Chapter 16 - McGraw Hill Higher Education
advertisement

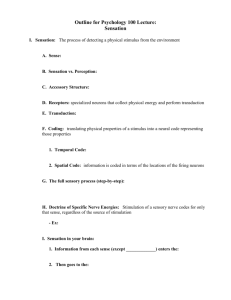
Chapter 16 Lecture Outline See PowerPoint Image Slides for all figures and tables pre-inserted into PowerPoint without notes. 16-1 Copyright (c) The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Sense Organs • Sensory receptors – properties and types • General senses • Chemical senses • Hearing and equilibrium • Vision 16-2 Properties of Receptors • Sensory transduction – convert stimulus energy into nerve energy • Receptor potential – local electrical change in receptor cell • Adaptation – conscious sensation declines with continued stimulation 16-3 Receptors Transmit Information 1. Modality - type of stimulus 2. Location – each sensory receptor receives input from its receptive field – sensory projection - brain identifies site of stimulation 3. Intensity – frequency, number of fibers and which fibers 4. Duration - change in firing frequency over time – phasic receptor - burst of activity and quickly adapt (smell and hair receptors) – tonic receptor - adapt slowly, generate impulses continually (proprioceptor) 16-4 Receptive Fields 16-5 Classification of Receptors • By modality: – chemo-, thermo-, mechano-, photo- receptors and nociceptors • By origin of stimuli – interoceptors - detect internal stimuli – proprioceptors - sense body position and movements – exteroceptors - detect external stimuli • By distribution – general senses - widely distributed – special senses - limited to head 16-6 Unencapsulated Nerve Endings • Dendrites not wrapped in connective tissue • General sense receptors – for pain and temperature • Tactile discs – associated with cells at base of epidermis • Hair receptors – monitor movement of hair 16-7 Encapsulated Nerve Endings • Dendrites wrapped by glial cells or connective tissue – tactile corpuscles - phasic • light touch and texture – krause end bulb - phasic • tactile; in mucous membranes – lamellated corpuscles - phasic • deep pressure, stretch, tickle and vibration – ruffini corpuscles - tonic • heavy touch, pressure, joint movements and skin stretching 16-8 Somesthetic Projection Pathways • 1st order neuron (afferent neuron) – from body, enter the dorsal horn of spinal cord via spinal nerves – from head, enter pons and medulla via cranial nerve – touch, pressure and proprioception on large, fast, myelinated axons – heat and cold on small, unmyelinated, slow fibers • 2nd order neuron – decussation to opposite side in spinal cord or medulla/pons – end in thalamus, except for proprioception (cerebellum) • 3rd order neuron – thalamus to primary somesthetic cortex of cerebrum 16-9 Pain • Nociceptors – allow awareness of tissue injuries – found in all tissues except the brain • Fast pain travels in myelinated fibers at 30 m/sec – sharp, localized, stabbing pain perceived with injury • Slow pain travels unmyelinated fibers at 2 m/sec – longer-lasting, dull, diffuse feeling • Somatic pain from skin, muscles and joints • Visceral pain from stretch, chemical irritants or ischemia of viscera (poorly localized) • Injured tissues release chemicals that stimulate pain fibers (bradykinin, histamine, prostaglandin) 16-10 Projection Pathway for Pain • General pathway – conscious pain – 1st order neuron cell bodies in dorsal root ganglion of spinal nerves or cranial nerves V, VII, IX, and X – 2nd order neurons decussate and send fibers up spinothalamic tract or through medulla to thalamus • gracile fasciculus carries visceral pain signals – 3rd order neurons from thalamus reach primary somesthetic cortex as sensory homunculus • Spinoreticular tract – pain signals reach reticular formation, hypothalamus and limbic – trigger visceral, emotional, and behavioral reactions 16-11 Pain Signal Destinations 16-12 Referred Pain • Misinterpreted pain – brain “assumes” visceral pain is coming from skin – heart pain felt in shoulder or arm because both send pain input to spinal cord segments T1 to T5 16-13 Referred Pain 16-14 CNS Modulation of Pain • Intensity of pain - affected by state of mind • Endogenous opiods (enkephalins, endorphins and dynorphins) – produced by CNS and other organs under stress – in dorsal horn of spinal cord (spinal gating) – act as neuromodulators block transmission of pain 16-15 Spinal Gating • Stops pain signals at dorsal horn – descending analgesic fibers from reticular formation travel down reticulospinal tract to dorsal horn • secrete inhibitory substances that block pain fibers from secreting substance P • pain signals never ascend – dorsal horn fibers inhibited by input from mechanoreceptors • rubbing a sore arm reduces pain 16-16 Spinal Gating of Pain Signals 16-17 Chemical Sense - Taste • Gustation - sensation of taste – results from action of chemicals on taste buds • Lingual papillae – filiform (no taste buds) • important for texture – foliate (no taste buds) – fungiform • at tips and sides of tongue – vallate (circumvallate) • at rear of tongue • contains 1/2 of taste buds 16-18 Taste Bud Structure • Taste cells – apical microvilli serve as receptor surface – synapse with sensory nerve fibers at their base • Supporting cells • Basal cells 16-19 Physiology of Taste • • Molecules must dissolve in saliva 5 primary sensations - throughout tongue 1. 2. 3. 4. 5. • Sweet - concentrated on tip Salty - lateral margins Sour - lateral margins Bitter - posterior Umami - taste of amino acids (MSG) Influenced by food texture, aroma, temperature, and appearance – mouthfeel - detected by lingual nerve in papillae • Hot pepper stimulates free nerve endings (pain) 16-20 Physiology of Taste • Mechanisms of action – activate 2nd messenger systems • sugars, alkaloids and glutamates bind to receptors – depolarize cells directly • sodium and acids penetrate cells 16-21 Projection Pathways for Taste • Innervation of taste buds – facial nerve (VII) - anterior 2/3’s of tongue – glossopharyngeal nerve (IX) - posterior 1/3 – vagus nerve (X) - palate, pharynx, epiglottis 16-22 Projection Pathways for Taste • To solitary nucleus in medulla • To hypothalamus and amygdala – activate autonomic reflexes • e.g. salivation, gagging and vomiting • To thalamus, then postcentral gyrus of cerebrum – conscious sense of taste 16-23 Chemical Sense - Smell • Olfactory mucosa – contains receptor cells for olfaction – highly sensitive • up to 10,000 odors – on 5cm2 of superior concha and nasal septum 16-24 Olfactory Epithelial Cells • Olfactory cells – olfactory hairs neurons with 20 cilia • bind odor molecules in thin layer of mucus – axons pass through cribriform plate – survive 60 days • Supporting cells • Basal cells – divide 16-25 Physiology of Smell • Molecules bind to receptor on olfactory hair – hydrophilic - diffuse through mucus – hydrophobic - transport by odorant-binding protein • Activate G protein and cAMP system • Opens ion channels for Na+ or Ca2+ – creates a receptor potential • Action potential travels to brain • Receptors adapt quickly – due to synaptic inhibition in olfactory bulbs 16-26 Olfactory Pathway • Olfactory cells synapse in olfactory bulb – on mitral and tufted cell dendrites – in spherical clusters called glomeruli • each glomeruli dedicated to single odor 16-27 Olfactory Pathway • Output from bulb forms olfactory tracts – end in primary olfactory cortex and thalamus – travel to insula and frontal cortex – identify odors – integrate taste and smell into flavor – travel to hypocampus, amygdala, and hypothalamus • memories, emotional and visceral reactions 16-28 Olfactory Pathway • Feedback – granule cells in olfactory cortex synapse in glomeruli • food smells better when hungry 16-29 Olfactory Projection Pathways 16-30 The Nature of Sound • Sound - audible vibration of molecules – vibrating object pushes air molecules 16-31 Pitch and Loudness • Pitch - frequency vibrates specific parts of ear – hearing range is 20 (low pitch) - 20,000 Hz (cycles/sec) – speech is 1500-4000 where hearing is most sensitive • Loudness – amplitude; intensity of sound energy 16-32 Outer Ear 16-33 Outer Ear • Fleshy auricle (pinna) directs air vibrations down external auditory meatus – cartilagenous and bony, S-shaped tunnel ending at eardrum – glandular secretions and dead cells form cerumen (earwax) 16-34 Anatomy of Middle Ear 16-35 Middle Ear • Air-filled tympanic cavity in temporal bone between tympanic membrane and oval window – continuous with mastoid air cells • Contains – auditory tube (eustachian tube) connects to nasopharynx • equalizes air pressure on tympanic membrane – ear ossicles • malleus • incus • stapes – stapedius and tensor tympani muscles attach to stapes and malleus 16-36 Anatomy of Inner Ear 16-37 Inner Ear • Bony labyrinth - passageways in temporal bone • Membranous labyrinth - fleshy tubes lining bony tunnels – filled with endolymph (similar to intracellular fluid) – floating in perilymph (similar to cerebrospinal fluid) 16-38 Details of Inner Ear Fig. 16.12c 16-39 Details of Inner Ear 16-40 Anatomy of Cochlea • Scala media (cochlear duct) – separated from • scala vestibuli by vestibular membrane • scala tympani by basilar membrane • Spiral organ (organ of corti) 16-41 Spiral Organ 16-42 Spiral Organ • Stereocilia of hair cells attach to gelatinous tectorial membrane • Inner hair cells – hearing • Outer hair cells – adjust cochlear responses to different frequencies – increase precision 16-43 SEM of Cochlear Hair Cells 16-44 Physiology of Hearing - Middle Ear • Tympanic membrane – has 18 times area of oval window – ossicles transmit enough force/unit area at oval window to vibrate endolymph in scala vestibuli • Tympanic reflex – muscle contraction – tensor tympani m. tenses tympanic membrane – stapedius m. reduces mobility of stapes • best response to slowly building loud sounds • occurs while speaking 16-45 Stimulation of Cochlear Hair Cells • Vibration of ossicles causes vibration of basilar membrane under hair cells – as often as 20,000 times/second 16-46 Cochlear Hair Cells • Stereocilia of OHCs – bathed in high K+ • creating electrochemical gradient – tips embedded in tectorial membrane – bend in response to movement of basilar membrane • pulls on tip links and opens ion channels • K+ flows in – depolarization causes release of neurotransmitter • stimulates sensory dendrites at base 16-47 Potassium Gates 16-48 Sensory Coding • Vigorous vibrations excite more inner hair cells over a larger area – triggers higher frequency of action potentials – brain interprets this as louder sound • Pitch depends on which part of basilar membrane vibrates – at basal end, membrane narrow and stiff • brain interprets signals as high-pitched – at distal end, 5 times wider and more flexible • brain interprets signals as low-pitched 16-49 Basilar Membrane Frequency Response Notice high and low frequency ends 16-50 Cochlear Tuning • Increases ability of cochlea to receive some sound frequencies • Outer hair cells contract reducing basilar membranes freedom to vibrate – fewer signals from that area allows brain to distinguish between more and less active areas of cochlea • Pons has inhibitory fibers that synapse near the base of IHCs – increases contrast between regions of cochlea 16-51 Innervation of Internal Ear • Vestibular ganglia - visible in vestibular nerve • Spiral ganglia - buried in modiolus of cochlea 16-52 Auditory Pathway 16-53 Auditory Projection Pathway • Spiral ganglion formed by cell bodies of sensory neurons • Axons form cochlear nerve portion of CN VIII • Synapse in cochlear nuclei • Binaural hearing – superior olivary nucleus compares sounds from both sides to identify direction • Inferior colliculus helps – locate origin of sound – process fluctuations in pitch during speech – produce startle response; head turning to loud sound • Fibers from inferior colliculus go to primary auditory cortex – temporal lobe 16-54 Auditory Processing Centers • Damage to either auditory cortex does not cause unilateral deafness (extensive decussation) 16-55 Equilibrium • Control of coordination and balance • Receptors in vestibular apparatus – semicircular ducts contain crista – saccule and utricle contain macula • Static equilibrium – perceived by macula – perception of head orientation • Dynamic equilibrium – perception of motion or acceleration • linear acceleration perceived by macula • angular acceleration perceived by crista 16-56 Saccule and Utricle • Contain macula – hair cells with stereocilia and one kinocilium buried in a gelatinous otolithic membrane – otoliths add to the density and inertia and enhance the sense of gravity and motion 16-57 Macula • • Static equilibrium - when head is tilted, weight of membrane bends the stereocilia Dynamic equilibrium – in car, linear acceleration detected as otoliths lag behind 16-58 Crista ampullaris • Consists of hair cells buried in a mound of gelatinous membrane (one in each duct) • Orientation causes ducts to be stimulated by rotation in 16-59 different planes Crista Ampullaris - Head Rotation • As head turns, endolymph lags behind, pushes cupula, 16-60 stimulates hair cells Vestibular Projection Pathways 16-61 Equilibrium Projection Pathways • Hair cells of macula sacculi, macula utriculi and semicircular ducts synapse on vestibular nerve • Fibers end in vestibular nucleus in pons and medulla 16-62 Equilibrium Projection Pathways • Information sent to 5 targets – cerebellar control of head and eye movements and posture – nuclei of CN III, IV, and VI to produce vestibulo ocular reflex – reticular formation control of blood circulation and posture – vestibulospinal tracts innervate antigravity muscles – thalamic relay to cerebral cortex for awareness of position and movement 16-63 Vision and Light • Vision - perception of light emitted or reflected from objects in the environment • Visible light – electromagnetic radiation with wavelengths from 400 to 750 nm – must cause a photochemical reaction to produce a nerve signal • radiation below 400 nm; energetic, kills cells • radiation above 750 nm; too little energy to cause photochemical reaction 16-64 External Anatomy of Eye 16-65 Eyebrows and Eyelids • Eyebrows provide facial expression • Eyelids (palpebrae) – block foreign objects, help with sleep, blink to moisten – meet at corners (commissures) – consist of orbicularis oculi muscle and tarsal plate covered with skin outside and conjunctiva inside – tarsal glands secrete oil that reduces tear evaporation – eyelashes help keep debris from eye 16-66 Conjunctiva • Transparent mucous membrane lines eyelids and covers anterior surface of eyeball except cornea • Richly innervated and vascular (heals quickly) 16-67 Lacrimal Apparatus • Tears flow across eyeball help to wash away foreign particles, help with diffusion of O2 and CO2 and contain bactericidal enzyme 16-68 Extrinsic Eyes Muscles • 6 muscles inserting on eyeball – 4 rectus, superior and inferior oblique muscles • Innervated by cranial nerves III, IV and VI 16-69 Innervation of Extrinsic Eye Muscles 16-70 Tunics of the Eyeball • Fibrous layer - sclera and cornea • Vascular layer - choroid, ciliary body and iris • Internal layer - retina and optic nerve 16-71 Optical Components • Structures refract light to focus on retina – cornea • transparent cover on anterior surface of eyeball – aqueous humor • serous fluid posterior to cornea, anterior to lens – lens • changes shape to help focus light – rounded with no tension – flattened due to pull of suspensory ligaments – vitreous humor • jelly fills space between lens and retina 16-72 Aqueous Humor • Produced by ciliary body, flows to posterior chamber through pupil to anterior chamber reabsorbed into canal of Schlemm 16-73 Cataracts and Glaucoma • Cataract - clouding of lens – aging, diabetes, smoking, and UV light • Glaucoma – death of retinal cells due to elevated pressure within the eye • obstruction of scleral venous sinus • colored halos and dimness of vision 16-74 Neural Components • Includes retina and optic nerve • Retina – forms as an outgrowth of the diencephalon – attached at optic disc and at ora serrata – pressed against rear of eyeball by vitreous 16-75 Detached retina • Blow to head or lack of vitreous • Blurry areas in field of vision • Disrupts blood supply, leads to blindness 16-76 Ophthalmoscopic Exam of Eye • Macula lutea - cells on visual axis of eye (3 mm) – fovea centralis - center of macula; finely detailed images due to packed receptor cells • Direct evaluation of blood vessels 16-77 Test for Blind Spot • Optic disk = blind spot – optic nerve exits posterior surface of eyeball – no receptor cells • Blind spot - use test illustration above – close eye, stare at X and red dot disappears • Visual filling - brain fills in green bar across blind spot area 16-78 Formation of an Image • Light passes through lens to form inverted image on retina • Pupillary constrictor - smooth muscle encircling the pupil – parasympathetic stimulation narrows pupil • Pupillary dilator - spokelike myoepithelial cells – sympathetic stimulation widens pupil • Active when light intensity changes or gaze shifts from distant object to nearby object – photopupillary reflex -- both pupils constrict if one eye is illuminated (type of consensual reflex) 16-79 Principle of Refraction Light striking the lens or cornea at a 90 degree angle is not bent. 16-80 Refraction • Bending of light rays occurs when light passes through substance with different refractive index at any angle other than 90 degrees – refractive index of air is arbitrarily set to n = 1 – refractive index • cornea is n = 1.38 • lens is n = 1.40 • Cornea refracts light more than lens does – due to shape of cornea – lens becomes rounder to increase refraction for near vision 16-81 Near Response • Allows eyes to focus on nearby object (that sends oblique light waves to eyes) 1. convergence of eyes • eyes orient their visual axis towards object 2. constriction of pupil • blocks peripheral light rays and reduces spherical aberration (blurry edges) 3. accomodation of lens • ciliary muscle contracts, lens takes convex shape – light refracted more strongly and focused onto retina 16-82 Emmetropia and Near Response Fig. 16.31a Distant object Close object 16-83 Emmetropia and Near Response 16-84 Accommodation of Lens 16-85 Effects of Corrected Lenses • Hyperopia - farsighted (eyeball too short) – correct with convex lenses • Myopia - nearsighted (eyeball too long) – correct with concave lenses 16-86 Photoreceptor Cells • Posterior layer of retina pigment epithelium – purpose is to absorb stray light and prevent reflections • Photoreceptors – rod cells (night - scotopic vision) • outer segment - stack of coinlike membranous discs studded with rhodopsin pigment molecules – cone cells (color - photopic vision) • outer segment tapers to a point 16-87 Histology - Layers of Retina 16-88 Location of Visual Pigments 16-89 Nonreceptor Retinal Cells • Bipolar cells (1st order neurons) – synapse on ganglion cells – large amount of convergence • Ganglion cells (2nd order neurons) – axons of these form optic nerve – more convergence occurs (114 receptors to one optic nerve fiber) • Horizontal and amacrine cells form connections between other cells – enhance perception of contrast, edges of objects and changes in light intensity 16-90 Schematic Layers of the Retina 16-91 Visual Pigments • Rod cells have rhodopsin – has absorption peak at wavelength of 500 nm – 2 major parts of molecule • opsin - protein portion • retinal - a vitamin A derivative • Cones contain photopsin (iodopsin) – opsin moieties contain different amino acids that determine wavelengths of light absorbed – 3 kinds of cones absorbing different wavelengths of light produce color vision 16-92 Rhodopsin Bleaching/Regeneration • Rhodopsin absorbs light, converted from bent shape (cis-retinal) to straight (trans-retinal) – retinal dissociates from opsin (bleaching) – 5 minutes to regenerate 50% of bleached rhodopsin 16-93 Generating Visual Signals 16-94 Generating Nerve Signals - Rods • In the dark, rods exhibit a dark signal – flow of Na+ and release of neurotransmitter (glutamate) • depolarization by Na+ stimulates glutamate release • In the light, dark current and glutamate release stops – bleached rhodopsin molecule acts like an enzyme and breaks down cGMP molecules – Na+ gates close and dark current ceases (inhibition stops), nerve signal results 16-95 Bipolar Cell Function • Two kinds of bipolar cells – inhibited (hyperpolarized) by glutamate • excited by rising light intensity – excited (depolarized) by glutamate • excited by falling light intensity • As your eye scans a scene, areas of light and dark cause a changing pattern of bipolar cell responses • Variable pattern of stimulation of ganglion cells and nerve signals sent to the brain 16-96 Light and Dark Adaptation • Light adaptation (walk out into sunlight) – pupil constriction and pain from over stimulated retinas – color vision and acuity below normal for 5 to 10 minutes • Dark adaptation (turn lights off) – dilation of pupils occurs – 20 to 30 minutes required for regeneration of rhodopsin 16-97 Duplicity Theory • Explains why we have both rods and cones • Single type of receptor cell incapable of providing high sensitivity and high resolution – sensitive night vision = one type of cell and neural circuitry – high resolution daytime vision = different cell type and neuronal circuitry 16-98 Duplicity Theory 16-99 Scotopic System (Night Vision) • Rods sensitive – react even in dim light – extensive neuronal convergence – 600 rods converge on 1 bipolar cell – many bipolar converge on each ganglion cell – results in high degree of spatial summation • one ganglion cells receives information from 1 mm2 of retina producing only a coarse image • Edges of retina have widely-spaced rod cells, act as motion detectors 16-100 Photopic System (Day Vision) • Fovea contains only 4000 tiny cone cells (no rods) – no neuronal convergence – each foveal cone cell has “private line to brain” • High-resolution color vision – little spatial summation so less sensitivity to dim light 16-101 Color Vision • Primates have well developed color vision – nocturnal vertebrates have only rods • Cones named for absorption peaks of photopsins – blue cones peak sensitivity at 420 nm – green cones peak at 531 nm – red cones peak at 558 nm (orange-yellow) • Color perception based on mixture of nerve signals 16-102 Color Blindness • Hereditary lack of one photopsin – red-green is common (lack either red or green cones) • incapable of distinguishing red from green • sex-linked recessive (8% of males) 16-103 Stereoscopic Vision (Stereopsis) • Depth perception - ability to judge distance to objects – requires 2 eyes with overlapping visual fields – panoramic vision has eyes on sides of head (horse) • Fixation point – farther away requires image focus medial to fovea – closer results in image focus lateral to fovea 16-104 Visual Projection Pathway 16-105 Visual Projection Pathway • Bipolar and ganglion cells in retina - 1st and 2nd order neurons (ganglion cell axons of form CN II) • Hemidecussation in optic chiasm – 1/2 of fibers decussate so that images of all objects in left visual field fall on right half of each retina – each side of brain sees what is on side where it has motor control over limbs • 3rd order neurons in lateral geniculate nucleus of thalamus form optic radiation to 1 visual cortex where conscious visual sensation occurs • Few fibers project to superior colliculi and midbrain for visual reflexes (photopupillary and accomodation) 16-106 Visual Information Processing • Some processing occurs in retina – adjustments for contrast, brightness, motion and stereopsis • Visual association areas in parietal and temporal lobes process visual data – object location, motion, color, shape, boundaries – store visual memories (recognize printed words) 16-107