater than 100 mg/dL. Fluid intake monitor glucose every 15-20 mins until glucose returns to greater than 100 mg/dL x 2 Dextromethorphan Guaifenesin (Robitussin) Dextromethorphan Guaifenesin (Robitussin) Dextrose prefill IV syringe 12.5 g Dextrose prefill IV syringe 12.5 g Dextrose prefill IV syringe 25 g Digoxin (Lanoxin) 250 mcg/mL 10-100 mg/5 mL oral liquid 5 mL 10-100 mg/5 mL oral liquid 15 mL, Dose: 15 mL, every 4 hrs PRN 12.5 g IV QID AC & HS PRN Dose 25 mL, Admin dose 12.5 g, IV PRN conditional Dose 50 mL, Admin dose: 25 g, IV PRN conditional 250 mcg IV daily @ 0900 Cough Cough Hypoglycemia Hypoglycemia Hypoglycemia BG less than 50, give 50 mL D50W (1 amp) and re-check blood glucose every 15 mins. Atrial fibrillation. Mechanism: Inhibits the sodiumpotassium ATPase, which makes more calcium available for contractile proteins, resulting in increased cardiac output (positive inotropic effect), increases force of contraction, decreases heart rate (negative chronotropic effect), decreases AV conduction speed Admin over at least 5 mins. IV: onset 5-30min, peak 1-5hr, duration variable. Apical pulse for 1 min before giving product; if pulse <60 in adult, take again in 1 hr; if <60 in adult, call prescriber; note rate, rhythm, character; monitor ECG continuously during parenteral loading dose. Precautions: Pregnancy C, breastfeeding, renal disease, acute MI, AV block, severe respiratory disease, hypothyroidism, geriatric patients, sinus nodal disease, hypokalemia . Side Effects: Headache, drowsiness, apathy, confusion, disorientation, fatigue, hallucinations, dysrhythmias, hypotension, bradycardia, AV block, blurred vision, yellow-green halos, photophobia, diplopia, N/V, anorexia, abdominal pain, diarrhea Antianginal, Antiarrhythmic, Antihypertensive. (Calcium channel blocker) Tachycardia, HR > 120 Onset 30-60min, Peak 2-3hr immediate rel; Half-life 31/2 -9 hr Diltiazem (Cardizem) 30 mg PO every 6 hours Diltiazem (Cardizem) 5mg/mL Diphenhydramine (Benadryl) 20 mg/4 mL IV every 6 hrs PRN 25 mg IV, every 4 hrs PRN Diphenhydramine (Benadryl) 25 mg IV, every 4 hrs PRN Itching, insomnia Diphenhydramine (Benadryl) 50 mg/mL IV, every 6 hrs PRN Base dose 5 mcg/kg/min x 73.3 kg, Admin dose 366.5 mcg/min 11 Itching, hives, pruritus Dobutamine (Dobutrex) drip (conc: 2,000 mcg/mL) As needed for blood glucose less than 70 mg/dL (if unable to tolerate oral glucose). Recheck blood glucose after 15 mins, may repeat x 1 if blood glucose less than 70 mg/dL. BG 51-69 and if patient cannot take PO, give D50W, 25 mL (1/2 amp) IV push. For elevated HR above 120. Administer bolus dose over 2 mins. Onset 30-60min, Peak 2-3hr immediate rel; Half-life 31/2 -9 hr Itching Heart failure, cardiogenic shock Continuous drip, calculate dose per pt. weight. mL/hr Docusate sodium (Colace) 100 mg cap 2x/day PRN Stool softener Swallow whole, don’t crush or chew Docusate sodium (Colace) 250 mg cap, 2x/day Stool softener Swallow whole, do not crush or chew. Docusate sodium (Colace) 100 mg/10 mL oral liquid, 2x/day, @ 0900 Stool softener Possibly administer via NG tube Docusate sodium (Colace) 100 mg/10 mL oral liquid, 2x/day, @ 0900 Stool softener Administer via PEG tube Docusate sodium (Colace) 100 mg cap daily Stool softener Swallow whole, do not crush or chew. Do not give if diarrhea occurs, then reevaluate daily. Docusate sodium (Colace) 100 mg cap 2x/day due @ 0900 100 mg oral liquid 2x/day Stool softener Swallow whole, don’t crush or chew Stool softener . 5mcg/kg/minute IV infusion Cardiac stimulant, vasopressor Base dose 5 mcg/kg/min x 68 kg, Admin dose 340 mcg/min 12.75 mL/hr continuous drip 60 mg cap 2x/day Circulation problems due to MI, CHF, kidney failure vasopressor. Titrate to keep systolic greater than 100 mmHg. Obtain patient’s weight. Common adverse effects: hypotension, tachycardia. Continuous drip. Begin at 5 mcg/kg/min. Titrate to maintain rate based on parameters. Parameters: Aug Dias > 90. Not to exceed 20 mcg/kg/min. 1,000 mL IV soln @ 20 mL/hr continuous 100 mg tab, daily Electrolyte replacement Control of HIV Patient’s own medication, supplied as a unit dose package, request med from 6th floor pharmacy 0.625 IV, every 6 hrs PRN Hypertension, SBP >180 For systolic greater than 180. Check to see if Clonidine was administered. 1.25 mg IV, every 6 hrs PRN 0.625 mg IV, every 6 hrs PRN 40 mg/0.4 mL SubQ Hypertension, SBP >140 For systolic greater than 140. Check to see if other antihypertensive administered. Hypertension Systolic BP greater than 160. Max initial single dose in non-critical care areas is 0.625 Anticoagulant Notify physician for dosing or holding plan if invasive procedure, LP, or surgery is to be performed in next 24 hrs. Docusate sodium (Colace) 100 mg/10mL Dopamine Dopamine 800 mg in D5W 500 mL drip Duloxetine (Cymbalta) Electrolyte-R (pH 7.4) (Normosol-R) IV soln Elvitegr-cobicistemtric-tenof 150-150200-300 mg tab 100 mg *Patient Own Med* Enalaprilat (Vasotec) 1.25 mg/mL Enalaprilat (Vasotec) 1.25 mg/mL Enalaprilat (Vasotec) 1.25 mg/mL injection 0.625 mg Enoxaparin (Lovenox) Shingles (herpes zoster) Swallow whole, do not crush, chew, or spit. Capsules may be opened and the contents taken without crushing or chewing. Hypervolemia Enoxaparin (Lovenox) 40 mg/0.4 mL SubQ every 24 hrs 30 mg/0.3 mL SubQ Anticoagulant 40 mg/0.4 mL SubQ every 24 hrs @ 1800 40 mg/0.4 mL SubQ every 24 hrs, @ 0830 40 mg/0.4 mL SubQ every 24 hrs, due @ 0900 1 mg/kg SQ every 12 hours Anticoagulant (prophylaxis for blood clots) Famciclovir (Famvir) 500 mg tab 3x/day Shingles (herpes zoster) Famotidine (Pepcid) 20 mg tab daily Antiulcer drug Famotidine (Pepcid) 20 mg/2mL IV 2x/day GERD (H2 receptor antagonist) Famotidine (Pepcid) 20 mg tab 2x/day Antiulcer drug Famotidine (Pepcid) 20 mg/2mL IV 2x/day, @ 0900 GERD (H2 receptor antagonist), antiulcer drug Fentanyl (Duragesic) 75 mcg/hr transdermal patch, dose: 1 patch, every 48 hrs, due @ 1700 Pain, patient is allergic to morphine. Fentanyl (Sublimaze) 5,000 mcg in no diluent, 100 mL drip (conc: 50 mcg/mL). Dose 50 mcg/hr : 1 mL/hr, continuous. Peripheral IV R. Forearm, 20 g Moderate to severe pain Enoxaparin (Lovenox) Enoxaparin (Lovenox) Enoxaparin (Lovenox) Enoxaparin (Lovenox) Enoxaparin (Lovenox) Anticoagulant Anticoagulant Anticoagulant Anticoagulant, Antithrombotic Notify physician for dosing or holding plan if invasive procedure, LP, or surgery is to be performed in next 24 hrs. Dose adjusted for renal function (estimated CrCl 23 mL/min using SCr 1.68 on 8/3) Notify physician for dosing or holding plan if invasive procedure, LP, or surgery is to be performed in next 24 hrs. Notify physician for dosing or holding plan if invasive procedure or surgery is to be performed in next 24 hrs. Half-life 4 ½ hr Notify physician for dosing or holding plan if invasive procedure, LP, or surgery is to be performed in next 24 hrs. Notify physician for dosing or holding plan if invasive procedure, LP, or surgery is to be performed in next 24 hrs. Caution if creatinine clearance less than 30. Life threatening adverse effects: Angioedema, Hemorrhage, Thrombocytopenia. Dilute in 5 mL NS and administer over 2 mins. Dilute in 5 mL NS and administer over 2 mins. Life threatening adverse side effect: thrombocytopenia. Peak: 0.5-3 hr, duration: 10-12 hr Should ONLY be used in patients already receiving opiod therapy demonstrated opioid tolerance, and require daily dose equivalent to fentanyl 25 mcg/hr or greater. Patients considered opioid tolerant are those who have been taking, for a week or longer, equianalgesic doses of at least morphine 60 mg, oxycodone 30 mg, or hydromorphone 8 mg per day. ** Use in non-opioid tolerant patients may lead to fatal respiratory depression. Apply to clean, dry area of the chest, back, flank or upper arm.. If goal pain score not achieved: Use up to 2 bolus doses before increasing rate by 25 mcg/hr every 15 mins until goal pain score achieved. If at goal pain score: continue current dose. Max dose: 600 mcg/hr. Recommended max dose: 10 mcg/kg/hr. Notify intensivist if patient on max dose. Contraindications: substance abuse, significant respiratory compromise; cautious use: head injuries. Life threatening adverse side effect: circulatory depression, cardiac arrest, respiratory depression or arrest; Fentanyl (Sublimaze) 5,000 mcg in no diluent, 100 mL drip (conc: 50 mcg/mL). Dose 50 mcg/hr : 1 mL/hr, continuous. Peripheral IV #1 L. Wrist, pumping at 100 mcg/hr on planning day. Moderate to severe pain Fentanyl (Sublimaze) 50 mcg/mL IV injection every 5 mins PRN 25 mcg dose of 50 mcg/mL, IV injection, every 5 mins PRN 5,000 mcg in no diluent, 100 mL drip (conc: 50 mcg/mL). Dose 05 mcg/kg/hr x 83 kg : Admin dose 41.5 mcg/hr. 0.83 mL/hr IV continuous Pain Fentanyl (Sublimaze) Fentanyl (Sublimaze) Pain IVP every 5 mins up to 2 doses PRN pain before increasing continuous infusion rate. Moderate to severe pain, palliative care Initiate drip at 50 mcg/hr; titrate by 50 mcg/hr every 30 mins until target pain score of 0 is achieved and respiratory rate is less than 14 per hour. Max rate of 300 mcg/hr. Notify physician if target pain score and respiratory rate is not achieved at max hourly rate for further orders. Life threatening adverse side effect: circulatory depression, cardiac arrest, respiratory depression or arrest; Common adverse effect: nausea. Onset: immediate IV, peak 3-5 min IV, duration: 30-60 min IV If goal pain score not achieved: Use up to 2 bolus doses before increasing rate by 25 mcg/hr every 15 mins until goal pain score achieved. If at goal pain score: continue current dose. Max dose: 600 mcg/hr. Recommended max dose: 10 mcg/kg/hr. Notify intensivist if patient on max dose. Contraindications: substance abuse, significant respiratory compromise; cautious use: head injuries. Life threatening adverse side effect: circulatory depression, cardiac arrest, respiratory depression or arrest; Common adverse effect: nausea. Onset: immediate IV, peak 3-5 min IV, duration: 30-60 min IV IVP every 5 mins up to 2 doses PRN pain before increasing continuous infusion rate. Fentanyl (Sublimaze) 5,000 mcg in no diluent, 100 mL drip (conc: 50 mcg/mL). Dose 50 mcg/hr : 1 mL/hr, continuous. Moderate to severe pain Fentanyl (Sublimaze) 50 mcg/mL, dose: 25 mcg IV injection every 5 mins PRN 5,000 mcg in no diluent, 100 mL drip (conc: 50 mcg/mL). Dose 50 mcg/hr Pain Fentanyl (Sublimaze) Common adverse effect: nausea. Onset: immediate IV, peak 3-5 min IV, duration: 30-60 min IV If goal pain score not achieved: Use up to 2 bolus doses before increasing rate by 25 mcg/hr every 15 mins until goal pain score achieved. If at goal pain score: continue current dose. Max dose: 600 mcg/hr. Recommended max dose: 10 mcg/kg/hr. Notify intensivist if patient on max dose. Requires dual sign off! Contraindications: substance abuse, significant respiratory compromise; cautious use: head injuries. Life threatening adverse side effect: circulatory depression, cardiac arrest, respiratory depression or arrest; Common adverse effect: nausea. Onset: immediate IV, peak 3-5 min IV, duration: 30-60 min IV. IVP every 5 mins up to 2 doses PRN pain before increasing continuous infusion rate. Moderate to severe pain If goal pain score not achieved: Use up to 2 bolus doses before increasing rate by 25 mcg/hr every 15 mins until goal pain score achieved. If at goal pain score: continue current dose. Max dose: 600 mcg/hr. : 1 mL/hr, continuous. Fentanyl (Sublimaze) Fentanyl (Sublimaze) Fentanyl (Sublimaze) Ferrous sulfate (Feosol) Fluticasone – salmeterol (Advair HFA) 230-21 mcg/actuation inhaler Fluticasone (Flonase) 50 mcg/actuation nasal spray Fluticasone (Flonase) 50 mcg/actuation nasal spray Furosemide (Lasix) 10 mg/mL Furosemide (Lasix) 500 mg in no diluent, 50 mL drip (straight drug) Gabapentin (Neurontin) 25 mcg dose of 50 mcg/mL, IV injection, every 5 mins PRN 5,000 mcg in no diluent, 100 mL drip (conc: 50 mcg/mL). Dose 50 mcg/hr : 1 mL/hr, continuous. 25 mcg dose of 50 mcg/mL, IV bolus, every 5 mins PRN 325 mg tab 2x/day Pain Moderate to severe pain Pain Recommended max dose: 10 mcg/kg/hr. Notify intensivist if patient on max dose. Contraindications: substance abuse, significant respiratory compromise; cautious use: head injuries. Life threatening adverse side effect: circulatory depression, cardiac arrest, respiratory depression or arrest; Common adverse effect: nausea. Onset: immediate IV, peak 3-5 min IV, duration: 30-60 min IV IVP every 5 mins up to 2 doses PRN pain before increasing continuous infusion rate. Dose to be given from IV infusion pump. If goal pain score not achieved: Use up to 2 bolus doses before increasing rate by 25 mcg/hr every 15 mins until goal pain score achieved. If at goal pain score: continue current dose. Max dose: 600 mcg/hr. Recommended max dose: 10 mcg/kg/hr. Notify intensivist if patient on max dose. Contraindications: substance abuse, significant respiratory compromise; cautious use: head injuries. Life threatening adverse side effect: circulatory depression, cardiac arrest, respiratory depression or arrest; Common adverse effect: nausea. Onset: immediate IV, peak 3-5 min IV, duration: 30-60 min IV IVP every 5 mins up to 2 doses PRN pain before increasing continuous infusion rate. Dose to be given from IV infusion pump Iron deficiency Swallow whole, don’t crush, chew, or spit. 2 Puffs. Inhalation with spacer. 2x/day @0900 1 spray, both nares, daily Acute respiratory failure (interstitial lung disease) Administered by RT 2 sprays, both nares, 2x/day @ 0900 40 mg = 4 mL IV every 12 hrs @ 1200 Acute respiratory failure (interstitial lung disease) Dose: 30 mg/hr, infusion: 3 mL/hr, IV continuous drip 800 mg cap 3x/day Rhinitis Pulmonary edema; CHF, HTN. Loop diuretic. Action: Inhibits reabsorption of sodium and chloride at proximal and distal tubule and in the loop of Henle Pulmonary edema; CHF, HTN, fluid volume overload. Loop diuretic. Action: Inhibits reabsorption of sodium and chloride at proximal and distal tubule and in the loop of Henle Neuropathic pain May not be able to take due to NG tube/occluded nares. Onset 12hr, peak several days, duration 1-2 wk Life threatening adverse side effects: circulatory collapse, leukopenia, aplastic anemia, agranulocytosis (rare) Life threatening adverse side effects: circulatory collapse, leukopenia, aplastic anemia, agranulocytosis (rare). Protect from light. Gabapentin (Neurontin) 1,600 mg cap daily Neuropathy, neuropathic pain, fibromyalgia, insomnia Gabapentin (Neurontin) 400 mg cap 3x/day Neuropathic pain, migraine prophylaxis Glucagon (Glucagen) injection 1 mg 1 mg IM, QID AC & HS PRN, 1 mL = 1mg of 1 mg/mL Hypoglycemia Guaifenesin (Robitussin) 100 mg/5 mL, 200 mg, dose: 10 mL, every 4 hrs PRN 200 mg/10 mL every 4 hrs PRN 15 mL, 300 mg, oral, every 6 hrs PRN 7500 units SQ every 12 hours Cough Guaifenesin (Robitussin) Guailfenesin (Robitussin) 100 mg/5 mL oral liquid 300 mg Heparin Heparin 5,000 units/0.5 mL injection 10,000 units Heparin 5,000 units/0.5 mL injection 5,000 units Heparin 5,000 units/0.5 mL injection 5,000 units Heparin D5W 25,000 unit/500 mL (50 unit/mL) drip Heparin D5W 25,000 unit/500 mL (50 unit/mL) drip Heparin dosing per pharmacy 1 each Heparin dosing per pharmacy 1 each Hydralazine (Apresoline) 20 mg/mL injection If patient glucose less than 70 mg/dL, has a decreased level of consciousness, is unable to take glucose orally, and IV access cannot be established within 5 mins, administer glucagon 1 mg IM then continue to attempt IV access. Place pt. in lateral recumbent position in anticipation of vomiting. Monitor glucose every 15-20 mins and repeat 1mg IM if glucose remains less than 80 mg/dL. Continue to monitor glucose every 15-20 mins until it returns to greater than 100 mg/dL x2. Sore throat, cough Congestion, cough Anticoagulant Requires 2 nurse check. Life threatening adverse effects: spontaneous bleeding, thrombocytopenia, bronchospasm, anaphylactoid reactions. 2 nurse check, potential for bleeding. 10,000 units Intracatheter, PRN conditional, post hemodialysis tx 5,000 units SubQ every 12 hrs-STD 5,000 units SubQ every 12 hrs-STD, due @ 0900 2,000 units/hr, 40mL/hr, IV continuous drip 1,550 units/hr, 31 mL/hr, IV continuous drip 1 each, daily PRN For post hemodialysis treatment; Anticoagulant 1 each, daily PRN, Pharmacy consult 10 mg IV, every 4 hrs PRN; admin 0.5 mL = 10 mg of 20 mg/mL For NSTEMI, Anticoagulant Heparin dosing and monitoring (including platelets) in accordance with medical centerapproved guideline and policy and procedure. HTN, For Systolic BP > 170. Non-nitrate vasodilator Only give if meets parameters for high BP, check BP prior to admin. Anticoagulant, deep venous thrombosis 2 nurse check Anticoagulant, DVT prophylaxis 2 nurse check, potential for bleeding. Anticoagulant Requires 2 nurse check For NSTEMI, Anticoagulant. Venous thromboembolism prophylaxis Anticoagulant Requires 2 nurse check Requires 2 nurse check. Hydrochlorothiazide (Hydrodiuril) 25 mg tab daily Hypertension, and also edema associated with CHF Check BP before giving Hydrocodone – acetaminophen (Norco) 7.5 - 325 mg tab 1-2 Tabs, every 4 hrs PRN 10 – 325 mg tab 1 Tab, every 4 hrs PRN 7.5 – 325 mg tab 1 Tab, every 4 hrs PRN 7.5-325 mg tab 1-2 Tabs, every 4 hrs PRN 5 – 325 mg tab 1 Tab, every 4 hrs PRN 10 – 325 mg tab 1 Tab, every 4 hrs PRN 7.5 – 325 mg tab 1 Tab, every 4 hrs PRN 5 – 325 mg tab 1-2 Tab, every 4 hrs PRN Mod pain (4 – 6) 1 tab, severe pain (7-10) 2 tabs Don’t exceed 4,000 mg of acetaminophen per day from all sources Mod pain (4 – 6) Don’t exceed 4,000 mg of acetaminophen per day from all sources Mild pain (1-3) Don’t exceed 4,000 mg of acetaminophen per day from all sources Mild pain (1-3) 1 tab, Mod pain (4 – 6) 2 tabs Don’t exceed 4,000 mg of acetaminophen per day from all sources Mild pain (1-3) Don’t exceed 4,000 mg of acetaminophen per day from all sources Mod pain (4 – 6) Don’t exceed 4,000 mg of acetaminophen per day from all sources Mild pain (1-3) Don’t exceed 4,000 mg of acetaminophen per day from all sources Mild pain (1-3), Mod pain (4-6) Don’t exceed 4,000 mg of acetaminophen per day from all sources. If an injectable analgesic is concurrently ordered for the same severity of pain, use oral when patient is consistently tolerating oral intake. Do not exceed 4,000 mg of acetaminophen per day from all sources. If an injectable analgesic is concurrently ordered for the same severity of pain, use oral when patient is consistently tolerating oral intake. Apply to left chest wall rash as needed. Hydrocodone – acetaminophen (Norco) Hydrocodone – acetaminophen (Norco) Hydrocodone – acetaminophen (Norco) Hydrocodone – acetaminophen (Norco) Hydrocodone – acetaminophen (Norco) Hydrocodone – acetaminophen (Norco) Hydrocodone – acetaminophen (Norco) Hydrocodone – acetaminophen (Norco) 5-325 mg tab 1 tab, every 4 hrs PRN Mild pain (1-3) Hydrocortisone (Cortizone-10) 1% topical cream, 2x/day PRN 1 mg/1 mL, IV, every 3 hrs PRN Skin rash Hydromorphone (Dilaudid) injection Severe pain (7-10) Hydromorphone (Dilaudid) injection 1 mg IV, every 4 hrs PRN Severe pain (7-10) Hydromorphone (Dilaudid) injection 2 mg IV, 2x/day PRN Severe pain (7-10) Hydromorphone (Dilaudid) injection 1.5 mg IV, every 2 hrs PRN Severe pain (7-10) Hydromorphone (Dilaudid) injection 1 mg IV, every 2 hrs PRN Moderate pain (4 – 6), if patient is not tolerating oral intake or if oral analgesics ineffective If an oral analgesic is concurrently ordered for the same severity of pain, only use injectable route if patient is not tolerating oral intake or if oral analgesics are ineffective. If oral analgesic is concurrently ordered for same severity of pain, only use injectable route if pt. is not tolerating oral intake or if oral analgesics ineffective. Premedicate for dosage change. If oral analgesic is concurrently ordered for same severity of pain, only use injectable route if pt. is not tolerating oral intake or if oral analgesics ineffective. If oral analgesic is concurrently ordered for same severity of pain, only use injectable route if pt. is not tolerating oral intake or if oral analgesics ineffective. If oral analgesic is concurrently ordered for same severity of pain, only use injectable route if pt. is not tolerating oral intake or if oral analgesics ineffective. 0.5 mg IV, every 4 hrs PRN Moderate pain (4 – 6) Hydroxyzine (atarax) 25 mg tab every 6 hrs prn Itching Insulin glargine (Lantus) 100 unit/mL injection 10 units 10 units, SubQ, daily @ 0900 Glucose control, Steroid induced diabetes (solumedrol) Insulin glargine (Lantus) 100 unit/mL injection 16 units 16 units, SubQ, daily at bedtime Type 2 diabetes Insulin Lispro (Humalog) 100 unit/mL injection 1-6 Units 1 – 6 Units SubQ, every 6 hrs per correction scale, due @1200 2 – 12 Units SubQ, QID AC & HS PRN for elevated glucose per correction scale 2 – 12 Units SubQ, every 6 hours PRN for elevated glucose per correction scale 2 – 12 Units SubQ, 4x/day – before meals & at bedtime. Due @ 0800 & 1200. For elevated glucose per correction scale 2 – 12 Units SubQ, 4x/day – before meals & at bedtime. Due @ 0800 & 1100. 2-12 units SubQ every 6 hrs PRN Type 2 diabetes Hydromorphone (Dilaudid) injection Insulin Lispro (Humalog) 100 unit/mL injection 2-12 Units Insulin Lispro (Humalog) 100 unit/mL injection 2-12 Units Insulin Lispro (Humalog) 100 unit/mL injection 2-12 Units Insulin Lispro (Humalog) 100 unit/mL injection 2-12 Units Insulin regular human (NovoLin R, HumuLIN R), 100 unit/mL, injection 2-12 units If oral analgesic is concurrently ordered for same severity of pain, only use injectable route if pt. is not tolerating oral intake or if oral analgesics ineffective. Drowsiness To be given when insulin drip discontinued. Long acting insulin, duration up to 24 hrs. If patient becomes NPO or other nutrition is interrupted for more than 1 hr or a bolus feeding is missed, contact physician for orders which may include insulin dose reduction, addition of D10 infusion, and more frequent glucose monitoring. Long acting insulin, duration up to 24 hrs. If patient becomes NPO or other nutrition is interrupted for more than 1 hr or a bolus feeding is missed, contact physician for orders which may include insulin dose reduction, addition of D10 infusion, and more frequent glucose monitoring. 2 nurse check. Use correction scale. Call MD if glucose greater than 400 mg/dL Type 2 diabetes 2 nurse check. Use correction scale. Type 2 diabetes 2 nurse check. Use correction scale. Type 2 diabetes 2 nurse check. Use correction scale. Type 2 diabetes 2 nurse check. Use correction scale. For elevated blood glucose per correction scale. Type 2 DM. Requires 2 nurse check. BG 151-200 = 2 units, BG 201-250 = 4 units, BG 251-300 = 6 units, BG 301-350 = 8 units, BG 351-400 = 10 units, BG > 400 = 12 units and call MD Insulin regular human (NovoLin R, HumuLIN R), 100 units in NS 100 mL drip 1-5 units/hr, 15mL/hr, continuous IV drip Glucose control, Steroid induced diabetes (solumedrol) Insulin regular human U-500 “Concentrated” (HumuLIN R U-500 “concentrated”), 500 unit/mL 40 Units, SubQ, 3x/day before meals Type 2 Diabetes Insulin regular human U-500 “Concentrated” (HumuLIN R U-500 “concentrated”), 500 unit/mL 5-15 Units, SubQ, 3x/day before meals as needed Type 2 Diabetes Insulin regular human U-500 “Concentrated” (HumuLIN R U-500 “concentrated”), 500 unit/mL Ipratropium – albuterol (Duo-neb) 0.5 mg3mg (2.5 mg base/ 3 mL nebulizer soln Ipratropium – albuterol (Duo-neb) 0.5 mg3mg (2.5 mg base/ 3 mL nebulizer soln 5-15 Units, SubQ, HS PRN Type 2 Diabetes 3 mL nebulizer 4x/day, due @ 0800 & 1200. RT Admin 3 mL nebulizer every 4 hrs, due @ 0800 & 1200. RT Admin 0.02% nebulizer soln 0.5 mg every 4 hrs 0.02% nebulizer soln 0.5 mg every 2 hrs PRN 0.02% nebulizer soln 0.5 mg every 4 hrs @ 0815 and 1215 0.02% nebulizer soln 0.5 mg PRN conditional: dyspnea 10 mg PO 4x/day Wheezing, shortness of breath Administered by Respiratory Therapist Wheezing, shortness of breath Administered by Respiratory Therapist COPD, bronchodilator Administered by Respiratory Therapist Wheezing, shortness of breath Administered by Respiratory Therapist Acute respiratory failure (interstitial lung disease) Shortness of breath, bronchodilator Administered by Respiratory Therapist Dyspnea, Acute respiratory failure, ARDS, bronchodilator Administered by Respiratory Therapist Nitrate vasodilator, Antianginal Adverse effects: light headedness, flushing. Ketorolac (Toradol) 30 mg IV every 6 hrs PRN Mild pain (1 – 3), Mod pain (4 – 6) Labetalol (Normodyne) 20 mg IV every 4 hrs PRN Hypertension, SBP >140 Ipratropium (Atrovent) Ipratropium (Atrovent) Ipratropium (Atrovent) Ipratropium (Atrovent) Isosorbide Dinitrate Requires 2 nurse check. Same caution as above. BG < 180 = 0 units/hr, BG 181-200 = 1 unit/hr, BG 201-250 = 2 units/hr, BG 251-300 = 3 units/hr, BG 301-400 = 4 units/hr, BG > 400 = 5 units/hr (on care planning day insulin was not being titrated according to this scale). Requires 2 nurse check. Caution: Insulin U-500 is five times more concentrated than insulin U100. 40 units U-500 equals 8 units marking on U-100 syringe (Blood sugar 100 or higher). If blood sugar less than 100 mg/dl, give 25 units U-500, equals 5 units marking on U-100 syringe. If pt. is NPO, HOLD insulin. Requires 2 nurse check. Same caution as above. If glucose 200-300, give 5 units, U-500 equals 1 unit marking on U-100 syringe. If glucose 301-400, give 10 units U-500 equals 2 unit marking on U-100 syringe. If over 400, give 15 units U-500 equals 3 unit marking on U-100 syringe. Requires 2 nurse check. For elevated blood sugar per correction scale at 2100. Same caution and instructions as immediately above. For systolic greater than 140. Check to see if other antihypertensive administered. Lansoprazole (Prevacid) 30 mg soluble tab, via NG tube @ 0700 GI Prophylaxis Levalbuterol (Xopenex) 1.25 mg/0.5 mL nebulizer soln @ 0800 and 1200 1,000 mg in D5W 100 mL, 2x/day, @ 0900, infuse over 15 mins 500 mg tab 2x/day, due @ 0900 Acute respiratory failure (interstitial lung disease) Levetiracetam (Keppra) Levetiracetam (Keppra) Levothyroxine (Synthroid) Levothyroxine (Synthroid) Lidocaine – D5W 4 mg/mL (0.4%) drip (conc: 4000 mcg/mL Lidocaine (Xylocaine) Lidocaine 1% (Xylocaine) 125 mcg tab before breakfast 300 mcg tab before breakfast @ 0700 Dose: 1 mg/min, 15 mL/hr, IV PRN conditional 100 mg/5 mL (2%) prefill syringe 75 mg Dose: 75 mg IV PRN conditional. 3.75 mL = 75 mg of 100 mg/5 mL Before breakfast. Per P&T approved policy, automatically substituted for protonix 40 mg d/t NG tube. Plasma half-life 1 ½ -2hr. Adverse Reactions: CVA, MI, shock, hematuria, hemolysis . Administered by Respiratory Therapist Prevention of epileptic seizures (anticonvulsant). Inhibtis complex partial seizures and prevents epileptic and seizure activity Contraindications: suicidal ideation; Cautious use: history of psychosis or depression, suicidal tendencies. Peak: 1hr, Half-life: 7.1 hr. Prevention of epileptic seizures (anticonvulsant). Inhibits complex partial seizures and prevents epileptic and seizure activity Hypothyroidism Contraindications: suicidal ideation; Cautious use: history of psychosis or depression, suicidal tendencies. Peak: 1hr, Half-life: 7.1 hr. Hyponatremia and Hypothyroidism Ventricular tachycardia For sustained ventricular tachycardia (class IB antiarrhythmic). Surpresses automaticity in His-Purkinje system. Inhibits sodium influx into myocardial cells, elevates electrical stimulation threshold of ventricle during diastole. 0.1 mL, once For use by RT (as needed prior to drawing ABG) Lorazepam (Ativan) 1 – 2 mg IV every 4 hrs PRN Agitation, seizures, tremor, give for withdrawal symptoms Lorazepam (Ativan) 1 mg IV every 6 hrs PRN Anxiety, agitation, seizures, tremor, history of methamphetamine use. Lorazepam (Ativan) 2 mg IV every 2 hrs PRN Anxiety, Agitation Contraindications: severe cardiovascular conditions, acute MI. Cautious: cardiac disease, angina pectoris, cardiac arrhythmias, older adult, impaired kidney function. Common adverse: insomnia. Other adverse: palpitations, tachycardia, arrhythmias, angina pectoris, hypertension Start after push for sustained ventricular tachycardia. Contraindications: supraventricular arrhythmias, untreated sinus bradycardia, severe degrees of sinoatrial, atrioventricular, and intraventricular heart block. Cautious use: Liver or kidney disease, CHF, shock, older adults. Onset: 45-90 sec IV, Duration 10-20 min IV, Half-life: 1.5-2 hr. Life threatening adverse effects: difficulty in breathing or swallowing; convulsions, respiratory distress (high doses); cardiovascular collapse, cardiac arrest. Administered by Respiratory Therapist Dilute with an equal amount of NS and give over 1 – 2 mins. Hold for any compromise of respirations; unarousable, alteration in mental status. Call MD immediately. Dilute with an equal amount of NS and give over 1 – 2 mins. Common adverse effects: drowsiness, sedation. Onset: 1-5 min IV, Duration: 12-24 hr Dilute with an equal amount of NS and give over 1 – 2 mins. Usual maximum dose per 12 hours: 8 mg. Hold for any compromise of respirations; unarousable, alteration in mental status. Call MD immediately. Lorazepam (Ativan) 2 mg IV every 1 hr PRN Anxiety, Agitation Dilute with an equal amount of NS and give over 1 – 2 mins. Losartan (Cozaar) 50 mg tab daily @ 0900 CHF, HTN; angiotensin II receptor antagonist; antihypertensive Patient on ventilator, NG Tube. Hold for Systolic BP < 100. Peak: 6h, duration: 24 h, half-life: 1.5-2 h. Cautious use: patients on diuretics, heart failure Maalox TC (Loperamide) 15 mL PO every 4 hours PRN Concentrated oral liquid, 10 mL daily PRN Dose 2g, IVPB, over 1 hr, PRN conditional, for Mg 1.9-2.0 Indigestion Magnesium hydroxide (Milk of magnesia) Magnesium sulfate 2g in D5W 50 mL IVPB Magnesium sulfate 2g in D5W 50 mL IVPB Dose 2g, IVPB, over 1 hr, PRN conditional, for Mg 1.9-2.0 Magnesium sulfate 2g in D5W 50 mL IVPB Dose 2g, IVPB, over 1 hr, PRN conditional, for Mg 1.9-2.0 Magnesium sulfate 3g in D5W 100 mL IVPB Dose 3g, IVPB, over 90 mins, PRN conditional, for Mg 1.6-1.8 Dose 3g, IVPB, over 90 mins, PRN conditional, for Mg 1.6-1.8 Dose 4g, IVPB, over 2 hrs, PRN conditional, for Mg less than 1.6 Dose 4g, IVPB, over 2 hrs, PRN conditional, for Mg less than 1.6 12.5 mg tab 4x/day Magnesium sulfate 3g in D5W 100 mL IVPB Magnesium sulfate 4g in D5W 100 mL IVPB Magnesium sulfate 4g in D5W 100 mL IVPB Meclizine (Antivert) constipation Hypomagnesemia (electrolyte replacement) Hypomagnesemia (electrolyte replacement) Hypomagnesemia (electrolyte replacement) 10 mL concentrate equivalent to 30 mL MOM Contraindications: myocardial damage; AV heart block; cardiac arrest except for certain arrhythmias. Cautious: renal disease, renal failure, renal impairment; acute MI. Life threatening adverse effects: complete heart block, circulatory collapse, respiratory paralysis, flaccid paralysis Conditional, for Mg 1.9-2.0, admin over 1 hour. Contraindications: myocardial damage; AV heart block; cardiac arrest except for certain arrhythmias. Cautious: renal disease, renal failure, renal impairment; acute MI. Life threatening adverse effects: complete heart block, circulatory collapse, respiratory paralysis, flaccid paralysis Contraindications: myocardial damage; AV heart block; cardiac arrest except for certain arrhythmias. Cautious: renal disease, renal failure, renal impairment; acute MI. Life threatening adverse effects: complete heart block, circulatory collapse, respiratory paralysis, flaccid paralysis Hypomagnesemia Hypomagnesemia Conditional, for Mg 1.6-1.8, admin over 90 mins. Hypomagnesemia Hypomagnesemia Nausea/vomiting and dizziness (antihistamine) Conditional, for Mg less than 1.6, admin over 2 hours Contraindicated for GI obstruction or ileus Meperidine PF (Demerol) 100 mg every 4 hrs PRN IVPB Shivering Meropenem (Merrem) 1g in NS 100 mL IVPB every 12 hrs @ 0900 Methylprednisolone PF (Solu-medrol) Methylprednisolone PF (Solu-medrol) 40 mg IV every 6 hrs taper @0700, 1300 40 mg IV every 12 hrs @ 0630 Antibiotic, for respiratory culture positive for gram pos cocci and gram neg bacilli. Broad-spectrum carbapenem antibiotic that inhibits cell wall synthesis of bacteria by its strong affinity for penicillin binding proteins of bacterial cell wall. Effective against both gram pos and gram neg bacteria. Anti-inflammatory agent for COPD (bronchial asthma) Methylprednisolone PF (Solu-medrol) 40 mg IV every 12 hrs @ 0900 Metoclopramide (Reglan) Metoclopramide (Reglan) 10 mg tab every 6 hrs PRN 10 mg IV every 6 hrs Metoclopramide (Reglan) 10 mg IV every 12 hrs @ 0830 If an oral analgesic is concurrently ordered for the same severity of pain, only use injectable route if patient is not tolerating oral intake or if oral analgesics are ineffective.. Adjusted based on estimated CI = 41 ml/min from Vancomycin Acute respiratory failure (interstitial lung disease). Has anti-inflammatory and immunosuppressive properties. For COPD. Has antiinflammatory and immunosuppressive properties. Anti-inflammatory agent for COPD (bronchial asthma) Nausea Led to steroid induced diabetes mellitus in this patient. Nausea IV Administration: Doses > 10 mg – Dilute in 50 mls D5W or NS and infuse over 15 minutes Nausea IV Administration: Doses > 10 mg – Dilute in 50 mls D5W or NS and infuse over 15 minutes Metolazone (Zaroxolyn) 10 mg tab @ 0900 Metoprolol (Lopressor) 5 mg IV every 4 hrs PRN Atrial fibrillation, CHF, HTN For heart rate > 110, administer over 1 minute Metoprolol (Lopressor) 12.5 mg tab, 2x/day, @0900 Hold for HR < 50, Hold for systolic BP < 100, administer with food if not NPO. Cautious use: major depression. Life threatening effects: laryngospasms, complete heart block, cardiac arrest. Onset: 15 min, Peak: 20 min IV, Duration 13-19 hr, Half-life: 3-4 hr. Metoprolol (Lopressor) 5 mg IVP slowly every 5 mins x3 doses total 50 mg PO every 12 hrs Blood pressure/hypertension management, replacement med for Nicardipine. Beta-adrenergic antagonist with preferential effect on beta1 receptors located primarily on cardiac muscle. Reduces HR and cardiac output at rest, lowers BP. Acute MI, HTN management. (Antihypertensive, Antianginal) Acute MI, HTN management Hold for HR < 60 or SBP < 110. HTN management Hold for HR < 60 or Systolic BP < 100. Admin with food if not NPO. Hypertension management, long term treatment of angina pectoris reduce risk of mortality after Hold for heart rate less than 60 bpm. Hold for Systolic BP less than 110 mmHg. Swallow whole, don’t crush or chew, tablet is scored Metoprolol (Lopressor) Metoprolol (Lopressor) Metoprolol ER (Toprol - XL) 50 mg tab PO 2x/day due @ 0900 50 mg tab daily Diuretic (thiazide like), for fluid volume overload, CHF Leads to elevated blood glucose Glucocorticoid. Patient also has Type 2 DM. Immunosuppressant. May be administered with food or milk. Only admin if not done in ED. Admin slowly. Hold for HR < 60 or SBP < 110. MI, migraine prophylaxis and may be split If goal RASS (Richmond Agitation Sedation Scale) not achieved: use up to 2 bolus doses before increasing rate by 1 mg/hr every 15m ins until goal RASS score achieved. If goal RASS surpassed: lower rate by 1 mg/hr every 15 mins until goal RASS score achieved. If at goal RASS score: continue current dose. Max dose: 12 mg/hr. Recommended max dose: 0.2 mg/kg/hr. Notify intensivist: if patient on max dose. Common adverse effects: retrograde amnesia; Life threatening adverse effects: laryngospasm, respiratory arrest. Onset: 1-5 min IV, peak: 20-60 min, Duration: less than 2hr IV. Admin IV push over 2-5 mins, every 5 mins up to 2 dosees PRN agitation before increasing continuous infusion rate. Admin IV push over 2-5 mins. Hold for Systolic BP < 100. Midazolam (Versed) 100 mg in D5W 100 mL continuous drip IV; dose: 1mg/hr. Held on care planning day (not needed) Agitation (CNS depressant with muscle relaxant, sedativehypnotic, anticonvulsant, and amnestic properties) Midazolam (Versed) 1 mg IV, every 5 mins PRN agitation Midazolam (Versed) 1 mg IV, every hrs PRN Midazolam (Versed) 100 mg in D5W 100 mL continuous drip IV; dose: 1mg/hr. 1mL/hr Not currently running. Agitation (CNS depressant with muscle relaxant, sedativehypnotic, anticonvulsant, and amnestic properties) Agitation (CNS depressant with muscle relaxant, sedativehypnotic, anticonvulsant, and amnestic properties) Midazolam (Versed) 1 mg IV, every 5 mins PRN agitation Midazolam (Versed) 100 mg in D5W 100 mL continuous drip IV; dose: 1mg/hr. 1mL/hr Agitation (CNS depressant with muscle relaxant, sedativehypnotic, anticonvulsant, and amnestic properties) Midazolam (Versed) 1 mg IV, every 5 mins PRN Agitation Midazolam (Versed) 100 mg in D5W 100 mL continuous drip IV; dose: Agitation (CNS depressant with muscle relaxant, sedativehypnotic, anticonvulsant, and amnestic properties) If goal RASS (Richmond Agitation Sedation Scale) not achieved: use up to 2 bolus doses before increasing rate by 1 mg/hr every 15 mins until goal RASS score achieved. If goal RASS surpassed: lower rate by 1 mg/hr every 15 mins until goal RASS score achieved. If at goal RASS score: continue current dose. Max dose: 12 mg/hr. Recommended max dose: 0.2 mg/kg/hr. Notify intensivist: if patient on max dose. Common adverse effects: retrograde amnesia; Life threatening adverse effects: laryngospasm, respiratory arrest. Onset: 1-5 min IV, peak: 20-60 min, Duration: less than 2hr IV. Admin IV push over 2-5 mins, every 5 mins up to 2 doses PRN agitation before increasing continuous infusion rate. If goal RASS (Richmond Agitation Sedation Scale) not achieved: use up to 2 bolus doses before increasing rate by 1 mg/hr every 15 mins until goal RASS score achieved. If goal RASS surpassed: lower rate by 1 mg/hr every 15 mins until goal RASS score achieved. If at goal RASS score: continue current dose. Max dose: 12 mg/hr. Recommended max dose: 0.2 mg/kg/hr. Notify intensivist: if patient on max dose. Common adverse effects: retrograde amnesia; Life threatening adverse effects: laryngospasm, respiratory arrest. Onset: 1-5 min IV, peak: 20-60 min, Duration: less than 2hr IV. Every 5 mins up to 2 doses PRN agitation before increasing continuous infusion rate. Dose to be given from IV infusion pump. If goal RASS (Richmond Agitation Sedation Scale) not achieved: use up to 2 bolus doses before increasing rate by 1 mg/hr every 15 mins until goal RASS score achieved. If goal 1mg/hr. 1mL/hr RASS surpassed: lower rate by 1 mg/hr every 15 mins until goal RASS score achieved. If at goal RASS score: continue current dose. Max dose: 12 mg/hr. Recommended max dose: 0.2 mg/kg/hr. Notify intensivist: if patient on max dose. Common adverse effects: retrograde amnesia; Life threatening adverse effects: laryngospasm, respiratory arrest. Onset: 1-5 min IV, peak: 20-60 min, Duration: less than 2hr IV. Every 5 mins up to 2 doses PRN agitation before increasing continuous infusion rate. Dose to be given from IV infusion pump. Midazolam (Versed) 1 mg IV, every 5 mins PRN Agitation Milk of magnesia (magnesium hydroxide) Morphine 30 mL PO daily PRN Constipation 1 – 2 mg IV every 3 hrs PRN 1-4 mg IVP every 5 minutes Mod pain (4-6), severe pain (710) For angina not relieved by Nitroglycerin Hold for SBP less than 90 Morphine ER (MS Contin) 45 mg tab every 8 hrs Pain Swallow whole. Do not crush, chew, or split. Morphine injection 4 mg IV every 3 hrs PRN 2 mg mod pain (4-6), 4 mg severe pain (7-10), for breakthrough pain. Morphine injection 4-6 mg IV every 4 hrs PRN Mod pain (4 – 6) 4 mg, severe pain (7-10) 6 mg If an oral analgesic is concurrently ordered for the same severity of pain, only use injectable route if patient is not tolerating oral intake or if oral analgesics are ineffective. Only use injectable route if patient isn’t tolerating oral intake or if oral analgesics ineffective (see: Norco) Morphine injection 2 mg IV, every 3 hrs PRN Mod pain (4-6), severe pain (710) Morphine injection 2 mg IV, every 5 mins PRN Mild pain (1-3), Mod pain (4-6), severe pain (7-10) Morphine injection 2 mg IV, every 2 hrs PRN Mod pain (4-6), severe pain (710) Morphine injection 2 mg IV, every 1 hr PRN Mod pain (4-6), severe pain (710) Morphine injection 1 mg IV, every 4 hrs PRN Mod pain (4-6), severe pain (710) Naloxone (Narcan) 0.2 mg IV every 1 min PRN Nicardipine (Cardene) Dose: 2.5 mg/hr; 50 mg in NS 250 mL drip, continuous drip To counteract morphine overdose. As needed x5 doses, to increase patient alertness and respiratory rate to greater than 10/min As needed to keep Systolic BP under 140. Calcium channel blocker. Significantly decreases systemic vascular resistance; reduces BP. Morphine Maximum dose = 10 mg. Agent A: give in PACU ONLY, discontinue on transfer from PACU. If an oral analgesic is concurrently ordered for the same severity of pain, only use injectable route if patient is not tolerating oral intake or if oral analgesics are ineffective. . Hold for Systolic BP < 100. If an oral analgesic is concurrently ordered for the same severity of pain, only use injectable route if patient is not tolerating oral intake or if oral analgesics are ineffective. If an oral analgesic is concurrently ordered for the same severity of pain, only use injectable route if patient is not tolerating oral intake or if oral analgesics are ineffective. If patient difficult to arouse and/or resp rate less than 10/min. If 0.1 and 0.2 mg/mL concentration are administered through a large peripheral vein, change the infusion site every 12 hours. Onset: 1 min IV, Peak: 0.5-2 hr, Duration: 3 hr IV, Half-life: 8.6 hr. Nicotine (Nicoderm) 21 mg/24 hr transdermal patch Nitroglycerin Nitroglycerin Nitroglycerin SL (Nitrostat) Nitroglycerin SL (Nitrostat) Nitropaste Norepinephrine (Levophed) 8,000 mcg in D5W 250 mL drip Norepinephrine (Levophed) 8,000 mcg in D5W 250 mL drip NS 1,000 mL IV soln NS 1,000 mL IV soln NS 1,000 mL IV soln NS 1,000 mL IV soln NS 500 mL IV soln NS with KCL 20 mEq/L IV soln NS with KCL 20 mEq/L IV soln NS with KCL 20 mEq/L IV soln Nystatin (Mycostatin) topical powder 1 patch Tobacco user Apply to hairless, clean, dry area of upper arm or hip 50 mg/250mL D5W IV at 5mcg/minute 0.4 mg SL for chest pain PRN. May repeat 3x every 5 mins 0.4 mg sublingual every 5 minutes PRN 0.4 mg sublingual every 5 minutes PRN 1” topically 3x/ day Chest pain. Antianginal, vasodilator Titrate for chest pain with SBP greater than 90 Chest pain. Antianginal, vasodilator May repeat 3x every 5 mins. Call healthcare provider if chest pain unrelieved by nitroglycerin Chest pain (Antianginal, vasodilator) Dissolve under tongue Chest pain (Antianginal, vasodilator) Dissolve under tongue Antianginal, vasodilator Hold for SBP < 110 Dose: 2 mcg/min, 3.75 mL/hr IV continuous drip (32 mcg/mL) Dose: 2 mcg/min, 3.75 mL/hr IV continuous drip (32 mcg/mL) 50 mL/hr continuous IV infusion 75 mL/hr continuous IV infusion 1,000 mL, 125 mL/hr continuous IV 100 mL/hr continuous IV infusion 20 mL/hr continuous IV infusion 1,000 mL, 100 mL/hr IV continuous 1,000 mL, 75 mL/hr IV continuous; R. wrist 20 g 1,000 mL, 40 mL/hr IV continuous 1 application, 2x/day, due @ 0900 Low blood pressure and heart failure, sepsis. Low blood pressure, sepsis. Vesicant (skin, eye, mucosal pain/irritation) Titrate to keep MAP > 65. Vesicant (skin, eye, mucosal pain/irritation) Fluid intake Hypervolemia Fluid intake Hypervolemia Fluid intake Fluid intake Hypervolemia Fluid intake Hypervolemia Fluid intake and electrolyte balance Fluid intake and electrolyte balance Keep patient euvolemic and minimize IV fluids if possible per neurosurgery. Fluid intake and electrolyte balance Antifungal antibiotic; Candida infection Apply to pannus, groin Ondansetron (Zofran) 4 mg/2 mL, IV, every 8 hrs PRN 4 mg IV , every 6 hrs PRN Nausea/vomiting May repeat x1 after 30 mins Nausea/vomiting Dizziness Ondansetron (Zofran) 4 mg IV every 4 hrs PRN Nausea/vomiting May repeat x1 after 30 mins Ondansetron (Zofran) 4 mg/2mL IV , every 6 hrs PRN 4 mg/2 mL, IV, every 8 hrs PRN Dose 1-2 tab every 6 hrs PRN Nausea/vomiting Dizziness, headache, sedation, diarrhea are common adverse side effects. Peak: 1-1.5 hr, half-life: 3 hr. May repeat x1 after 30 mins. Dizziness. Peak: 1-1.5 hr, half-life: 3 hr. Ondansetron (Zofran) Ondansetron (Zofran) Oxycodone acetaminophen (Percocet) 5-325 mg tab Nausea/vomiting For moderate to severe breakthrough pain Do not exceed 4,000 mg of acetaminophen per day from all sources. If an injectable analgesic is concurrently ordered for the same severity of pain, use oral when patient is consistently tolerating oral intake. 1 tab for moderate pain, 2 tabs for severe pain. Therapeutic substitution with formulary agent per P&T committee. Substituted for Percocet 2.5-325 mg tab. Do not exceed 4,000 mg of acetaminophen per day from all sources. If an injectable analgesic is concurrently ordered for the same severity of pain, use oral when patient is consistently tolerating oral intake. Dilute in 10 mL of NS and admin over a minimum of 2 mins. Oxycodone acetaminophen (Percocet) 7.5-325 mg tab 2 tab, every 4 hrs PRN Mild pain (1-3), mod pain (4-6) Pantoprazole (Protonix) 40 mg IV daily @ 0900 GI prophylaxis Pantoprazole (Protonix) 40 mg IV every 12 hrs GI prophylaxis Dilute in 10 mL of NS and admin over a minimum of 2 mins. Pantoprazole EC (Protonix) 40 mg tab daily GI prophylaxis (Antiulcer, proton pump inhibitor) Swallow whole. Do not crush, chew, or split Pantoprazole EC (Protonix) 20 mg tab daily @ 0900 GI prophylaxis (Antiulcer, proton pump inhibitor) Swallow whole. Do not crush, chew, or split Piperacillin – tazobactam (Zosyn) 3.375 g in D5W 100 mL IVPB @ 200 mL/hr every 6 hrs 3.375 g in D5W 100 mL IVPB @ 200 mL/hr every 6 hrs, due @ 1045 Antibiotic Piperacillin – tazobactam (Zosyn) Piperacillin – tazobactam (Zosyn) 3.375 g in D5W 100 mL IVPB @ 200 mL/hr every 6 hrs, due @ 1200 Antibiotic; two drug combination has antibiotic activity against an extremely broad spectrum of gram-positive, gram-negative, and anaerobic bacteria. Tazobactam extends the spectrum of bacteria susceptible to piperacillin. Heavy growth of multiple colony types of gram negative bacilli, clinical significance uncertain. Possible aspiration pneumonia. Antibiotic; two drug combination has antibiotic activity against an extremely broad spectrum of gram-positive, gram-negative, and anaerobic bacteria. Tazobactam extends the Infuse over 30 mins. Life threatening adverse effect: pseudomembranous colitis. Infuse over 30 mins @ 200 mL/hr. Life threatening adverse effect: pseudomembranous colitis. Pneumococcal vaccine (Pneumovax 23) Pneumococcal vaccine (Pneumovax) 0.5 mL IM PRN conditional Polyethylene glycol (Miralax) 17g oral packet, daily PRN 1.4% opthalmic soln 1 drop, both eyes, every 4 hours Dose: 20 mEq/100 mL, IV, PRN conditional, 20 mEq = 100 mL Dose: 40 mEq tab daily @ 0900 Dose: 10 mEq, IV, PRN conditional, 10 mEq = 100 mL Dose: 10 mEq, IV, PRN conditional, 10 mEq = 100 mL 25 mg rectal suppository every 12 hrs PRN 10 mg tab every 6 hrs PRN 12.5 mg IV/PO every 4-6 hours PRN 5 mcg/kg/min x 90.3 kg, Admin dose: 451.5 mcg/min: 2.71 mL/hr continuous, 10mg/mL drip Polyvinyl alcohol (Teargen) Potassium chloride Potassium chloride (K-Dur) Potassium chloride 10 mEq/100 mL Potassium chloride 10 mEq/100 mL Prochlorperazine (Compazine) Prochlorperazine (Compazine) Promethazine Propofol (Diprivan) spectrum of bacteria susceptible to piperacillin. Heavy growth of multiple colony types of gram negative bacilli, clinical significance uncertain. Patient has Health Care Associated Pneumonia. Vaccine 0.5 mL IM Vaccine Constipation Indicated per screening. Consider subQ admin if patient anticoagulated Prior to discharge, admin when pt. temp is less than 100.4 Dissolve in 4 to 8 ounces of liquid; give only if no BM today, use as PRN for constipation. 1 fl. Oz. = 30 mL Artificial tears Hypokalemia Infuse each 20 mEq over 1 hr. Use correction scale in MAR Hypokalemia Swallow whole. Don’t crush or chew. Scored tablet may be split. Hypokalemia Infuse each 10 mEq over 1 hr. Use correction scale Hypokalemia Daily PRN. Infuse each 10 mEq over 1 hr. Use correction scale in MAR. nausea nausea Nausea Agitation, sedation, general anesthesia. 5 mcg/kg/min is for conscious sedation of an adult. Used in induction and maintenance of anesthesia or sedation. Life threatening adverse effects: respiratory depression, apnea, Leukopenia, agranulocytosis If Goal RASS not achieved: Use up to 2 bolus doses before increasing rate by 5 mcg/kg/min every 15 mins until goal RASS score achieved. If goal RASS surpassed: Lower rate by 5 mcg/kig/min every 15 mins until goal RASS score achieved. If at goal RASS score: continue current dose. Maximum dose: 50 mcg/kg/min. Notify Intensivist: If patient on max dose. Notify Intensivist: If propofol continues greater than or equal to 72 hours to consider change to Versed. Contraindications: patients w/ increased intracranial pressure or impaired cerebral circulation. Onset: 9-36 sec, Duration: 6-10 mins, Half-Life: 5-12 hr. Propofol (Diprivan) Propranolol (Inderal) Pyridostigmine (Mestinon) Quetiapine (Seroquel) Quinapril (Accupril) 25 mg, every 5 mins PRN, 10 mg/mL drip 10 mg tab 60 mg tab, oral, every 8 hrs STD 300 mg tab daily Agitation Hypertension IV Push every 5 mins up to 2 doses PRN agitation before increasing continuous infusion rate. Hold for heart rate less than 60 bpm, hold for systolic BP less than 115 mmHg. Myasthenia gravis Add-on therapy for major depressive disorder, bipolar disorder ACE Inhibitor, anithypertensive 2.5 mg PO on admission, 20 mg daily Dose: 1 packet, 250 mg, NG Tube, 2x/day @ 0900 10 mL IV PRN conditional Treatment/prevention of diarrhea as a result of antibiotics (strain of yeast). Admin via NG Tube, however NG Tube was removed. Lock flush “Flush after each use and after blood draws. Use ONLY a 10cc syringe.” Saline lock flush 3 mL 3 mL IV Daily Lock flush, line patency Saline lock flush 3 mL 3 mL, daily, @ 0900 Lock flush, line patency Saline lock flush 3 mL 3 mL IV every 8 hrs. Lock flush, line patency Sennosides (Senokot) 2 tabs, 2x/day, @ 0900 Constipation (retains water in intestine) Simvastatin 10 mg PO daily at HS Sodium chloride tab 1 g tab, 4x/day @ 0800 & 1200 HMG-CoA reductase inhibitor (Statin), Antihyperlipemic. (increases HDL and decreases LDL cholesterol) Hyponatremia and hypochloride (fluid volume overload) Sodium hypochlorite (Dankin’s) 0.125% (1/4 strength) irrigation Sodium phosphate Topical, daily Saccharomyces boulardii (Florastore) packet 250 mg Saline lock flush 10 mL Sodium phosphate Sodium phosphate Sodium phosphate 15 mmol in NS 100 mL IVPB, PRN conditional 24 mmol in NS 100 mL IVPB, PRN conditional 36 mmol in NS 150 mL IVPB, PRN conditional 45 mmol in NS 150 mL IVPB, PRN conditional Infection, topical antiseptic Life threatening adverse effect: Angioedema And after each IV med for IV line patency. Use 10 mL for PICC, use 20 mL after blood or TPN 8.6 mg sennosides is equivalent to 187 mg senna. Onset: 2 week; Peak: 4-6 week. Avoid grapefruit. For irrigation use only. Electrolyte replacement For Phosphate of 2.0-2.3. Infuse slowly over 2 hrs. Electrolyte replacement For Phosphate of 1.6-1.9. Infuse slowly over 3 hrs. Electrolyte replacement For Phosphate of 1.0-1.5. Infuse slowly over 4 hrs. Electrolyte replacement For Phosphate less than 1.0-1.5. Infuse slowly over 5 hrs. Tamsulosin (Flomax) 0.4 mg cap daily Urination, Benign prostatic hypertrophy Temazepam (Restoril) 30 mg cap HS PRN Insomnia Temazepam (Restoril) 15 mg PO at bedtime PRN Sleep aid, Insomnia Therapeutic multivitamin (Theravite) Therapeutic multivitamin (Theravite) Tolvaptan (Samsca) 1 tablet, daily Vitamin deficiency 1 tablet, daily, due @0900 Vitamin deficiency Administer 30 mins after a meal. Swallow whole, don’t crush, chew, or spit. May repeat x1 15 mg tab, daily @ 1200 Hyponatremia (associated with CHF), increases urine output. 50 mg tab every 4 hrs PRN 150 mg tab daily at bedtime Mild pain (1-3), Moderate pain (46) 0.1% topical cream, 3x/day Anti-inflammatory Apply to face and back Empiric Bactrim prophylaxis, Pneumocystis pneumonia (PCP) prophylaxis Dose in mgs represents trimethoprim component – Administer on an empty stomach 1 hour prior or 2 hrs after meals. Vancomycin (Vanconcin) 1,500 mg in D5W 300 mL IVPB Vancomycin dosing per pharmacy 1 each 160-800 mg tab, 1 tab, Mon Wed Fri, due @ 0900 1,250 mg in D5W 250 mL IVPB @ 167 mL/hr every 12 hrs 1,250 mg in NS 250 mL IVPB @ 167 mL/hr every 18 hrs @ 0200 1,000 mg in D5W 250 mL IVPB @ 250 mL/hr every 6 hrs, due @ 1200 1,500 mg, 200 mL/hr, IVPB, every 16 hrs 1 each, daily PRN, Vancomycin dosing per pharmacy 1 each 1 each, daily PRN, Tramadol (Ultram) Trazodone (Desyrel) Triamcinolone (Aristocort) Trimethoprim – sulfamethoxazole ds (Bactrim DS) Vancomycin (Vancocin) Vancomycin (Vancocin) Vancomycin (Vancocin) Water (Free water) 200 mL every 8 hrs via NG Tube @ 1245 Patient should NOT be on fluid restriction for the first 24 hrs of therapy. Hold for sodium greater than 140 or sodium increase greater than or equal to 12 meq/L per 24 hr period. Request from pharmacy. Potassium checks every 12 hrs. Major depression (Antidepressant) Antibiotic Antibiotic, for respiratory culture positive for gram pos cocci and gram neg bacilli. Inhibits bacterial wall synthesis. Life threatening adverse effects: Nephrotoxicity, fatal uremia, Anaphylaxis, Leukopenia. Peak: 30 mins after end of infusion, half-life: 4-8 hrs. Antibiotic Life threatening adverse effects: Nephrotoxicity, fatal uremia, Anaphylaxis, Leukopenia. Peak: 30 mins after end of infusion, half-life: 4-8 hrs. Antibiotic Antibiotic Needs pharmacy consult Antibiotic, for respiratory culture positive for gram pos cocci and gram neg bacilli. Hypernatremia Needs pharmacy consult Admin via NG Tube Water (Free water) Zinc sulfate (Orazinc) Zolpidem (Ambien) 200 mL oral every 6 hrs due @ 1000 and @1600 220 mg tab, daily 5 mg tab HS PRN Fluid intake Nursing to chart on MAR and record intake on the Doc Flow sheet. Zinc deficiency Insomnia Do not give after 2400