Spine_01 (Anatomy)
advertisement

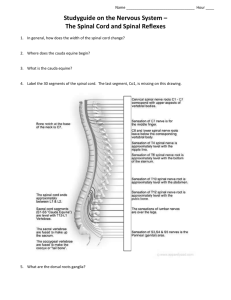
Spinal (Anatomy) INTRODUCTION 1. Because it is primary pathway of communication between brain and PNS, diseases that affect spinal cord are clinically eloquent. Many of these disease processes have predilection for targeting specific areas or tracts within spinal cord. As result, knowledge of spinal cord anatomy and recognition of typical common spinal cord syndromes are useful in evaluation of patient with myelopathy and can allow for more directed diagnostic evaluation. 2. The anatomy of spinal cord and its vascular supply and clinical features of common spinal cord syndromes will be reviewed here. Diseases that affect spinal cord are discussed separately. ANATOMY 1. There are 31 spinal cord segments, each with pair of ventral (anterior) and dorsal (posterior) spinal nerve roots, which mediate motor and sensory function. The ventral and dorsal nerve roots combine on each side to form spinal nerves as they exit from vertebral column through neuroforamina. 2. Longitudinal organization A. The spinal cord is divided longitudinally into 4 regions: cervical, thoracic, lumbar, and sacral cord. The spinal cord extends from base of skull and terminates near lower margin B. of L1. Below that level, spinal canal contains lumbar, sacral, and coccygeal spinal nerve roots that comprise cauda equina. Because spinal cord is shorter than vertebral column, vertebral and spinal cord segmental levels are not necessarily the same. C1 through C8 spinal cord segments lie between C1 through C7 vertebral levels. T1 through T12 cord segments lie between T1 through T8. The five lumbar cord segments are situated at T9 through T11 vertebral levels, and S1 through S5 segments lie between T12 to L1. C1 through C7 nerve roots emerge above their respective vertebrae; C8 nerve root emerges between C7 and T1 vertebral bodies. The remaining nerve roots emerge below their respective vertebrae. C. Cervical cord i. The first cervical vertebra (atlas) and second cervical vertebra (axis), upon which atlas pivots, support head at atlanto-occiput junction. The interface between first and second vertebra is called atlanto-axis junction. ii. Cervical spinal segments innervate skin and musculature of upper extremity and diaphragm. 1. C3 through C5 innervate diaphragm, chief muscle of inspiration, via phrenic nerve 2. C4 through C7 innervate shoulder and arm musculature 3. C6 through C8 innervate forearm extensors and flexors 4. C8 through T1 innervate hand musculature D. Thoracic cord i. The thoracic vertebral segments are defined by those that have attached rib. The spinal roots form intercostal nerves that run along inferior rib margin and innervate associated dermatomes, as well as intercostal abdominal wall musculature. These muscles are main muscles of expiration. The thoracic cord also contains sympathetic nerves that heart and abdominal organs. E. Lumbosacral cord i. Lumbosacral spinal cord contains segment that innervate muscles and dermatomes of lower extremity, as well as buttocks and anal regions. Sacral nerve roots S3 ii. through S5 originate in narrow terminal part of cord, called conus medullaris. 1. L2 and L3 mediate hip flexion 2. L3 and L4 mediate knee extension 3. L4 and L5 mediate ankle dorsiflexion and hip extension 4. L5 and S1 mediate knee flexion 5. S1 and S2 mediate ankle plantar flexion Sacral nerve roots also provide parasympathetic innervation of pelvic and abdominal organs, while lumbar nerve roots L1 and L2 contain sympathetic innervation of some pelvic and abdominal organs. F. 3. Cauda equina i. In adults, spinal cord ends at level of L1 and L2. The filum terminale, thin connective tissue filament that descends from conus medullaris with spinal nerve roots, is connected to third, fourth, and fifth sacral vertebrae; its terminal part is fused to periosteum at base of coccygeal bone. ii. Pathology at T12 and L1 vertebral level affects lumbar cord. Injuries to L2 frequently damage conus medullaris. Injuries below L2 usually involve cauda equina and represent injuries to spinal roots rather than to spinal cord. Cross-sectional anatomy A. The spinal cord contains gray matter, butterfly-shaped central region, and surrounding white matter tracts. The spinal cord gray matter, which contains neuronal cell bodies, is made up of dorsal and ventral horns, each divided into several laminae. B. Dorsal horn i. The dorsal horn is entry point of sensory information into CNS. It is divided into 6 layers or laminae that process sensory information. More than relay station for transmission of sensory information, dorsal horn also modulates pain transmission through spinal and supraspinal regulatory circuits. Three major categories of sensory input that are important to clinical examination of spinal cord pathology. 1. 2. Afferents from muscle spindles that participate in spinal cord reflexes. Axons, mostly small and unmyelinated, mediating sensory modalities of pain and temperature. These can travel up and down few segments before synapsing with 2nd order neurons, which then cross midline of cord in anterior commissure, just anterior to central canal, and then enter contralateral anterior or lateral spinothalamic tract. 3. Axons mediating sensory modalities of proprioception, vibration, and touch discrimination. These large myelinated fibers pass through dorsal horn to enter ipsilateral dorsal column. ii. The anatomy of sensory system is discussed in more detail separately. C. Ventral horn i. The motor nuclei of spinal cord are contained within ventral horn, which also contains interneurons mediating information from other descending tracts of pyramidal and extrapyramidal motor systems. These ultimately synapse on α and γ motor neurons, which subsequently leave ventral horn via ventral nerve root to terminate at NMJ. D. White matter tract i. The major WM tracts of clinical importance in assessment of spinal cord disease. 1. The dorsal or posterior columns, fasciculus gracilis, and fasciculus cuneatus. These contain sensory information regarding joint position and vibration. They are organized anatomically such that cervical sections lie most laterally and sacral segments most medially. These pathways will cross in medulla; hence, in spinal cord, these tracts contain ipsilateral sensory representation. 2. 3. ii. iii. commissure and therefore contain contralateral sensory representation. This tract is somatotopically organized with cervical inputs located most medially and sacral inputs most laterally. The corticospinal tracts contain UMN that originate in M1 of primary motor cortex. These axons synapse either directly or indirectly on anterior horn cells, and as such have distinct sites of anatomic origin within M1. A single corticomotoneuronal axon synapses with many anterior horn cells of its own motor neuron pool and also with those of agonists and antagonists, allowing for coordination of highly skilled movements. The lateral corticospinal tract contains majority (80 to 85%) of these fibers, which have previously decussated (crossed) at cervicomedullary junction and therefore provide input to ipsilateral musculature. Fibers are somatotopically organized within tract such that fibers destined for upper extremity motor control lie most medially, while fibers controlling lower extremity lie more laterally. The anterior corticospinal tract contains undecussated fibers, some of which will subsequently cross at spinal level through anterior commissure. Other descending tracts. 1. The tectospinal tract originates in superior colliculus and mediates reflex postural movements of head in response to visual and/or acoustic input. 2. 3. 4. iv. The anterior and lateral spinothalamic tracts contain sensory information regarding pain, temperature, and touch. These axons have crossed in ventral The rubrospinal tract originates from magnocellular subdivision of red nucleus, markedly developed in reptiles, birds, and other lower mammals, but is much less evident in primates, in which there are direct connections with motoneurons innervating wrist muscles. The vestibulospinal tract arises from vestibular nuclei and facilitates spinal cord reflexes and muscle tone to maintain posture. Reticulospinal tract are widely assumed to be responsible for coordinated gross movements primarily of proximal muscles, whereas corticospinal tract mediates fine movements, particularly of hand. However, reticulospinal system may form parallel pathway to distal muscles, alongside corticospinal tract. As result, reticulospinal neurons may influence upper limb muscle activity after damage to corticospinal system as may occur in stroke. Other ascending tracts. 1. The dorsal and ventral spinocerebellar tracts carry inputs mediating unconscious proprioception directly to cerebellum 2. The spinoreticular tract carries deep pain input to reticular formation of brainstem 4. Autonomic fiber A. Autonomic fibers of hypothalamic and brainstem origin descend in lateral aspect of B. C. D. E. F. 5. spinal cord but not in well-defined tract. These synapse with cell bodies in intermediolateral columns of central gray matter of spinal cord. Sympathetic fibers exit between T1 and L2, and parasympathetic fibers exit between S2 and S4. The sympathetic neurons lie in lateral horn of central gray matter at spinal levels T1-L3. The preganglionic fibers exit via ventral root, spinal nerve, and ventral ramus to reach paravertebral ganglion. Many will synapse at paravertebral ganglion, others pass through it to terminate on postganglionic neurons more proximate to their end organ. Parasympathetic neurons originate in sacral spinal cord and exit spinal cord with other efferents to ventral ramus. After leaving ventral ramus, they may subsequently join with sympathetic nerves to reach viscera. These preganglionic fibers then synapse with diffuse network of terminal ganglion cells that affect organs in pelvis. Autonomic dysfunction is important determinant of site, extent, and severity of spinal cord pathology. Many autonomic functions can be affected by spinal cord pathology, but for clinical evaluation, the most useful symptoms relate to bladder control. Autonomic bladder control is primarily parasympathetic, and is unaffected by isolated injury to the sympathetic fibers. Voluntary bladder control is under somatomotor control, mediated by motor fibers originating from anterior horn cells at levels S2-S4. A spinal cord lesion that interrupts descending motor and autonomic tracts above S2 level produces "automatic bladder" that cannot be emptied voluntarily, but empties reflexly when expanded to certain degree, so-called neurogenic bladder. Loss of descending inhibition of segmental reflex control leads to urinary urgency and incontinence. Injury to S2-S4 spinal levels interrupts bladder reflex circuit; bladder becomes flaccid, and fills beyond capacity with overflow incontinence. Other autonomic functions are disturbed by spinal cord pathology. The effects of spinal cord injury on colon and rectum are similar to those on bladder. Spinal cord transections interrupt voluntary control of external sphincter and produce constipation. Sacral lesions cause loss of anal reflex and rectal incontinence. Impotence can result from spinal cord lesions at any level. Spinal cord injuries can also affect CV function, most dramatically with lesions above T6 which can produce phenomenon of autonomic dysreflexia. Blood supply A. A single anterior and two posterior spinal arteries supply spinal cord. The anterior spinal artery supplies anterior two-thirds of cord. The posterior spinal arteries primarily supply dorsal columns. The anterior and posterior spinal arteries arise from VA in neck and descend from base of skull. Various radicular arteries branch off thoracic and abdominal aorta to provide additional blood supply to spinal arteries. The largest and most consistently present of these radicular branches is the great ventral radicular artery or artery of Adamkiewicz, which supplies anterior spinal artery. This artery enters the spinal cord anywhere between T5 and L1 (usually between T9 and T12). B. C. In most people, anterior spinal artery passes uninterrupted along entire length of spinal cord; in others, it is discontinuous, usually in its midthoracic segment, making these individuals more susceptible to vascular injury. The primary watershed area of spinal cord in most people is in midthoracic region. The vascular anatomy of spinal cord is discussed in detail separately. LOCALIZATION 1. A spinal cord lesion may be suspected when there are bilateral motor and sensory signs or symptoms that do not involve head or face. Motor deficits are manifest by weakness and long tract signs (spasticity, increased reflexes, Babinski sign). When pathology is localized or segmental, these findings will be present in muscle groups innervated below that level and will be normal above. A sensory level, with normal sensation above and reduced or absent below, can also often be defined and should be specifically sought. Other so-called segmental signs include lower motor neuron findings (atrophy, flaccid weakness, loss of reflexes) in myotomal distribution at specific level of involvement; however, these are usually not elicitable in thoracic lesions. 2. 3. As well as longitudinal localization within spinal cord, it can also be helpful to distinguish specific areas of functional loss with spinal cord level (or across spinal cord levels for non-segmental pathologies). Some disorders affecting spinal cord preferentially affect different structures, and therefore careful testing of all spinal cord functions, including motor, reflex, and all sensory modalities, and sphincter function is important for clinical localization. Several distinct spinal cord syndromes are recognized. These are useful in clinical evaluation, as they often correspond to distinct pathologies. These are summarized in table and are discussed below (table 1). 4. Segmental syndrome A. Pathologies that affect all functions of spinal cord at one or more levels produce B. segmental syndrome. Loss of function may be total or incomplete. A total cord transection syndrome results from cessation of function in all ascending and descending spinal cord pathways and results in loss of all types of sensation and loss of movement below level of lesion. Less profound injuries produce similar pattern of deficits, which are less severe: ie, weakness rather than paralysis and decreased sensation rather than anesthesia. Acute transection can cause spinal shock, with flaccid paralysis, urinary retention, and diminished tendon reflexes. This is usually temporary, and increased tone, spasticity, and hyperreflexia will usually supervene in days or weeks after the event. C. 5. Transverse injuries above C3 involve cessation of respiration and are often fatal if acute. Cervical cord lesions that spare phrenic nerve but impair intercostal nerve function can produce respiratory insufficiency. Lesions above L2 cord level will cause impotence and spastic paralysis of bladder. There is loss of voluntary control of bladder, which will empty automatically by reflex action. D. Causes of cord segmental syndrome include acute myelopathies, such as traumatic injury and spinal cord hemorrhage. Epidural or intramedullary abscess, tumors, and transverse myelitis may have more subacute presentation. Dorsal (posterior) cord syndrome A. Dorsal cord syndrome results from bilateral involvement of dorsal columns, B. corticospinal tracts, and descending central autonomic tracts to bladder control centers in sacral cord. Dorsal column symptoms include gait ataxia and paresthesias. Corticospinal tract dysfunction produces weakness that, if acute, is accompanied by muscle flaccidity and hyporeflexia and, if chronic, by muscle hypertonia and hyperreflexia. Extensor plantar responses and urinary incontinence may be present. Causes of dorsal cord syndrome include multiple sclerosis (more typically primary progressive form), tabes dorsalis, Friedreich ataxia, subacute combined degeneration, vascular malformations, epidural and intradural extramedullary tumors, cervical spondylotic myelopathy, and atlantoaxial subluxation. 6. Ventral (anterior) cord syndrome A. Ventral cord or anterior spinal artery syndrome usually includes tracts in anterior 66% of spinal cord, which include corticospinal tracts, spinothalamic tracts, and descending autonomic tracts to sacral centers for bladder control. Corticospinal tract involvements produce weakness and reflex changes. A spinothalamic tract deficit produces bilateral loss of pain and temperature sensation. Tactile, position, and vibratory sensation are normal. Urinary incontinence is usually present. B. The causes of ventral cord syndrome include infarction, HIVD, and radiation myelopathy. 7. Brown-Sequard (hemi-cord) syndrome A. A lateral hemisection syndrome, also known as Brown–Sequard syndrome, involves dorsal column, corticospinal tract, and spinothalamic tract unilaterally. This produces weakness, loss of vibration, and proprioception ipsilateral to lesion and loss of pain and temperature on opposite side. The unilateral involvement of descending autonomic fibers does not produce bladder symptoms. While there are many causes of this syndrome, knife or bullet injuries and demyelination are the most common. Rarer causes include spinal cord tumors, disc herniation, infarction, and infection. 8. Central cord syndrome A. The central cord syndrome is characterized by loss of pain and temperature sensation in distribution of one or several adjacent dermatomes at site of spinal cord lesion caused by disruption of crossing spinothalamic fibers in ventral commissure. Dermatomes above and below level of lesion have normal pain and temperature sensation, creating the so-called "suspended sensory level." Vibration and proprioception are often spared. B. As central lesion enlarges, it may encroach on medial aspect or corticospinal tracts or on anterior horn gray matter, producing weakness in analgesic areas. Fibers mediating DTR are interrupted as they pass from dorsal to ventral horn, thus causing tendon reflex loss C. in analgesic areas. There are usually no bladder symptoms. The classic causes of central cord syndrome are slow-growing lesions such as syringomyelia or intramedullary tumor. However, central cord syndrome is most frequently result of hyperextension injury in individuals with long-standing cervical spondylosis. This form of central cord syndrome is characterized by disproportionately greater motor impairment in upper compared with lower extremities, bladder dysfunction, and variable degree of sensory loss below level of injury. 9. Pure motor syndrome A. A pure motor syndrome produces weakness without sensory loss or bladder involvement. This may involve only upper motor neurons, producing hyperreflexia and extensor plantar responses, or only lower motor neuron bilaterally, producing muscle atrophy and fasciculations. Other disorders involve both upper and lower motor neurons and produce mixed signs. B. The causes of pure motor syndrome include chronic myelopathies such as HTLV-I myelopathy, hereditary spastic paraplegia, primary lateral sclerosis, amyotrophic lateral sclerosis, progressive muscular atrophy, post-polio syndrome, and electric shock-induced myelopathy. 10. Conus medullaris syndrome A. Lesions at vertebral level L2 often affect conus medullaris. There is early and prominent sphincter dysfunction with flaccid paralysis of bladder and rectum, impotence, and saddle (S3-S5) anesthesia. Leg weakness may be mild if lesion is very restricted and spares both lumbar cord and adjacent sacral and lumbar nerve roots. B. Causes include HIVD, spinal fracture, and tumors. 11. Cauda equina syndrome A. Though not spinal cord syndrome, cauda equina syndrome is considered here because its location within spinal canal subjects it to many of same disease processes that cause myelopathy. The syndrome is caused by loss of functions of two or more of 18 nerve roots constituting cauda equina. Deficits usually affect both legs but are often asymmetric. i. Low back pain accompanied by pain radiating into one or both legs. Radicular pain reflects involvement of dorsal nerve roots and may have localizing value. ii. Weakness of plantar flexion with loss of ankle jerks occurs with mid cauda equina lesions, involving S1, S2 roots. Involvement of progressively higher levels leads to corresponding weakness in other muscles. iii. Bladder and rectal sphincter paralysis usually reflect involvement of S3-S5 nerve roots. iv. Sensory loss of all sensory modalities occurs in dermatomal distribution of affected nerve roots. B. Many etiologies can cause cauda equina syndrome, including HIVD, epidural abscess, epidural tumor, intradural extramedullary tumor, lumbar spine spondylosis, and number of inflammatory conditions including spinal arachnoiditis, CIDP, and sarcoidosis. The cauda equina can also be primary site of involvement in carcinomatous meningitis and number of infections (CMV, HSV, VZV, EBV, Lyme disease, mycoplasma, and TB). 12. Lhermitte's sign A. This well-described sign describes sensation of electric shock-like sensations that run down back and/or limbs during flexion of neck. This generally occurs with pathologies involving cervical spinal cord, but is not specific to etiology, occurring in patients with cervical spondylotic myelopathy, multiple sclerosis, radiation myelopathy, and vitamin B12 deficiency, among others. It can also occur with cervical nerve root pathology. DIAGNOSIS 1. The differential diagnosis of myelopathy is wide, but can be significantly narrowed by clinical syndrome. Other features in examination and history also limit differential diagnosis and 2. 3. tailor diagnostic work-up. Clinical features of some of more common causes of myelopathy are outlined in the Table (table 2). These are discussed in detail separately. For patients with clinical syndrome that suggests localized process within spinal cord (transection syndrome, central cord syndrome, ventral cord syndrome), imaging study, usually MRI, of relevant section of spinal cord is usually required. Administration of gadolinium contrast is often helpful. When infectious or inflammatory disorder is suspected, CSF examination may be helpful. The role of PET in evaluating patients with myelopathy is under investigation; it appears to be particularly sensitive for neoplastic disease. In general, pace at which spinal cord deficits appear dictate urgency of neurologic evaluation. Even when deficits are not severe, acute myelopathic signs need to be evaluated urgently because neurologic deterioration can occur abruptly, and clinical deficit at time of intervention often dictates chances of recovery. This is true particularly for compressive etiologies such as spinal cord metastases and epidural spinal abscess. SUMMARY 1. Disorders that affect the spinal cord often target specific structural and functional anatomic regions, producing distinct clinical syndromes. The spinal cord syndromes are summarized in the table. The clinical syndrome along with other features in examination and history usually significantly limits the differential diagnosis and tailors the diagnostic work-up.