Source Documentation
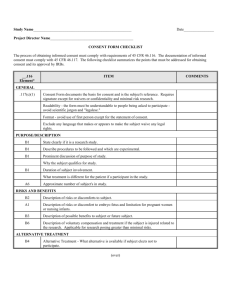
advertisement
Source Documentation Source Documentation Objectives: At the conclusion of this discussion, participants will be able to: – Define source document and source data – Identify what data from nuclear medicine is considered to be source data – Define the acronym “ALCOA” and what it means to the FDA and sponsor – Understand the difference between the source document and the Case Report Form (CRF) – Document the informed consent process as required by 21CFR312 and GCP Source Data: GCP Definition 1.51 Source Data: All information in original records and certified copies of original records of clinical findings, observations, or other activities in a clinical trial necessary for the reconstruction and evaluation of the trial. Source data are contained in source documents (original records or certified copies). Source Document: GCP Definition 1.52 Source Documents: Original documents, data, and records (e.g., hospital records, clinical and office charts, laboratory notes, memoranda, subjects' diaries or evaluation checklists, pharmacy dispensing records, recorded data from automated instruments, copies or transcriptions certified after verification as being accurate and complete, microfiches, photographic negatives, microfilm or magnetic media, x-rays, subject files, and records kept at the pharmacy, at the laboratories, and at medico-technical departments involved in the clinical trial). Practical Definition • • • • • • • The FIRST place you write something down All scan data, in DICOM or printed format All radiopharmacy records Well counter print-outs Documents that you sign Worksheets and logs Notes about the patient ANYWHERE The FIRST Place…scenarios • You go back to the hot lab to assay the residual activity in the syringe after injection. You write the activity and time down….where? • You get a phone call about the patient’s creatinine level. You write it down…where? • You inject at 11:06, and start scanning at 12:22. You write it down…where? • You are taking vital signs. You take three blood pressures because the first one was just after the patient laid down and it was high. You write this down…where? Where NOT to Write • Your hand • A scrap of paper in your lab coat pocket • A document that has information about another patient Where TO Write • Worksheet provided by the sponsor • Data sheet created for a specific purpose • Blank sheet of paper for that patient But Just in Case… • If you write on a scrap paper, sign and date it, include it in the case record. • If you write on a piece of paper that relates to another patient, write an explanation on the paper, sign and date it, and include it in the case record. • If you write on your hand, never wash it again, and present your hand to the FDA at inspection which will take place 2-5 years later. What is the Big Deal? Good source document “hygiene” prevents: • Transcription errors • Memory lapses • Recreating data points to fit a predetermined idea • The appearance of fraud ALCOA principle • • • • • Attributable Legible Contemporaneous Original Accurate Attributable • Who wrote it? • Is this person authorized by the Principal Investigator to perform clinical trial duties? • What are this person’s credentials for recording the data? • Will you know who wrote this down in 10 years? Delegation of Responsibility Log Sample provided by Cellectar, Inc. Legible • To be avoided….”What does this say?” • Avoid nuclear medicine terms that don’t translate to all of medicine • Avoid departmental slang • Will you be able to interpret this in 10 years? Contemporaneous • Is the data being recorded at the time it is measured? • If there is a correction, when was the correction and by whom? • If there is a significant gap between the recording of the data and the gathering of the data, why? • Never ever ever back-date something…. Original • The FIRST place it was written down • Transcriptions are not original • CRFs are not original – 21CFR says CRFs are part of case history – Per GCP, CRFs should NOT be original recording – Industry standard: verify all CRF data with source document • Copies are not original – Copies can be altered Accurate • Don’t ever guess…. • Don’t ever guess… • Don’t ever guess… – The most well-intentioned guess can defeat a study. – Missing data points should be recorded as missing. • Are there conflicting data recorded elsewhere? Source Document Hygiene • Write in ink (never pencil or erasable ink) • Blue or black is best (blue has advantages) • Never ever ever ever EVER use white-out • Correct errors and changes with the following technique: – Draw one line through the original entry – Write the correct entry beside the original – Initial and date the change – The original entry and the new entry should both be legible Examples of Corrections Scan Data as Source Documents • DICOM files – Time and date stamps – Isotope used – Parameters such as matrix, bed position, scan speed – Name of scan – Patient identifiers • Avoid distractions Equipment QC Documentation • Is your camera working like it’s supposed to? • Is your treadmill or glucometer or refrigerator or infusion pump calibrated? • Has your uniformity correction been done within the manufacturer’s recommended guidelines (or sponsor prescribed timeline)? • Is your energy correction accurate? • Did you perform daily QC, and did it meet predetermined specifications? Radiopharmacy Documentation • How long are your patient dosing logs kept? • Where is the dose calibrator QC kept? • Did you follow the sponsor’s protocol for assaying the dose before and after the injection? Dose Calibrators & Well Counters • Original print-outs are source documents • Annotate: Sign and Date Nuclear M. Technologist, 25 Jan 2010 Numbers on a Page • 82 – Pulse? – Respiration? – Systolic blood pressure? – Glucose level? – Age? – Millicuries? Microcuries? – Volume of urine sample? • Record full data, sign and date entries • Duplicate measurements okay; record accurately Forms, Worksheets, CRFs • Case Report Form (CRF) “A printed, optical, or electronic document designed to record all of the protocol-required information to be reported to the sponsor for each trial subject” “A record of clinical study observations and other information that a study protocol designates must be completed for each subject” • Provided by the sponsor • NOT source document (per industry standard and GCP) • Must be checked against the source document CDISC v. 8.0, 2009 Forms, Worksheets, CRFs • Worksheets – Frequently provided by sponsor – May look like copy of CRF – Should be signed and dated – Usually study-specific • Forms – Frequently provided by sponsor – May look like copy of CRF – Should be signed and dated – May be generalized to all studies for that company FDA Inspection Manual From the FDA Inspection Manual Source Documents a. Describe the investigator's source documents in terms of their organization, condition, completeness, and legibility. b. Determine whether there is adequate documentation to ensure that all subjects were alive and available for the duration of their stated participation in the study. From the FDA Inspection Manual c. Determine whether the records contain: – Observations, information, and data on the condition of the subject at the time of entry into the clinical study, as required by the protocol; – Documentation of the subject's exposure to the test article, as required by the protocol; – Observations and data on the condition of the subject throughout participation in the investigation, including results of lab tests, development of unrelated illness, and other factors which might alter the effects of the test article; and – Identification of key personnel involved in collecting and analyzing data at the site. From the FDA Inspection Manual Case Report Forms (CRFs) a. Describe the process for obtaining and recording information in CRFs. – Who obtained and recorded the information; – The source of the information (e.g., were data transcribed from another document or were data recorded directly onto the CRF); and – Whether corrections were made to the CRF data entries. If corrections were made, determine who made them, the reason(s) for the changes, and whether the clinical investigator was aware of these changes. From the FDA Inspection Manual b. Compare the source documents with the CRFs and any background information provided (e.g., data tabulations provided by the sponsor) per the assignment memorandum and sampling plan (if applicable). Determine whether: • The study subjects met the eligibility criteria (inclusion/exclusion); • Protocol-specified clinical laboratory testing (including EKGs, X-rays, eye exams, etc.) was documented by laboratory records; • All adverse events were documented and appropriately reported Case History Requirement 21CFR312.62(b): Case histories. An investigator is required to prepare and maintain adequate and accurate case histories that record all observations and other data pertinent to the investigation on each individual administered the investigational drug or employed as a control in the investigation. Case histories include the case report forms and supporting data including, for example, signed and dated consent forms and medical records including, for example, progress notes of the physician, the individual's hospital chart(s), and the nurses' notes. The case history for each individual shall document that informed consent was obtained prior to participation in the study. Key point: Case History The case history for each individual shall document that informed consent was obtained prior to participation in the study. • Clinic notes or nuclear medicine chart must provide documentation that the patient is willingly involved in the study, has had time to review the consent form, and has had an opportunity to ask questions and have their concerns addressed. • Forms and pre-printed clinic notes are okay, as long as they are signed and dated appropriately. Sample Documentation of Consent “The informed consent for the XXXXXX study was presented to the subject. The subject was given the opportunity to ask and have all questions answered. The consent form was signed and a copy was given to the subject.” (Signature/Date) Source Documentation Scenarios • You go back to the hot lab to assay the residual activity in the syringe after injection. You write the activity and time down….where? • You get a phone call about the patient’s creatinine level. You write it down…where? • You inject at 11:06, and start scanning at 12:22. You write it down…where? • You are taking vital signs. You take three blood pressures because the first one was just after the patient laid down and it was high. You write this down…where? References • FDA Inspection Manual http://www.fda.gov/downloads/ICECI/EnforcementActions/Bioresear chMonitoring/ucm133773.pdf • ICH GCP http://www.ich.org/cache/compo/276-254-1.html • 21CFR312 http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch. cfm?CFRPart=312 • CDISC Glossary http://appliedclinicaltrialsonline.findpharma.com/appliedclinicaltrials/ CRO%2FSponsor/CDISC-Clinical-ResearchGlossary/ArticleStandard/Article/detail/648647?ref=25