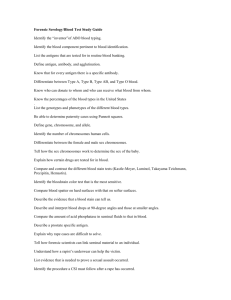
IMMUNOLOGY AND IMMUNOTECH - E
advertisement

SEMESTER III PAPER IX - IMMUNOLOGY & MMUNOTECHNOLOGY UNIT - II Antigens - properties, Epitopes, haptens, adjuvant, cross reactivity. Antibodies - properties, structure (primary & secondary) and isotypes. Diversity and specificity. Anti antibodies. UNIT - III Serology - Introduction and classification of antigens and antibody reactions - Agglutination and precipitation reaction. Strength of antigen and antibody bindings - affinity & avidity. Complement pathway and complement fixation reaction. Immunofluorscence RIA, RAST, ELISA and Flowcytometry. Monoclonal antibodies & its applications. (Hybridoma technique) UNIT - IV MHC antigens - types and functions. Regulation and response of immune system. Response of B Cell to antigens. T cell products. Immunity to infectious diseases - Viral, bacterial and protozoan . Hyper sensitivity reactions . UNIT V Transplantation immunology - Tissue transplantation and grafting . Mechanism of graft acceptance and rejection. HLA typing Tumor immunology. Immunodeficiency diseases and auto immunity. Vaccines - Types and vaccination methods. UNIT I Historical background and scope of immunology, Immunohaematology -ABO and Rh factor. Cells and organs of immune system. Non immunological defence mechanism - Barriers, Phagocytosis, inflammation, fever . Types of immunity - HI and CMI. 1. Explain the historical background and scope of immunology. 1718 - Lady Mary Wortley Montagu, the wife of the British ambassador to Constantinople, observed the positive effects of variolation on the native population and had the technique performed on her own children. 1798 - First demonstration of vaccination smallpox vaccination (Edward Jenner) 1837 - First description of the role of microbes in putrefaction and fermentation (Theodore Schwann) 1838 - Confirmation of the role of yeast in fermentation of sugar to alcohol (Charles Cagniard-Latour) 1840 - First "modern" proposal of the germ theory of disease (Jakob Henle) 1850 - Demonstration of the contagious nature of puerperal fever (childbed fever) (Ignaz Semmelweis) 1857-1870 - Confirmation of the role of microbes in fermentation (Louis Pasteur) 1862 - phagocytosis (Ernst Haeckel) 1867 - First aseptic practice in surgery using carbolic acid (Joseph Lister) 1876 - First demonstration that microbes can cause disease-anthrax (Robert Koch) 1877 - Mast cells (Paul Ehrlich) 1878 - Confirmation and popularization of the germ theory of disease (Louis Pasteur) 1880 - 1881 -Theory that bacterial virulence could be attenuated by culture in vitro and used as vaccines. Proposed that live attenuated microbes produced immunity by depleting host of vital trace nutrients. Used to make chicken cholera and anthrax "vaccines" (Louis Pasteur) 1883 - 1905 - Cellular theory of immunity via phagocytosis by macrophages and microphages (polymorhonuclear leukocytes) (Elie Metchnikoff) 1885 - Introduction of concept of a "therapeutic vaccination". First report of a live "attenuated" vaccine for rabies (Louis Pasteur). 1888 - Identification of bacterial toxins (diphtheria bacillus) (Pierre Roux and Alexandre Yersin) 1888 - Bactericidal action of blood (George Nuttall) 1890 - Demonstration of antibody activity against diphtheria and tetanus toxins. Beginning of humoral theory of immunity. (Emil von Behring) and (Shibasaburo Kitasato) 1891 - Demonstration of cutaneous (delayed type) hypersensitivity (Robert Koch) 1893 - Use of live bacteria and bacterial lysates to treat tumors-"Coley's Toxins" (William B. Coley) 1894 - Bacteriolysis (Richard Pfeiffer) 1896 - An antibacterial, heat-labile serum component (complement) is described (Jules Bordet) 1900 - Antibody formation theory (Paul Ehrlich) 1901 - blood groups (Karl Landsteiner) 1902 - Immediate hypersensitivity anaphylaxis (Paul Portier) and (Charles Richet) 1903 - Intermediate hypersensitivity, the "Arthus reaction" (Maurice Arthus) 1903 - Opsonization 1905 - "Serum sickness" allergy (Clemens von Pirquet and (Bela Schick) 1909 - Paul Ehrlich proposes "immune surveillance" hypothesis of tumor recognition and eradication 1911 - 2nd demonstration of filterable agent that caused tumors (Peyton Rous) 1917 - hapten (Karl Landsteiner) 1921 - Cutaneous allergic reactions (Otto Prausnitz and Heinz Küstner) 1924 - Reticuloendothelial system 1938 - Antigen-Antibody binding hypothesis (John Marrack) 1940 - Identification of the Rh antigens (Karl Landsteiner and Alexander Weiner) 1942 - Anaphylaxis (Karl Landsteiner and Merill Chase) 1942 - Adjuvants (Jules Freund and Katherine McDermott) 1944 - hypothesis of allograft rejection 1945 - Coombs Test aka antiglobulin test (AGT) 1946 - identification of mouse MHC (H2) by George Snell and Peter A. Gorer 1948 - antibody production in plasma B cells 1949 - growth of polio virus in tissue culture, neutralization with immune sera, and demonstration of attenuation of neurovirulence with repetitive passage (John Enders) and (Thomas Weller) and (Frederick Robbins) 1949 - immunological tolerance hypothesis 1951 - vaccine against yellow fever 1953 - Graft-versus-host disease 1953 - immunological tolerance hypothesis 1957 - Clonal selection theory (Frank Macfarlane Burnet) 1957 - Discovery of interferon by Alick Isaacs and Jean Lindenmann 1958-1962 - Discovery of human leukocyte antigens (Jean Dausset and others) 1959-1962 - Discovery of antibody structure (independently elucidated by Gerald Edelman and Rodney Porter) 1959 - Discovery of lymphocyte circulation (James Gowans) 1960 - Discovery of lymphocyte "blastogenic transformation" and proliferation in response to mitogenic lectins-phytohemagglutinin (PHA) (Peter Nowell) 1961-1962 Discovery of thymus involvement in cellular immunity (Jacques Miller) 1961- Demonstration that glucocorticoids inhibit PHA-induced lymphocyte proliferation (Peter Nowell) 1963 - Development of the plaque assay for the enumeration of antibody-forming cells in vitro (Niels Jerne) (Albert Nordin) 1964-1968 T and B cell cooperation in immune response 1965 - Discovery of the first lymphocyte mitogenic activity, "blastogenic factor" (Shinpei Kamakura) and (Louis Lowenstein) (J. Gordon) and (L.D. MacLean) 1965 - Discovery of "immune interferon" (gamma interferon) (E.F. Wheelock) 1965 - Secretory immunoglobulins 1967 - Identification of IgE as the reaginic antibody (Kimishige Ishizaka) 1968 - Passenger leukocytes identified as significant immunogens in allograft rejection (William L. Elkins and Ronald D. Guttmann) 1969 - The lymphocyte cytolysis Cr51 release assay (Theodore Brunner) and (JeanCharles Cerottini) 1971 - Peter Perlmann and Eva Engvall at Stockholm University invented ELISA 1972 - Structure of the antibody molecule 1973 - Dendritic Cells first described by Ralph M. Steinman 1974 - T-cell restriction to major histocompatibility complex (Rolf Zinkernagel and (Peter C. Doherty) 1975 - Generation of the first monoclonal antibodies (Georges Köhler) and (César Milstein) 1976 - Identification of somatic recombination of immunoglobulin genes (Susumu Tonegawa) 1979 - Generation of the first monoclonal T cells (Kendall A. Smith) 1980-1983 - Discovery and characterization of the first interleukins, 1 and 2 IL-1 IL-2 (Kendall A. Smith) 1981 - Discovery of the IL-2 receptor IL2R (Kendall A. Smith) 1983 - Discovery of the T cell antigen receptor TCR (Ellis Reinherz) (Philippa Marrack) and (John Kappler) (James Allison) 1983 - Discovery of HIV (Luc Montagnier) 1984 - The first single cell analysis of lymphocyte proliferation (Doreen Cantrell) and (Kendall A. Smith) 1985-1987 - Identification of genes for the T cell receptor 1986 - Hepatitis B vaccine produced by genetic engineering 1986 - Th1 vs Th2 model of T helper cell function (Timothy Mosmann) 1988 - Discovery of biochemical initiators of T-cell activation: CD4- and CD8-p56lck complexes (Christopher E. Rudd) 1990 - Gene therapy for SCID 1991 - Role of peptide for MHC Class II structure ([Scheherazade Sadegh-Nasseri] & [Ronald N. Germain]) 1992- Discovery of transitional B cells (David Allman & Michael Cancro) 1994 - 'Danger' model of immunological tolerance (Polly Matzinger) 1995 - Regulatory T cells (Shimon Sakaguchi) 1995 - First dendritic cell vaccine trial reported by Mukherji et al. 1996-1998 - Identification of Toll-like receptors 2001 - Discovery of FOXP3 - the gene directing regulatory T cell development 2005 - Development of human papillomavirus vaccine (Ian Frazer) Scope of immunology Of the four major causes of death – injury, infection, degenerative disease and cancer – onl y the fi rst two regularl y kill their victims before child -bearing age, which means that they are a potential source of lost genes. Therefore any mechanism that reduces their effects has tremendous survival value, and we see this in the processes of, respectivel y, healing and immunity. Immunit y is concerned with the recognition and disposal of foreign or ‘non-self’ material that enters the body (represented by red arrows in the fi gure), usually in the form of life -threatening infectious microorganisms but sometimes, unfortunatel y, in the shape of a life -saving kidney graft. Resistance to infection may b e ‘innate’ (i.e. inborn and unchanging) or ‘acquired’ as the result of an adaptive immune response (centre). Immunology is the study of the organs, cells and molecules responsible for this recognition and disposal (the ‘immune system’), of how they respond and interact, of the consequences – desirable (top) or otherwise (bottom) – of their activit y, and of the ways in which they can be advantageously increased or reduced. By far the most important t ype of foreign material that needs to be recognized and disposed of is the microorganisms capable of causing infectious disease and, strictl y speaking, immunit y begins at the point when they enter the body. But it must be remembered that the fi rst line of defence is to keep them out, and a variet y of external defences have evolved for this purpose. Whether these are part of the immune s ystem is a purel y semantic question, but an immunologist is certainl y expected to know about them. Non-self A widel y used term in immunology, covering everything that is detectabl y different from an animal’s own constituents. Infectious microorganisms, together with cells, organs or other materials from another animal, are the most important non -self substances from an immunological viewpoint, but drugs and even normal foods, whic h are, of course, non -self too, can sometimes give rise to immunit y. Detection of non -self material is carried out by a range of receptor molecules (see Figs 11 –15). Infection Parasitic viruses, bacteria, protozoa, worms or fungi that attempt to gain acces s to the body or its surfaces are probabl y the chief raison d’être of the immune system. Higher animals with a damaged or defi cient immune system frequentl y succumb to infections that normal animals overcome. External defences The presence of intact skin on the outside and mucous membranes lining the hollow viscera is in itself a powerful barrier against entry of potentiall y infectious organisms. In addition, there are numerous antimicrobial (mainl y antibacterial) secretions in the skin and mucous surface s; these include l ysoz yme (also found in tears), lactoferrin, defensins and peroxidases. More specialized defences include the extreme acidit y of the stomach (about pH 2), the mucus and upwardl y beating cilia of the bronchial tree, and specialized surfactant proteins that recognize and clump bacteria that reach the lung alveoli. Successful microorganisms usuall y have cunning ways of breaching or evading these defences. Innate resistance Organisms that enter the body (shown in the fi gure as dots or rods) are often eliminated within minutes or hours by inborn, ever present mechanisms, while others (the rods in the fi gure) can avoid this and survive, and may cause disease unless they are dealt with by adaptive immunit y (see below). These mechanisms have evolv ed to dispose of pathogens (e.g. bacteria, viruses) that if unchecked can cause disease. Harmless microorganisms are usuall y ignored by the innate immune system. Innate immunit y also plays a vital role in initiating the adaptive immune response. Adaptive immune response The development or augmentation of defence mechanisms in response to a particular (‘specifi c’) stimulus, e.g. an infectious organism. It can result in elimination of the microorganism and recovery from disease, and often leaves th e host with specifi c memory, enabling it to respond more effectivel y on reinfection with the same microorganism, a condition called acquired resistance. Since the body has no prior way of knowing which microorganisms are and which are not harmless, all fo reign material is usuall y responded to as if it were harmful, including relativel y inoffensive pollens, etc. Vaccination A method of stimulating the adaptive immune response and generating memory and acquired resistance without suffering the full effects o f the disease. The name comes from vaccinia, or cowpox, used by Jenner to protect against smallpox. Grafting Cells or organs from another individual usuall y survive innate resistance mechanisms but are attacked by the adaptive immune response, leading to r ejection. Autoimmunity The body’s own (‘self’) cells and molecules do not normall y stimulate its adaptive immune responses because of a variet y of special mechanisms that ensure a state of self -tolerance, but in certain circumstances they do stimulate a re sponse and the body’s own structures are attacked as if they were foreign, a condition called autoimmunit y or autoimmune disease. Hypersensitivity Sometimes the result of specifi c memory is that re exposure to the same stimulus, as well as or instead of e liminating the stimulus, has unpleasant or damaging effects on the body’s own tissues. This is called hypersensitivit y; examples are allergies such as hay fever and some forms of kidney disease. Immunosuppression Autoimmunit y, hypersensitivit y and, above a ll, graft rejection sometimes necessitate the suppression of adaptive immune responses by drugs or other means. Immunohaematology -ABO and Rh factor. Immunohematology, more commonly known as blood banking is a branch of hematology which studies antigen-antibody reactions and analogous phenomena as they relate to the pathogenesis and clinical manifestations of blood disorders. A person employed in this field is referred to as an immunohematologist. Their day to day duties include blood typing, crossmatching and antibody identification CELLS OF THE IMMUNE RESPONSE Immune responsive cells can be divided into five groups based on i) the presence of specific surface components and ii) function: B-cells (B lymphocytes), T-cells (T lymphocytes), Accessory cells (Macrophages and other antigen-presenting cells), Killer cells (NK and K cells), and Mast cells. Some of the properties of each group are listed below. Cell group Surface components Surface immunoglobulin (Ag recognition) Immunoglobulin Fc receptor B-lymphocytes Function Direct antigen recognition Differentiation into Class II Major antibody-producing Histocompatability plasma cells Complex (MHC) molecule (Ag Antigen presentation within Class II MHC presentation) T-lymphocytes CD3 molecule T-cell receptor (TCR, humoral and cell- Ag recognition) mediated responses Involved in both Recognizes antigen presented within Class II MHC Helper T-cells (TH) CD4 molecule Promotes differentiation of Bcells and cytotoxic Tcells Suppressor T-cells (TS) CD8 molecule Activates macrophages Downregulates the activities of other cells Recognizes antigen presented within Class I Cytotoxic T-cells (CTL) CD8 molecule MHC Kills cells expressing appropriate antigen Accessory cells Variable Phagocytosis and cell killing Bind Fc portion of immunoglobulin (enhances phagocytosis) component C3b Immunoglobulin Fc (enhances receptor Macrophages Complement component C3b receptor Class II MHC molecule Bind complement phagocytosis) Antigen presentation within Class II MHC Secrete IL-1 (macrokine) promoting T-cell differentiation and proliferation Can be "activated" by T-cell lymphokines Dendritic cells Polymorphonuclear cells (PMNs) Class II MHC molecule Immunoglobulin Fc Antigen presentation within Class II MHC Bind Fc portion of receptor immunoglobulin Complement component (enhances C3b receptor phagocytosis) Bind complement component C3b (enhances phagocytosis) Killer cells NK cells Variable Direct cell killing Kills variety of target cells (e.g. tumor cells, Unknown virus-infected cells, transplanted cells) Bind Fc portion of immunoglobulin K cells Immunoglobulin Fc Kills antibody-coated target cells (antibody- receptor dependent cellmediated cytotoxicity, ADCC) Mast cells High affinity IgE Fc receptors Bind IgE and initiate allergic responses by release of histamine LYMPHOID TISSUES Primary Secondary (Responsible for maturation of Ag-reactive cells) Thymus Bone (T-cell marrow (Sites for Ag contact and response) Lymph nodes Spleen maturation) (Expansion of lymphatic system, (T-cell (B-cell maturation) maturation) separate from blood circulation. Deep cortex harbors mostly T-cells, superficial cortex harbors mostly Bcells) (Similar to lymph nodes but part of blood circulation. Collects blood-borne Ags) . NON IMMUNOLOGICAL DEFENSE MECHANISM Body Defenses • Physical barriers: skin & epithelial linings & cilia • Chemical: acids, mucous & lysozymes • Immune defenses – internal • • Innate, non-specific, immediate response (min/hrs) • Acquired – attack a specific pathogen (antigen) Steps in Immune defense • Detect invader/foreign cells • Communicate alarm & recruit immune cells • Suppress or destroy invader • Microbial killing by phagocytes: • Phagocytosis involves two steps namely attachment and ingestion. Following attachment of the organism, • invagination of the phagocyte results in the formation of a phagosome. Some capsulated bacteria don’t attach to the • phagocyte, but they can still be phagocytosed if they are coated with opsonins such as IgG and complement • component (C3b). The engulfed bacteria are held inside a vacuole called phagosome. The formation of phagosome • triggers respiratory bursts and fusion of lysosome with phagosome to form phagolysosome • The phagocytes appear to kill engulfed bacteria by two pathways, oxygen independent pathway and oxygen dependent pathway. The microbicidal mechanisms of the respiratory burst are termed oxygen dependent and phagolysosome formations are termed oxygen independent.Oxygen dependent mechanism involves catalytic conversion of molecular oxygen to oxyhalide free radicals, which are highly reactive oxidizing agents. The phagocyte oxidase present in the plasma membrane and phagolysosome reduce oxygen into reactive oxygen intermediates such as superoxide radicals. Superoxide is converted to H2O2,which is used by enzyme myeloperoxidase to convert unreactive halide ions to reactive hypohalous acids that are toxic to bacteria.Oxygen independent mechanism involves release of lysosomal contents into phagolysosomes. The content of lysosome includes lactoferrin, cathepsin G, lysozyme and defensins etc.In addition to the phagocyte oxidase system, macrophages have free-radical generating system, namely inducible nitric oxide synthase. This cytosolic enzyme is absent in resting macrophages but can be induced in response to bacterial lipopolysaccharides and IFN-γ. This enzyme catalyses the conversion of arginine to citrulline, and in the process releases nitric oxide gas. Nitric oxide may then combine with H2O2 or superoxide to form highly reactive peroxynitrite radicals that kill the microbes. Dendritic cells: These cells are derived from myeloid progenitor in the bone marrow and are morphologically identified by spiny membranous projection on their surfaces. Immature dendritic cells are located in epithelia of skin, gastrointestinal tract and respiratory tract and are called langerhan cells. They express low levels of MHC proteins on their surface and their main function is to capture and transport protein antigen to the draining lymph node. During their migration to the lymph node, dendritic cells mature into excellent antigen presenting cells (APC). Mature dendritic cells reside in the T cell area (paracortex) of the lymph node. Here, they are referred as interdigitating dendritic cells. These cells are distinct from the dendritic cells that occur in the germinal centers of lymphoid follicles (follicular dendritic cells) in lymph node, spleen and MALT. The follicular dendritic cells are not derived from the bone marrow and their role is to present antigen-antibody complex and complement products to B cell. Lymphoid system: Lymphoid organs are stationed throughout the body and are concerned with the growth, development and deployment of lymphocytes. These structurally and functionally diverse lymphoid organs and tissues are interconnected by the blood vessels and lymphatic vessels through which lymphocytes circulate. The organs involved in specific as well as non-specific immunity are classified as primary (central) lymphoid organs and secondary (peripheral) lymphoid organs. The blood and lymphatic vessels that carry lymphocytes to and from the other structures can also be considered lymphoid organs. Recently, it has become accepted that the liver is also a hematopoietic organ, giving rise to all leukocyte lineages. PRIMARY LYMPHOID ORGANS: Also called central lymphoid organs, these are responsible for synthesis and maturation of immunocompetant cells. These include the bone marrow and the thymus. BONE MARROW: All the cells of the immune system are initially derived from the bone marrow through a process called hematopoiesis. During foetal development hematopoiesis occurs initially in yolk sac and paraaortic mesenchyme and later in the liver and spleen. This function is taken over gradually by the bone marrow. During hematopoiesis, bone marrow-derived stem cells differentiate into either mature cells or into precursors of cells that migrate out of the bone marrow to continue their maturation in thymus. The bone marrow produces B cells, natural killer cells, granulocytes and immature thymocytes, in addition to red blood cells and platelets. It is both a primary and secondary lymphoid organ. The proliferation and maturation of precursor cells in the bone marrow are stimulated by cytokines, many of which are called colony stimulating factors (CSFs). The bone marrow also contains antibody secreting plasma cells, which have migrated from the peripheral lymphoid tissue. THYMUS: The thymus is a gland located in the anterior mediastinum just above the heart, which reaches its greatest size just prior to birth, then atrophies with age. This lymphoepithelial organ develops from ectoderm derived from the third branchial cleft and endoderm of the third branchial pouch. Immature lymphocytes begin to accumulate in the thymus of human embryos at about 90-100 days after fertilization. Initially most of these immature lymphocytes have come from the yolk sac and fetal liver rather than the bone marrow. Cells from the bone marrow, later migrate to the thymus as precursors and develop into mature peripheral T cells. Once the immature lymphocytes have passed the blood-thymus barrier they are called thymocytes. Mature T cells migrate from the thymus to secondary lymphoid organs such as lymph node, Peyer's patches and spleen. Ultimately the thymus becomes an encapsulated and consists of many lobes, each divided into an outer cortical region and an inner medulla. The cortex contains mostly immature thymocytes, some of which mature and migrate to the medulla, where they learn to discriminate between self and non-self during foetal development and for a short time after birth. T cells leave the medulla to enter the peripheral blood circulation, through which they are transported to the secondary lymphoid organs. About 98% of all T cells die in the thymus. The greatest rate of T cell production occurs before puberty. After puberty, the thymus shrinks and the production of new T cells in the adult thymus drops away. Children with no development of thymus suffer from DiGeorge syndrome that is characterized by deficiency in T cell development but normal numbers of B cells. PERIPHERAL LYMPHOID ORGANS: While primary lymphoid organs are concerned with production and maturation of lymphoid cells, the secondary or peripheral lymphoid organs are sites where the lymphocytes localise, recognise foreign antigen and mount response against it. These include the lymph nodes, spleen, tonsils, adenoids, appendix, and clumps of lymphoid tissue in the small intestine known as Peyer's patches. They trap and concentrate foreign substances, and they are the main sites of production of antibodies. Some lymphoid organs are capsulated such as lymph node and spleen while others are noncapsulated, which include mostly mucosa-associated lymphoid tissue (MALT). LYMPH NODE: Clusters of lymph nodes are strategically placed in the neck, axillae, groin, mediastinum and abdominal cavity, where they filter antigens from the interstitial tissue fluid and the lymph during its passage from the periphery to the thoracic duct. The key lymph nodes are the axillary lymph nodes, the inguinal lymph nodes, the mesenteric lymph nodes and the cervical lymph nodes. Lymph nodes that protect the skin are termed somatic nodes, while deep lymph nodes protecting the respiratory, digestive and genitourinary tracts are termed visceral nodes. Each lymph node is surrounded by a fibrous capsule that is pierced by numerous afferent lymphatics that drain lymph into marginal sinus. The lymph flows through the medullary sinus and leaves through efferent lymphatics. Each lymph node is divided into an outer cortex, inner medulla and intervening paracortical region. The cortex is also referred as B cell area, which mainly consists of B cells. The cortex is a high traffic zone where recirculating Tand B lymphocytes enter from the blood. Aggregates of cells called follicles are present in the cortex, which in turn may have central areas called germinal centers. Follicles without germinal centers are called primary follicles and those with germinal centers are called secondary follicles. Primary follicles are rich in mature but resting B cells. Germinal centers develop in response to antigenic stimulation and consist of follicular dendritic cells and reactive B cells. The medulla contains a mixture of B cells, T cells, plasma cells and macrophages. The medulla consists of medullary cords that lead to the medullary sinus. The cords are populated by plasma cells and macrophages. Between these two zones, lie the paracotex (T cell area) that contains T lymphocytes, dendritic cells and mononuclear phagocytes. Most of the T cells (70%) located there are CD4+ helper cells. SPLEEN: Situated in the left upper quadrant of the abdomen and weighing about 150 grams, spleen is the largest single lymphoid organ in the body. It has a dense fibrous capsule with muscular trabeculae extending inward to subdivide the spleen into lobules. It filters blood and is the major organ in which antibodies are synthesized and released into circulation. In addition to capturing foreign antigens from the blood that passes through the spleen, migratory macrophages and dendritic cells also bring antigens to the spleen via the bloodstream. Persons lacking spleen (eg. splenectomy) are highly susceptible to infections with capsulated bacteria such as pneumococci and meningococci. Spleen is the major site for phagocytosis of antibody coated bacteria and destruction of aged RBCs. It is supplied by splenic artery, which pierces the capsule at hilum and divides into smaller branches that are surrounded by fibrous trabeculae. The spleen is composed of two types of tissue, the red pulp and the white pulp. The red pulp contains vascular sinusoids, large number of erythrocytes, resident macrophages, dendritic cells, granulocytes, few plasma cells and lymphocytes. It is the site where aged platelets and erythrocytes are destroyed. The white pulp contains the lymphoid tissue clustered around small arterioles and is known as a periarteriolar lymphoid sheath (PALS). PALS contain mainly T lymphocytes, about 75% of which are CD4+ helper T cells. Attached to this are lymphoid follicles, some of which contain germinal centers. Follicles and germinal center predominantly contain B cells. The PALS and follicles are surrounded by rim of lymphocytes and macrophages,called marginal zone. Marginal zone is composed of macrophages, B cells, and CD4+ helper T cells. The arterioles end in vascular sinusoids in the red pulp, which in turn end in venules that drain into splenic vein. Antigens and lymphocytes enter the spleen through vascular sinusoids. Activation of B cells occurs at the juncton between follicle and PALS. Activated B cells then migrate to the germinal centers or into the red pulp. MUCOSA ASSOCIATED LYMPHOID TISSUE (MALT): Approximately >50% of lymphoid tissue in the body is found associated with the mucosal system. MALT is composed of gut-associated lymphoid tissues (GALT) lining the intestinal tract, bronchusassociated lymphoid tissue (BALT) lining the respiratory tract, and lymphoid tissue lining the genitourinary tract. The respiratory, alimentary and genitourinary tracts are guarded by subepithelial accumulations of lymphoid tissue that are not covered by connective tissue capsule. They may occur as diffuse collections of lymphocytes, plasma cells and phagocytes throughout the lung and lamina propria of intestine or as clearly organised tissue with well-formed lymphoid follicles. The well-formed follicles include the tonsils (lingual, palatine and pharyngeal), Peyer’s patches in the intestine and appendix. The major function of these organs is to provide local immunity by way of sIgA (also IgE) production. Diffuse accumulations of lymphoid tissue are seen in the lamina propria of the intestinal wall. The intestinal epithelium overlying the Peyer's patches is specialized to allow the transport of antigens into the lymphoid tissue. This function is carried out by cuboidal absorptive epithelial cells termed "M" cells, so called because they have numerous microfolds on their luminal surface. M cells endocytose, transport and present antigens to subepithelial lymphoid cells. Majority of intra-epithelial lymphocytes are T cells, and most often CD8+ lymphocytes. The intestinal lamina propria contains CD4+ lymphocytes, large number of B cells, plasma cells, macrophages, dendritic cells, eosinophils and mast cells. Peyer’s patches contain both B cells and CD4+ T cells. LYMPHOCYTES: Lymphocytes are stem cells derived cells that mature either in the bone marrow or thymus. Together, the thymus and marrow bone marrow produce approximately 109 mature lymphocytes each day and the adult human body contains approximately 1012 lymphocytes. Lymphocytes comprise 20-40% (1000 - 4000 cells/μl) of all leukocytes. The lymphocytes are distributed to blood, lymph and lymphoid organs. Typically, lymphocyte is small, round, cell with diameter of 5-10μm, spherical nucleus, densely compacted nuclear chromatin and scanty cytoplasm. Though the cytoplasm contains mitochondria and ribosomes, other organelles are not detectable. Such mature but resting lymphocytes are known as naïve cells. They are mitotically inactive but when stimulated can undergo cell division. Naïve lymphocytes have a short life span and die in few days after leaving bone marrow or thymus unless they are stimulated. Once the lymphocyte is activated (stimulated), they become large (10-12μm), have more cytoplasm and more organelles. Activated lymphocytes may undergo several successive rounds of cell division over a period of several days. Some of the progeny cells revert to the resting stage and become memory cells, but can survive for several years in the absence of any antigenic stimulus. There are three major types of lymphocyte, B lymphocyte, T lymphocyte and NK cells. Different lymphocytes are identified by certain protein markers on their surface called "cluster of differentiation" or "CD" system. One marker that all leukocytes have in common is CD45. The presence of the markers can be detected using specific monoclonal antibodies. Distribution of lymphocytes Approximate % Tissue T-Cells B-Cells NK Cells Peripheral blood 70-80 10-15 10-15 Bone marrow 5-10 80-90 5-10 Thymus 99 <1 <1 Lymph node 70-80 20-30 <1 Spleen 30-40 50-60 1-5 B LYMPHOCYTE: Also called B-cells, they are so called because in birds they were found to mature in bursa of fabricius. Humans don’t have an anatomical equivalent to bursa, but the development and maturation of these cells occur in bone marrow. © Sridhar Rao P.N (www.microrao.com) Ontogeny: In mammals, the early stages of B cell maturation occur in the fetal liver and bone marrow. B cell development begins in the fetal liver and continues in the bone marrow throughout life. The stages in B cell development in the bone marrow are: Stem cell > pro-B cell > pre-B cell > small pre-B cell > immature B cell > mature B cell. Distribution: They account for 5-15% of lymphocytes (250 cells/μl) in circulation and 80-90% in bone marrow, 20-30% in lymph node and 50-60% in spleen. Surface markers: The most important surface marker on the surface of mature B cell is the surface immunoglobulin. The surface immunoglobulins are of IgM and IgD type. A B cell will have approximately 109 immunoglubulins of single specificity on its surface. Markers/Receptors on B cells are Surface Immunoglobulin (IgM and IgD), CD40, B7, ICAM-1, LFA-1, MHC II, CD32 (Ig Fc receptor), CD35 (Receptor for complement component) and additional markers that distinguish B cells such as CD19, CD20, CD21 and CD22. Demonstration of B cells: EAC (Erythrocyte Amboceptor Complement) Rosettes: When sheep RBCs coated with antibody and treated with complement and B cells, a rosette is formed due to the presence of complement receptor on B cells. B cells can be demonstrated by immunofluorescence with fluorescent-labelled monoclonal antibodies against surface markers such as surface immunoglobulin. On stimulation by pokeweed mitogen, they undergo blast transformation. Functions of B-cells: Direct antigen recognition and Antigen presentation B cells may differentiate into plasma cells (which secrete large amounts of antibodies) or into memory B cells. Memory cells can survive 20 years or more. Plasma cells: These are the effector cells of the B-cell lineage and are specialised in secreting immunoglobulins. When activated B cells divide, some of its progeny become memory cells and the reminder become immunoglobulin-secreting plasma cells. Plasma cells are oval or egg shaped, have eccentrically placed nuclei, have abundant cytoplasm containing dense rough endoplasmic reticulum (the site of antibody production), perinuclear Golgi body (where immunoglobulins are converted to final form and packaged). Unlike B cells, immunoglobulins are not present on the surface of plasma cells. They have a short life span of few days to few weeks. © Sridhar Rao P.N (www.microrao.com) T LYMPHOCYTE: Ontogeny: The name "T-cell" is an abbreviation of "thymus dependent lymphocyte". T lymphocytes arise in the bone marrow as T-cell precursors, then migrate to and mature in the thymus. After entry into the thymus T-cell precursors are also referred to as "thymocytes". In the thymus there are rearrangements at gene segments coding for the variable part of the TCR (T Cell Receptor) resulting in generation of diversity. T Cell Receptors are then expressed on the surface, which is followed by expression of either CD8 or CD4 surface molecules. Those cells expressing receptors that can interact with self MHC molecules are positively selected while those cells that express receptors that recognize peptides derived from self protein in association with self MHC are negatively selected. Such cells undergo clonal deletion or anergy. Distribution: T cell accounts for 70-80% (1500 cells/μl) lymphocytes in peripheral blood, 5-10% in bone marrow, 70-80% in lymph node and 30-40% in spleen. Surface markers: The most important surface receptor is TCR. TCR are polypeptides that belong to the immunoglobulin superfamily. There are two kinds of TCR, one composed of a α-β heterodimer (TCR2) and the other composed of a γ-δ heterodimer (TCR1). An individual T cell can express either α-β or γ-δ as its receptor but never both. 95% of T cells express the α-β heterodimer. The other markers/receptors present on the surface are IL-2R, IL1R, CD2, CD3, CD4/CD8, CD28, ICAM-1 and LFA-1. Nearly all the mature T lymphocytes express both CD2 and CD3 on their surface. CD3, which is always found closely associated with TCR, is necessary for signal transduction following antigen recognition by the TCR. Subsets of T Cells: There are two major types of T cells, Helper (CD4) and Cytotoxic/Suppressor (CD8) T cells. CD4 cells account for 45% (900/μl) of lymphocytes while CD8 cells account for 30% (600/μl). � Helper T cells (TH) secrete cytokines that promote the proliferation and differentiation of cytotoxic T cells, B cells and macrophages and activation of inflammatory leukocytes. TH cells are identified by the presence of the CD4 marker. They recognize antigen when presented along with Class II MHC molecules. TH cells are further subdivided into the TH1 and TH2 subsets on the basis of the kinds of cytokines they produce. TH1 cells produce interleukin-2 (IL-2), interferon-gamma (IFNγ), and tumour necrosis factor-beta (TNF-β) while TH2 cells produce IL-4, IL-5, IL-6, IL-10 and TGF-β. � Cytotoxic T cells (TC) lyse cells with foreign antigens, e.g. tumour cells, virus-infected cells, and foreign tissue grafts. TC cells are identified by the presence of the CD8 marker. They recognize antigen presented when presented along with Class I MHC molecules. The suppressor T cells have a role in downregulation of immune response. Demonstration of T cells: � -labelled monoclonal antibodies against TCR or other surface markers. � -Rosette/ SRBC rosette: T cells bind to sheep RBCs at 37oC forming rosettes. � (PHA) or Concanavalin A. © Sridhar Rao P.N (www.microrao.com) Functions of Helper T-cells (TH): Promotes differentiation of B-cells and cytotoxic T-cells Activates macrophages Functions of Cytotoxic/Suppressor T-cells (CTL): Kills cells expressing appropriate antigen Downregulates the activities of other cells NK CELLS (LARGE GRANULAR LYMPHOCYTES): Also called Large Granular Lymphocytes (LGLs), these are large lymphocytes containing azurophilic granules in the cytoplasm. NK cells derive form bone marrow but don't require thymus for development. NK cells are so called because they kill variety of target cells (such as tumour cells, virus-infected cells, transplanted cells) without the participation of MHC molecules. They can kill target cell without a need for activation unlike cytotoxic T lymphocytes. Hence they mediate a form of natural (innate) immunity. Distribution: They account for 10-15% of blood lymphocytes. They are rare in lymph nodes and don't circulate through lymph. Surface markers: NK cells lack any surface immunoglobulins, TCR or CD4 makers; instead they have CD16 (Immunoglobulin Fc receptor) and CD56. Approximately 50% of human NK cells express only one form of CD8. Other receptors include IL-2R, CD2, ICAM-1 and LFA-1. Functions: NK cells are activated by recognition of antibody-coated cells, virus infected cell, cell infected with intracellular bacteria and cells lacking MHC I proteins. Activation of NK cell results in cytolysis of target and cytokine secretion but no clonal expansion. Interestingly, NK cells are inhibited on contact with MHC I proteins. NK cells can kill antibody-coated target cells, which is mediated through Fc receptor present on its surface. This is called antibody-dependent cell cytotoxicity (ADCC). NK cells also participate in Graft vs Host reaction in recipient of bone marrow transplants. NK cells can be activated by IL-2 so that their cytotoxic capacity is enhanced. Such cells are called Lymphokine Activated Killer cells (LAK) and have been used clinically to treat tumours. LAK cells have enhanced cytolytic activity and are effective against wide range of tumour cells. Activated NK cells produce cytokines such as IFN-γ, TNFα, GM-CSF and CSF-1 all of which are immunomodulators. LYMPHOCTE RECIRCULATION: The movement of lymphocytes via the blood stream and lymphatics from peripheral tissue to another is called lymphocyte recirculation. Lymphocytes are migratory cells; mature lymphocytes continually migrate in and out of all peripheral lymphoid tissue. At an average each cell changes location once or twice each day. At any given point of time 1-2% of lymphocytes will be in transit. In most lymphoid organs, they enter through blood and exit through lymphatics, but in spleen they enter and leave directly through blood. As lymphocytes migrate, they can survey the body for foci of infection or presence of foreign antigens. Such a movement also helps to maintain a balance in distribution of lymphocytes in the body. Cell-mediated immunity The second arm of the immune response is refered to as CellMediated Immunity (CMIR). As the name implies, the functional "effectors" of this response are various immune cells. Cell mediated immunity is produced by the sensetised involve antibodies or complement but lymphocytes rather . involves It the is an immune activation of response that does macrophages, natural not killer cells (NK), antigen-specific cytotoxic T-lymphocytes, and the release of various cytokines in response to an antigen and this results in the lysis of the microbial antigens. Historically, the immune system was separated into two branches: humoral immunity, for which the protective function of immunization could be found in the humor (cell-free bodily fluid or serum) and cellular immunity, for which the protective function of immunization was associated with cells. CD4 cells or helper T cells provide protection against different pathogens. If an individual is exposed to a particularantigan for the second time, immune response occurs more quickly and more abundantly than during the first exposure. This is known as the secondary response. Both humoral and cell mediated immunity are associated with immunologic memory that is the immune system is able to retain the memory of the first antigenic exposure and there by during the secons similar exposure it produces a quick response. Cellular immunity protects the body by: apoptosis in body cells displaying epitopes of foreign antigen on their surface, such as virus-infected cells, cells with intracellular bacteria, and cancer cells displaying tumor antigens; activating macrophages and natural killer cells, enabling them to destroy intracellular pathogens stimulating cells to secrete a variety of cytokines that influence the function of other cells involved in adaptive immune responses and innate immune responses. Cell-mediated immunity is directed primarily at microbes that survivein phagocytes and microbes that infect non-phagocytic cells. It is most effective in removing virus-infected cells, but also participates in defending against fungi, protozoans, cancers, and intracellular bacteria. It also plays a major role in transplant rejection. These functions include: Phagocytosis and killing of intracellular pathogens Direct cell killing by NK and K cells Direct cell killing by cytotoxic T cells These responses are especially important for destroying intracellular bacteria, eliminating viral infections and destroying tumor cells. CELLS OF IMMUNE SYSTEM The immune system operates by producing cells.The important cells as follows LYMPHOCYTES Lymphocytes are the mononucleate, nongranular leukocytes of lymphoid tissue, participating in immunity. They are found in blood, lymph and lymphoid tissues such as spleen, lymph nodes, tonsils, peyers patches etc. They are spherical or ovoid in shape. They have a diameter of 7 to 12 microns. They have a large nucleus and cytoplasm. The lymphocyes are of three types. They are B lymphocytes, Tlymphocytes and null cells.T he null cells constitute about 3%, the B cells about 27% and the T cells about 70% of the total T lymphocytes. The B lymphocytes mature in bursa of Fabricus in birds or in bone marrow of mammals. The B lymphocytes produce antibodies and hence they are responsible for humoral immunity. The B cells kill bactreria, virus etc The T lyphocytes mature in the thymus under the influence of thymic hormones. The T lymphocytes bring about the cell mediated immunity. The T cells are responsible for the killing of cancer cells,killing viral infected cells, allograft etc. The null cells form a third population of lymphocytes. They are intermediate between T and B cells. They have cytotoxic activity. B LYMPHOCYTES The lymphocytes that mature in bursa of fabricius or bone marrow and that brings about humoral immunity is called B lymphocytes. The B lymphocytes have a large nucleus. They are found in the blood ad lymph. But they are highly concentrated in lymph nodes and spleen. They contain surface immunoglobulins. The B lymphocytes have the following markers. Ia(immune associated) protein which binds with the Ia receptor of the T lymphocytes. IgM. Fc protein to bind with the Fc fragment of the immunoglobulin CRI and CR3 receptors of complement system. Surface immunoglobulins The immature B cell changes in to mature B cell which has IgD molecules on the surface in addition to PLASMA CELLS These are the end cells of the B lymphocytes. They secrete immunoglobulins. They are very rarely seen in the plasma of blood but are but are found mainly in the lymph nodes and spleenThe cytoplasm is completely filled with rough endoplasmic reticulam. This is a site of protein synthesis namely synthesis of immunoglobulins. MACROPHAGE ACTIVATION Macrophages are the large mononuclear phagocytic cells derived from monocytes. They are components of the reticuloendothelial system. They are distributed through out the body but concentrated in lymph nodes, spleen, bone marrow and liver. They are large lymphoid cells. They have large nucleus. They contain large number of lysosomes. While the production of antibody through the humoral immune response can effectively lead to the elimination of a variety of pathogens, bacteria that have evolved to invade and multiply within phagocytic cells of the immune response pose a different threat. The following graphics illustrate this dilemma: Non-encapsulated microorganisms are easily phagocytosed and killed within macrophages. Encapsulated microorganisms require the production of antibody in order to be effectively phagocytosed. Once engul however, they are easily killed. cellular microorganisms Intracellular microorganisms elicit the production of antibody, which allows effective phagocytosis. Once engul however, they survive within the phagocyte and eventually kill it. IFN TNF Intracellular microorganisms also activate specific T-cells, which then release lymphokines (e.g. IFN, TNF) that ca macrophage activation. Activated ("killer") macrophages are then very effective at destroying the intracellular pathogens This process can be further illustrated by considering the following experiment known as "Koch's phenomenon". Inoculation of an unimmunized guinea pig with a lethal dose of the intracellular pathogen Mycobacterium tuberculosis (MT) results in death of the animal. Inoculation with a sub-lethal dose induces immunity.Inoculation of an MT-immunized guinea pig with a lethal dose of MT causes a local reaction ("delayed hypersensitivity") one to two days later. Inoculation of an MT-immunized guinea pig with a lethal dose of a different intracellular pathogen, Listeria monocytogenes (LM) again results in death of the animal.Inoculation of an MT-immunized guinea pig with a lethal dose of LM and MT causes a delayed hypersensitivity reaction.These results demonstrate the specific (T-cell mediated) and non-specific (macrophage mediated) aspects of this type of cell mediated immunity. T LYMPHOCYTES The mononucleated non granular leukocyte that matures in thymus and that bringa about cell mediated immunity is called T lymphocyte. They vare highly concentrated in blood and spleen. The T cell markers as follows. Erythocyte receptor- It recognizes the sheep erythrocytes T cell antigen receptor – It recognizes MHC antigens The Ia protein receptor etc 1. T helper cells They are sub population of T lymphocytes that help B cells and T cells in immune responses They are regulator cells. They help the B and T cells in many ways . The t helper cells contain glycoprotein molecules called CD4 molecules on the urface. The HIV infects mainly these cells. The TH cells are activated by very small quantities of antigen which can not activate other cells. They secrete lymphokines. 2. T suppressor cells These cells are a sub population of T cells that suppresses the activity of B cells and other T Cells. They are the regulatory T cells. They inhibit antibody production by B cells. They suppress the functions of the T killer cells and T helper cells. They are responsible for immune tolerance by limiting the ability of the immune system to attack a persons own bodt tissue. CELL MEDIATED CYTOTOXICITY The second half of the cell-mediated immune response is involved in rejection of foreign grafts and the elimination of tumors and virus-infected cells. The effector cells involved in these processes are cytotoxic T-lymphocytes (CTLs), NKcells and K-cells. Each of these effector cells recognizes their target by different means, described below. Cytotoxic T-lymphocytes CTLs, like other T-cells are both antigen and MHC-restricted. That is, CTLs require i) recognition of a specific antigenic determinant and ii) recognition of "self" MHC (Click here to review these requirements). Briefly, CTLs recognize antigen via their T-cell receptor. This receptor makes specific contacts with the antigenic determinant and the target cell's class I MHC molecule. CTLs also express CD8, which may assist the antigen recognition process. Once recognition is successful, the CTL "programs" the target cell for selfdestruction. This process is thought to occur in one of several possible ways. First, CTLs may release a substance known as perforin in the space between the CTL and its target. In the presence of calcium ions, the perforin polymerizes, forming channels in the target cell's membrane. These channels may cause the target cell to lyse. Second, the CTL may also release various enzymes that pass through the polyperforin channels, causing target cell damage. Third, the CTL may release lymphokines and/or cytokines that interact with specific receptors on the target cell surface, causing internal responses that lead to destruction of the target cell. CTLs principally act to eliminate endogenous antigens. NULL CELLS These are lymphocytes with cytotoxic properties. They are neither B cells or T cells. They are intermediate between these. They form less than 3%. Two types namely natural killer cells and killer cells. NK-CELLS NK cells are part of a group know as the "large granular lymphocytes". These cells are generally non-specific, MHC-unrestricted cells involved primarily in the elimination of neoplastic or tumor cells. The precise mechanism by which they recognize their target cells is not clear. Probably, there is some type of NK-determinant expressed by the target cells that is recognized by an NK-receptor on the NK cell surface. Once the target cell is recognized, killing occurs in a manner similar to that produced by the CTL. K-CELLS K-cells are probably not a separate cell type but rather a separate function of the NK group. K-cells contain immunoglobulin Fc receptors on their surface and are involved in a process known as Antibody-dependent Cellmediated Cytotoxicity (ADCC). ADCC occurs as a consequence of antibody being bound to a target cell surface via specific antigenic determinants expressed by the target cell. Once bound, the Fc portion of the immunoglobulin can be recognized by the K-cell. Killing then ensues by a mechanism similar to that employed by CTLs. This type of CMIR can also result in Type II hypersensitivities. UNIT-II Antibody Antibodies (also known as immunoglobulins[1], abbreviated Ig) are gamma globulin proteins that are found in blood or other bodily fluids of vertebrates, and are used by the immune system to identify and neutralize foreign objects, such as bacteria and viruses. They are typically made of basic structural units—each with two large heavy chains and two small light chains—to form, for example, monomers with one unit, dimers with two units or pentamers with five units. Antibodies are produced by a kind of white blood cell called a plasma cell. There are several different types of antibody heavy chains, and several different kinds of antibodies, which are grouped into different isotypes based on which heavy chain they possess. Five different antibody isotypes are known in mammals, which perform different roles, and help direct the appropriate immune response for each different type of foreign object they encounter.[2] Though the general structure of all antibodies is very similar, a small region at the tip of the protein is extremely variable, allowing millions of antibodies with slightly different tip structures, or antigen binding sites, to exist. This region is known as the hypervariable region. Each of these variants can bind to a different target, known as an antigen.[3] This huge diversity of antibodies allows the immune system to recognize an equally wide variety of antigens. The unique part of the antigen recognized by an antibody is called the epitope. These epitopes bind with their antibody in a highly specific interaction, called induced fit, that allows antibodies to identify and bind only their unique antigen in the midst of the millions of different molecules that make up an organism. Recognition of an antigen by an antibody tags it for attack by other parts of the immune system. Antibodies can also neutralize targets directly by, for example, binding to a part of a pathogen that it needs to cause an infection.[4] The large and diverse population of antibodies is generated by random combinations of a set of gene segments that encode different antigen binding sites (or paratopes), followed by random mutations in this area of the antibody gene, which create further diversity.[2][5] Antibody genes also re-organize in a process called class switching that changes the base of the heavy chain to another, creating a different isotype of the antibody that retains the antigen specific variable region. This allows a single antibody to be used by several different parts of the immune system. Production of antibodies is the main function of the humoral immune system. Forms Surface immunoglobulin (Ig) is attached to the membrane of the effector B cells by its transmembrane region, while antibodies are the secreted form of Ig and lack the trans membrane region so that antibodies can be secreted into the bloodstream and body cavities. As a result, surface Ig and antibodies are identical except for the transmembrane regions. Therefore, they are considered two forms of antibodies: soluble form or membrane-bound form (Parham 21-22). The membrane-bound form of an antibody may be called a surface immunoglobulin (sIg) or a membrane immunoglobulin (mIg). It is part of the B cell receptor (BCR), which allows a B cell to detect when a specific antigen is present in the body and triggers B cell activation.[7] The BCR is composed of surface-bound IgD or IgM antibodies and associated Ig-α and Ig-β heterodimers, which are capable of signal transduction.[8] A typical human B cell will have 50,000 to 100,000 antibodies bound to its surface.[8] Upon antigen binding, they cluster in large patches, which can exceed 1 micrometer in diameter, on lipid rafts that isolate the BCRs from most other cell signaling receptors.[8] These patches may improve the efficiency of the cellular immune response.[9] In humans, the cell surface is bare around the B cell receptors for several thousand ångstroms,[8] which further isolates the BCRs from competing influences. Immunoglobulin A Isotypes Name Types IgA 2 IgD 1 Antibody Complexes IgE 1 IgG 4 IgM 1 Antibodies can come in different varieties known as isotypes or classes. In placental mammals there are five antibody isotypes known as IgA, IgD, IgE, IgG and IgM. They are each named with an "Ig" prefix that stands for immunoglobulin, another name for antibody, and differ in their biological properties, functional locations and ability to deal with different antigens, as depicted in the table.[13] The antibody isotype of a B cell changes during cell development and activation. Immature B cells, which have never been exposed to an antigen, are known as naïve B cells and express only the IgM isotype in a cell surface bound form. B cells begin to express both IgM and IgD when they reach maturity—the co-expression of both these immunoglobulin isotypes renders the B cell 'mature' and ready to respond to antigen.[14] B cell activation follows engagement of the cell bound antibody molecule with an antigen, causing the cell to divide and differentiate into an antibody producing cell called a plasma cell. In this activated form, the B cell starts to produce antibody in a secreted form rather than a membrane-bound form. Some daughter cells of the activated B cells undergo isotype switching, a mechanism that causes the production of antibodies to change from IgM or IgD to the other antibody isotypes, IgE, IgA or IgG, that have defined roles in the immune system. Structure Antibodies are heavy (~150 kDa) globular plasma proteins. They have sugar chains added to some of their amino acid residues.[15] In other words, antibodies are glycoproteins. The basic functional unit of each antibody is an immunoglobulin (Ig) monomer (containing only one Ig unit); secreted antibodies can also be dimeric with two Ig units as with IgA, tetrameric with four Ig units like teleost fish IgM, or pentameric with five Ig units, like mammalian IgM.[16] Several immunoglobulin domains make up the two heavy chains (red and blue) and the two light chains (green and yellow) of an antibody. The immunoglobulin domains are composed of between 7 (for constant domains) and 9 (for variable domains) β-strands. See also: The variable parts of an antibody are its V regions, and the constant part is its C region. Immunoglobulin domains The Ig monomer is a "Y"-shaped molecule that consists of four polypeptide chains; two identical heavy chains and two identical light chains connected by disulfide bonds.[13] Each chain is composed of structural domains called immunoglobulin domains. These domains contain about 70-110 amino acids and are classified into different categories (for example, variable or IgV, and constant or IgC) according to their size and function.[17] They have a characteristic immunoglobulin fold in which two beta sheets create a “sandwich” shape, held together by interactions between conserved cysteines and other charged amino acids. Heavy chain There are five types of mammalian Ig heavy chain denoted by the Greek letters: α, δ, ε, γ, and μ.[3] The type of heavy chain present defines the class of antibody; these chains are found in IgA, IgD, IgE, IgG, and IgM antibodies, respectively.[4] Distinct heavy chains differ in size and composition; α and γ contain approximately 450 amino acids, while μ and ε have approximately 550 amino acids.[3] 1. Fab region 2. Fc region 3. Heavy chain (blue) with one variable (VH) domain followed by a constant domain (CH1), a hinge region, and two more constant (CH2 and CH3) domains. 4. Light chain (green) with one variable (VL) and one constant (CL) domain 5. Antigen binding site (paratope) 6. Hinge regions. In birds, the major serum antibody, also found in yolk, is called IgY. It is quite different from mammalian IgG. However, in some older literature and even on some commercial life sciences product websites it is still called "IgG", which is incorrect and can be confusing. Each heavy chain has two regions, the constant region and the variable region. The constant region is identical in all antibodies of the same isotype, but differs in antibodies of different isotypes. Heavy chains γ, α and δ have a constant region composed of three tandem (in a line) Ig domains, and a hinge region for added flexibility;[13] heavy chains μ and ε have a constant region composed of four immunoglobulin domains.[3] The variable region of the heavy chain differs in antibodies produced by different B cells, but is the same for all antibodies produced by a single B cell or B cell clone. The variable region of each heavy chain is approximately 110 amino acids long and is composed of a single Ig domain. Light chain . In mammals there are two types of immunoglobulin light chain, which are called lambda (λ) and kappa (κ).[3] A light chain has two successive domains: one constant domain and one variable domain. The approximate length of a light chain is 211 to 217 amino acids.[3] Each antibody contains two light chains that are always identical; only one type of light chain, κ or λ, is present per antibody in mammals. Other types of light chains, such as the iota (ι) chain, are found in lower vertebrates like Chondrichthyes and Teleostei. CDRs, Fv, Fab and Fc Regions Some parts of an antibody have unique functions. The arms of the Y, for example, contain the sites that can bind two antigens (in general identical) and, therefore, recognize specific foreign objects. This region of the antibody is called the Fab (fragment, antigen binding) region. It is composed of one constant and one variable domain from each heavy and light chain of the antibody.[18] The paratope is shaped at the amino terminal end of the antibody monomer by the variable domains from the heavy and light chains. The variable domain is also referred to as the FV region and is the most important region for binding to antigens. More specifically, variable loops of β-strands, three each on the light (VL) and heavy (VH) chains are responsible for binding to the antigen. These loops are referred to as the complementarity determining regions (CDRs). In the framework of the immune network theory, CDRs are also called idiotypes. According to immune network theory, the adaptive immune system is regulated by interactions between idiotypes. The base of the Y plays a role in modulating immune cell activity. This region is called the Fc (Fragment, crystallizable) region, and is composed of two heavy chains that contribute two or three constant domains depending on the class of the antibody.[3] Thus, the Fc region ensures that each antibody generates an appropriate immune response for a given antigen, by binding to a specific class of Fc receptors, and other immune molecules, such as complement proteins. By doing this, it mediates different physiological effects including opsonization, cell lysis, and degranulation of mast cells, basophils and eosinophils.[13][19] Function Activated B cells differentiate into either antibody-producing cells called plasma cells that secrete soluble antibody or memory cells that survive in the body for years afterward in order to allow the immune system to remember an antigen and respond faster upon future exposures.[20] At the prenatal and neonatal stages of life, the presence of antibodies is provided by passive immunization from the mother. Early endogenous antibody production varies for different kinds of antibodies, and usually appear within the first years of life. Since antibodies exist freely in the bloodstream, they are said to be part of the humoral immune system. Circulating antibodies are produced by clonal B cells that specifically respond to only one antigen (an example is a virus capsid protein fragment). Antibodies contribute to immunity in three ways: they prevent pathogens from entering or damaging cells by binding to them; they stimulate removal of pathogens by macrophages and other cells by coating the pathogen; and they trigger destruction of pathogens by stimulating other immune responses such as the complement pathway.[21] The secreted mammalian IgM has five Ig units. Each Ig unit (labeled 1) has two epitope binding Fab regions, so IgM is capable of binding up to 10 epitopes. Activation of complement Antibodies that bind to surface antigens on, for example, a bacterium attract the first component of the complement cascade with their Fc region and initiate activation of the "classical" complement system.[21] This results in the killing of bacteria in two ways.[6] First, the binding of the antibody and complement molecules marks the microbe for ingestion by phagocytes in a process called opsonization; these phagocytes are attracted by certain complement molecules generated in the complement cascade. Secondly, some complement system components form a membrane attack complex to assist antibodies to kill the bacterium directly.[22] Activation of effector cells To combat pathogens that replicate outside cells, antibodies bind to pathogens to link them together, causing them to agglutinate. Since an antibody has at least two paratopes it can bind more than one antigen by binding identical epitopes carried on the surfaces of these antigens. By coating the pathogen, antibodies stimulate effector functions against the pathogen in cells that recognize their Fc region.[6] Those cells which recognize coated pathogens have Fc receptors which, as the name suggests, interacts with the Fc region of IgA, IgG, and IgE antibodies. The engagement of a particular antibody with the Fc receptor on a particular cell triggers an effector function of that cell; phagocytes will phagocytose, mast cells and neutrophils will degranulate, natural killer cells will release cytokines and cytotoxic molecules; that will ultimately result in destruction of the invading microbe. The Fc receptors are isotype-specific, which gives greater flexibility to the immune system, invoking only the appropriate immune mechanisms for distinct pathogens.[3] Natural antibodies Humans and higher primates also produce “natural antibodies” which are present in serum before viral infection. Natural antibodies have been defined as antibodies that are produced without any previous infection, vaccination, other foreign antigen exposure or passive immunization. These antibodies can activate the classical complement pathway leading to lysis of enveloped virus particles long before the adaptive immune response is activated. Many natural antibodies are directed against the disaccharide galactose α(1,3)-galactose (α-Gal), which is found as a terminal sugar on glycosylated cell surface proteins, and generated in response to production of this sugar by bacteria contained in the human gut.[23] Rejection of xenotransplantated organs is thought to be, in part, the result of natural antibodies circulating in the serum of the recipient binding to αGal antigens expressed on the donor tissue.[24] Immunoglobulin diversity Virtually all microbes can trigger an antibody response. Successful recognition and eradication of many different types of microbes requires diversity among antibodies; their amino acid composition varies allowing them to interact with many different antigens.[25] It has been estimated that humans generate about 10 billion different antibodies, each capable of binding a distinct epitope of an antigen.[26] Although a huge repertoire of different antibodies is generated in a single individual, the number of genes available to make these proteins is limited by the size of the human genome. Several complex genetic mechanisms have evolved that allow vertebrate B cells to generate a diverse pool of antibodies from a relatively small number of antibody genes.[27] Domain variability The hypervariable regions of the heavy chain are shown in red, PDB 1IGT The region (locus) of a chromosome that encodes an antibody is large and contains several distinct genes for each domain of the antibody—the locus containing heavy chain genes (IGH@) is found on chromosome 14, and the loci containing lambda and kappa light chain genes (IGL@ and IGK@) are found on chromosomes 22 and 2 in humans. One of these domains is called the variable domain, which is present in each heavy and light chain of every antibody, but can differ in different antibodies generated from distinct B cells. Differences, between the variable domains, are located on three loops known as hypervariable regions (HV-1, HV-2 and HV-3) or complementarity determining regions (CDR1, CDR2 and CDR3). CDRs are supported within the variable domains by conserved framework regions. The heavy chain locus contains about 65 different variable domain genes that all differ in their CDRs. Combining these genes with an array of genes for other domains of the antibody generates a large cavalry of antibodies with a high degree of variability. This combination is called V(D)J recombination discussed below.[28] V(D)J recombination Simplistic overview of V(D)J recombination of immunoglobulin heavy chains Somatic recombination of immunoglobulins, also known as V(D)J recombination, involves the generation of a unique immunoglobulin variable region. The variable region of each immunoglobulin heavy or light chain is encoded in several pieces—known as gene segments. These segments are called variable (V), diversity (D) and joining (J) segments.[27] V, D and J segments are found in Ig heavy chains, but only V and J segments are found in Ig light chains. Multiple copies of the V, D and J gene segments exist, and are tandemly arranged in the genomes of mammals. In the bone marrow, each developing B cell will assemble an immunoglobulin variable region by randomly selecting and combining one V, one D and one J gene segment (or one V and one J segment in the light chain). As there are multiple copies of each type of gene segment, and different combinations of gene segments can be used to generate each immunoglobulin variable region, this process generates a huge number of antibodies, each with different paratopes, and thus different antigen specificities.[2] After a B cell produces a functional immunoglobulin gene during V(D)J recombination, it cannot express any other variable region (a process known as allelic exclusion) thus each B cell can produce antibodies containing only one kind of variable chain.[3][29] Somatic hypermutation and affinity maturation Following activation with antigen, B cells begin to proliferate rapidly. In these rapidly dividing cells, the genes encoding the variable domains of the heavy and light chains undergo a high rate of point mutation, by a process called somatic hypermutation (SHM). SHM results in approximately one nucleotide change per variable gene, per cell division.[5] As a consequence, any daughter B cells will acquire slight amino acid differences in the variable domains of their antibody chains. This serves to increase the diversity of the antibody pool and impacts the antibody’s antigenbinding affinity.[30] Some point mutations will result in the production of antibodies that have a weaker interaction (low affinity) with their antigen than the original antibody, and some mutations will generate antibodies with a stronger interaction (high affinity).[31] B cells that express high affinity antibodies on their surface will receive a strong survival signal during interactions with other cells, whereas those with low affinity antibodies will not, and will die by apoptosis.[31] Thus, B cells expressing antibodies with a higher affinity for the antigen will outcompete those with weaker affinities for function and survival. The process of generating antibodies with increased binding affinities is called affinity maturation. Affinity maturation occurs in mature B cells after V(D)J recombination, and is dependent on help from helper T cells.[32] Mechanism of class switch recombination that allows isotype switching in activated B cells Class switching Isotype or class switching is a biological process occurring after activation of the B cell, which allows the cell to produce different classes of antibody (IgA, IgE, or IgG). The different classes of antibody, and thus effector functions, are defined by the constant (C) regions of the immunoglobulin heavy chain. Initially, naïve B cells express only cell-surface IgM and IgD with identical antigen binding regions. Each isotype is adapted for a distinct function, therefore, after activation, an antibody with a IgG, IgA, or IgE effector function might be required to effectively eliminate an antigen. Class switching allows different daughter cells from the same activated B cell to produce antibodies of different isotypes. Only the constant region of the antibody heavy chain changes during class switching; the variable regions, and therefore antigen specificity, remain unchanged. Thus the progeny of a single B cell can produce antibodies, all specific for the same antigen, but with the ability to produce the effector function appropriate for each antigenic challenge. Class switching is triggered by cytokines; the isotype generated depends on which cytokines are present in the B cell environment.[33] Class switching occurs in the heavy chain gene locus by a mechanism called class switch recombination (CSR). This mechanism relies on conserved nucleotide motifs, called switch (S) regions, found in DNA upstream of each constant region gene (except in the δ-chain). The DNA strand is broken by the activity of a series of enzymes at two selected S-regions.[34][35] The variable domain exon is rejoined through a process called non-homologous end joining (NHEJ) to the desired constant region (γ, α or ε). This process results in an immunoglobulin gene that encodes an antibody of a different isotype.[36] INTRODUCTION: Antigen (Ant Installer Generator) is a tool to take an Ant build script, combine it with a GUI and wrap it up as an executable jar file. Its primary purpose is to create powerful graphical installers from Ant scripts. ANTIGENS PROPERTIES: Antigens- may possess: Immunogenicity, Antigenicity, Allerogenicity, or Tolerogenicity Immunogenicity – Property that allows a substance to induce a detectable immune response (humoral or cellular) when introduced into an animal. Such substances are termed Immunogens. Antigenicity – Property that allows a substance to combine specifically with antibodies or TcR,whether or not they are immunogenic. Therefore, all immunogens are antigens but not all antigens are immunogens. Allerogenicity- Property that allows a substnace to induce an allergic response. Such substances are termed allergens. Tolerogenicity- Property that allows a substance to induce specific immunologic non-responsiveness in either the humoral or cell-mediated branch. Such substances are termed tolerogens. Haptens – Low-molecular weight compounds including many drugs and antibiotics, are nonimmunogenic but when coupled to immunogenic proteins, the resulting conjugates stimulate the production of antibodies which can bind to the low-molecular weight component. Such molecules are termed haptens. Epitope – The part of an antigen that combines with a specific antibody or T cell receptor. Previous term used was antigenic determinant. Immunogens For the induction of humoral immunity (antibody response), the most potent immunogens are macromolecular proteins or glycoproteins, but polysaccharides, synthetic peptides, and other synthetic polymers such as polyvinylpyrrolidone are immunogenic under appropriate conditions. Pure nucleic acids or lipids are not immunogenic but antibodies which react with them can be induced by immunization with nucleoproteins or lipoproteins. In general, proteins serve as immunogens for T cell-mediated immunity. (Recall that these proteins must be processed into peptides and the peptides must be presented by an APC in association with MHC proteins. Requirements for Immunogenicity The requirements are somewhat dependent upon the experimental conditions (mode of immunization, organism being immunized, sensitivity of detection methods, etc.). However, certain conditions must be met in order for a molecule to be immunogenic: A. Foreignness: [Rabbit albumin not immunogenic in another rabbit but would be immunogenic in a mouse.] B. Molecular Size: [Certain minimum size is required for immunogenicity. The most potent immunogens are macromolecular proteins with molecular weights greater than 100,000. Substances <1000 are not usually immunogenic] C. Chemical Complexity: [Homopolymers consisting of repeating units of a single amino acid are poor immunogens regardless of their size] Co-polymers of 2 or 3 amino acids may be good immunogens. A co-polymer of glutamic acid and lysine must be 30-40,000 to be immunogenic Add tyrosine - reduce size limitation to 10-20,000 Add tyrosine and phenylalanine and reduce to, 4000 -- In general, immunogenicity increases with structural complexity. Aromatic amino acids contribute more to immunogenicity than non-aromatic (ex: tyrosine or phenylalanine). D. Degradability: Macromolecules that cannot be degraded and processed by APCs are poor immunogens. For example, polymers of D-amino acids are not immunogenic. Proteolytic enzymes can only degrade proteins containing L-amino acids. E. Genetic constitution of the Animal: Immune response is under genetic control. Individuals differ in their ability to respond to immunogens. Animal may not have an appropriate Ig, may not have an appropriate TcR, or may not have an appropriate MHC. F. Method of Antigen Administration: Whether an antigen will induce an immune response depends on the dose and the mode of administration. Antigen can be delivered in a variety of ways: ip, sc, iv, im, id, etc. The repsonse will vary depending upon the route chosen. In addition, too little antigen may not stimulate a strong response, whereas too much antigen may stimulate tolerance (specific non-responsiveness). The use of an adjuvant can also enhance the immunogenicity of an antigen. Adjuvants (such as Freunds) prolong the persistence of the antigen in the body, induce a strong inflammatory response which can lead to granuloma formation, and can stimulate lymphocyte proliferation. T cells and B cells exhibit fundamental differences in epitope recognition. B cell epitopes [epitopes recognized by membrane-bound Ig, or secreted Ig] The binding of antigen to Ig involves weak non-covalent interactions so there must be complementarity. Properties of B cell epitopes: 1]Epitopes may be associated with soluble immunogens or particulate immunogens. 2]Epitopes tend to be accessible and on the exposed surface of the immunogen. 3]Epitopes generally contain hydrophilic amino acids 4]Often the epitopes are found where the molecule bends or where there is a high degree of segmental mobility [atomic mobility] 5]The epitope may consist of either sequential or non-sequential amino acids. If non-sequential, the 3D conformation of the epitope if vital. 6] Complex proteins contain multiple overlapping epitopes 7] The size of a B cell epitope is determined by the size of the antigen binding site on the antibody molecule. Conformationally determined epitopes tend to require a larger epitope. Smaller ligands (carbohydrates, peptides, haptens, etc.) tend to fit within a deep concave pocket or crevice. Larger globuluar antigens tend to interact with Ig across a large planar face. Protrusions on the antigen binding site would be complementary with depressions on the epitope and vice versa. This type of interaction is obviously highly dependent upon the 3D conformation of the globular antigen. T cell epitopes [epitopes recognized by membrane-bound TcR only] T cells recognize processed peptides associated with MHC on the surface of APCs (Class II MHC) or altered self cells (Class I MHC). In other words, T cells exhibit MHC RESTRICTED ANTIGEN RECOGNITION CD4+ T cells are restricted to Class II MHC CD8+ T cells are restricted to Class I MHC More recent evidence suggests that a small population of T cells may possess TcRs capable of recognizing lipids or glycolipids. Little is known about this type of recognition and we will restrict our discussion to peptide epitopes. 1]The binding of the TcR to MHC + peptide represents a tri-molecular complex. 2]Only oligomeric peptides serve as epitopes. Epitopes which bind to Class I MHC have an optimal size of 9 amino acids with a range from 8-11. Epitopes which bind to Class II MHC have an optimal size range from 12-25 amino acids. 3) Epitopes are often internal and only exposed by processing within APCs or target cells. 4] Antigen processing is required to generate the peptides that interact specifically with MHC molecules. 5] T cell epitopes must have two binding regions. The region of the peptide which binds to MHC is termed the agretope while the region which binds to the TcR is termed the epitope. 6) Complex proteins may contain multiple, overlapping epitopes. 7 ) Immunodominant T cell epitopes are determined by the set of MHC molecules which are expressed by an individual. Experimentally it has been demonstrated that there is a correlation between the ability of a peptide to bind to a particular MHC molecule and the T cell response to that peptide. MITOGENS Mitogens are agents that are able to induce cell division (mitosis) in a high percentage of T or B cells. This proliferation is described as polyclonal activation (as opposed to clonal expansion following the specific encounter with a conventional immunogen). There are T cell mitogens and B cell mitogens. A number of common mitogens are lectins. Lectins are proteins which bind to specific carbohydrate groups (moieties). They bind to glycoproteins on the surface of the lymphocytes and cause activation. Important...they do not act via conventional TcR-epitope or Ig-epitope interactions. Lectin Examples: Con A - T cell mitogen PHA - T cell mitogen PWM - T and B cell mitogen Another important mitogen which is NOT a lectin is LPS (lipopolysaccharide). This polysaccharide component of the outer membrane of gram - bacteria is also known as endotoxin. LPS is a very potent mitogen for B cells. SUPERANTIGENS Among the most potent T cell mitogens known!! Bind differently to the TcR and MHC so a large # of T cells are activated. In some cases as many as 1/5 T cells may be activated to proliferate and to secrete cytokines. See figure in text for nature of interaction of superantigen + TCR and MHC. Many microbial pathogens (including Streptococcus and Staphylococcus) produce toxins which function as superantigens. The symptoms of staphylococcal food poisoning are due to the massive T cell proliferation and cytokine secretion which occurs in the GALT due to the presence of staphylococcal enterotoxin in food. Toxic shock syndrome and Toxic shock-like syndrome are both due to the action of bacterial superantigens. GENETIC BASIS OF ANTIBODY DIVERSITY OBJECTIVES: When you finish this section, you should be able to: 1. Define the following terms: allelic exclusion, isotype switching, affinity maturation, antibody repertoire, alternative RNA splicing, recombination signal sequence.2. Describe the genes that encode Ig Heavy and Light chains. 3. Describe the sequence of Ig gene rearrangement that occurs during B cell differentiation. 4. Discuss how diversity in antibody specificity is achieved. 5. Discuss the mechanisms of heavy chain class switching. 5. Calculate the number of possible Igs which can be produced from a given number of V, J, D, and C genes. GENETIC BASIS OF ANTIBODY DIVERSITY •Estimates of antibody specificities in an individual range between 106 - 108 . •If 1 gene encoded 1 immunoglobulin of a given specificity, approximately 106 - 108 genes would be required to JUST encode antibodies. •This is impossible because the entire human genome is made up of 3.2 x 109 base pairs. •Average protein = 107 amino acids = 107 x 3 = 3.2 x 102 base pairs •If 1 gene encodes 1 protein, the total # of genes will be equivalent to 3.2 x 109 3.2 x 102 = 1 x 107 genes • However, estimates are that only 31,000 to 35,000 genes in the human genome actually encode proteins! � This number of genes is unable to encode ALL antibody specificities Organization of Immunoglobulin Genes �Numerous V region genes are preceded by Leader or signal sequences (60-90 bp) exons interspersed with introns. �Heavy chain contains V (Variable), D (Diversity), J (Joining) and C (Constant) region gene segments. •V-D-J-C �Light chain contains V, J, and C region gene segments •V-J-C •Constant region genes are sub-divided into exons encoding domains (CH1,CH2, CH3, CH4) Genomic organization of the heavy and light chain gene segments in humans CHARACTERISTICS OF IMMUNOGLOBULIN GENE RE-ARRANGEMENT 1. Involves Allelic Exclusion. – Only one of two parental alleles of Ig is expressed in a B cell. – Either kappa or lambda light chain is expressed by a B cell (light chain isotype exclusion). 2. Ig rearrangement occurs prior to antigen exposure. • A. Heavy chain re-arrangement – Re-arrangement occurs in a precise order: – Heavy chain re-arranges before Light chain. – D-J joining occurs first to form DJ and is followed by V-DJ joining to form VDJ. – Production of μ heavy chain by re-arrangement of one allele inhibits re-arrangement on other allele. � If re-arrangement on first allele is non-productive (due to mutations, deletions or frame shifts that generate stop codons), then re-arrangement on the second allele is stimulated. � Therefore, in any antibody-producing B cell, one allele is productively rearranged and the other is either not re-arranged (in germ line configuration) or is aberrantly re-arranged. 5 B. Light chain re-arrangement i.Kappa chain (κ) rearranges before lambda (λ) chain Vjoining occurs. ii. Productive arrangement on one allele blocks re-arrangement on other allele. iii. If kappa protein is produced, re-arrangement of lambda chain is blocked. Otherwise lambda chain undergoes re-arrangement. GENETIC BASIS OF ANTIBODY DIVERSITY OBJECTIVES: When you finish this section, you should be able to: 1. Define the following terms: allelic exclusion, isotype switching, affinity maturation, antibody repertoire, alternative RNA splicing, recombination signal sequence. 2. Describe the genes that encode Ig Heavy and Light chains. 3. Describe the sequence of Ig gene rearrangement that occurs during B cell differentiation. 4. Discuss how diversity in antibody specificity is achieved. 5. Discuss the mechanisms of heavy chain class switching. 5. Calculate the number of possible Igs which can be produced from a given number of V, J, D, and C genes. GENETIC BASIS OF ANTIBODY DIVERSITY •Estimates of antibody specificities in an individual range between 106 - 108 . •If 1 gene encoded 1 immunoglobulin of a given specificity, approximately 106 108 genes would be required to JUST encode antibodies. •This is impossible because the entire human genome is made up of 3.2 x 109 base pairs. •Average protein = 107 amino acids = 107 x 3 = 3.2 x 102 base pairs •If 1 gene encodes 1 protein, the total # of genes will be equivalent to 3.2 x 109 3.2 x 102 = 1 x 107 genes • However, estimates are that only 31,000 to 35,000 genes in the human genome actually encode proteins! � This number of genes is unable to encode ALL antibody specificities! DILEMMA Since only 31-35 thousand genes in the human genome actually encode proteins, How then is antibody diversity (between 1 million to 100 million Organization of Immunoglobulin Genes Numerous V region genes are preceded by nLeader or signal sequences (60-90 bp) exons interspersed with introns. Heavy chain contains V (Variable), D (Diversity), J (Joining) and C (Constant) region gene segments. • V - D - J - C �Light chain contains V, J, and C region gene segments • V - J - C •Constant region genes are sub-divided into exons encoding domains (CH1,CH2, CH3, CH4) Genomic organization of the heavy and light chain gene segments in humans CHARACTERISTICS OF IMMUNOGLOBULIN GENE RE-ARRANGEMENT 1. Involves Allelic Exclusion. – Only one of two parental alleles of Ig is expressed in a B cell. – Either kappa or lambda light chain is expressed by a B cell (light chain isotype exclusion). 2. Ig rearrangement occurs prior to antigen exposure. • A. Heavy chain re-arrangement – Re-arrangement occurs in a precise order: – Heavy chain re-arranges before Light chain. – D-J joining occurs first to form DJ and is followed by V-DJ joining to form VDJ. – Production of μ heavy chain by re-arrangement of one allele inhibits re-arrangement on other allele. � If re-arrangement on first allele is non-productive (due to mutations, deletions or frame shifts that generate stop codons), then re-arrangement on the second allele is stimulated. � Therefore, in any antibody-producing B cell, one allele is productively rearranged and the other is either not re-arranged (in germ line configuration) or is aberrantly re-arranged. B. Light chain re-arrangement i.Kappa chain (κ) rearranges before lambda (λ) chain V-joining occurs. ii. Productive arrangement on one allele blocks re-arrangement on other allele. iii. If kappa protein is produced, re-arrangement of lambda chain is blocked. Otherwise lambda chain undergoes re-arrangement. MECHANISM OF IMMUNOGLOBULIN RE-ARRANGEMENT � Occurs principally via looping out (excision) of intervening gene sequences followed by ligation of Ig gene segments. � Controlled by recombination signal sequences (RSS) located at joining sites. � Consist of heptamer/nonamer (7/9) sequences interspersed by 12/23 base pair spacers. � Recognized by Recombinases (enzymes with endonuclease and ligase activities). Consists of RAG1,2 proteins (lymphocyte-specific, and nonlymphocytespecific DNA repair proteins (DNA ligase IV, DNAdependent protein kinase (DNA-PK) and Ku, a protein that associates with DNA-PK � Genes encoding recombinases are present in all cell types but are expressed only in lymphoid (B &T) cells. � Recombination activating genes 1 and 2 (RAG-1, RAG-2) have been identified which stimulate Ig gene rearrangement. Have endonuclease activity. MECHANISMS FOR GENERATING ANTIBODY DIVERSITY • Presence of multiple V genes in the germ line. • Combinatorial Diversity - due to potentially different associations of different V, D and J gene segments. • Junctional Diversity • i. Imprecise joining • ii. N/P region (insertional) diversity occurs in VDJ joining (heavy chain) as well as VJ join of light chain. Arises from addition of up to 20 nucleotides by terminal deoxynucleotidyl transferase (TdT). • Somatic Hypermutation • i. Occurs randomly after antigenic stimulation and principally in CDR1, CDR2, CDR3 regions (more frequent in CDR3). Introduces point mutations at a higher rate than for normal mammalian genes. Mutation rate of V genes is 1 base pair change per 103 base pairs/cell division; it is 10-7 in other mammalian genes. • ii. Can give rise to Ig with different (new) antigen specificities leading to high or low affinity Abs. High affinity B cell clones are selectively expanded (Affinity Maturation). • iii. Affinity maturation is associated with isotype switching. • Random Assortment of H and L chains. Mechanisms Contributing to the Generation of Antibody Diversity in Humans Germ line genes H κ λ V segments 65 40 30 J segments 6 5 4 D segments 27 0 0 Combinatorial Joining V x J (x D) 11,000 200 120 H-L chain associations H x κ 2.2 x 106 from 177 H x λ 1.3 x 106 segments EXPRESSION OF DIFFERENT CLASSES AND TYPES OF IMMUNOGLOBULINS •Co-expression of IgM and IgD • Both IgM and IgD are co-expressed on the surface of a mature B lymphocyte. • Occurs by alternative RNA splicing. ISOTYPE SWITCHING Is the conversion of an immunoglobulin from one isotype to another (e.g. IgG to IgE) while retaining the same antigen specificity. �Switching is dependent on antigenic stimulation and is induced by cytokines released by helper T cells and requires engagement of CD40L [e.g. IL-4 triggers switching from IgM to IgE or IgG4 (humans); IFN-γ triggers switching from IgM to IgG2a (mice)]. Cyokines are thought to alter chromatin structure making switch sites more accessible to recombinases for gene transcription. �Involves switch sites located in introns upstream of each CH segment (except Cδ). �Switch sites consist of multiple copies of conserved repeat sequences [(GAGCT)n GGGGGT)] where n can vary from 3-7. �Class switching occurs usually in activated B cells (including memory cells) and not in naïve B cells and involves heavy chain genes. These cells (you will recall) already have rearranged VDJ genes at the DNA level and were producing IgM and IgD. ISOTYPE SWITCHING (Contd.) • If this B cell chooses to class switch to say IgG at the DNA level (by DNA deletion, which is irreversible), then the switch regions of IgM and IgD (recall that they are both controlled by one switch region) join with that of IgG to excise the IgM and IgD constant region gene segments. • When this occurs what you have left is the recombined VDJ gene cluster still separated from the IgG constant region gene segments by intronic DNA. • The switched gene will now be transcribed into primary RNA that undergoes splicing to now bring the VDJ and C regions together to form VDJC. • The take home lesson is that VDJ (or VJ) segments do not join to C region genes at the DNA level whether it is during classical gene re-arrangement or class switching. The joining of VDJ to C to form VDJC occurs only at the RNA level! � Mechanism of switching is unclear. However, class specific recombinases are thought to recognize and bind to switch sites to facilitate recombination. Isotype switching can occur by: A. Switch recombination (Deletion of DNA) -primary mechanism of isotype switching -is irreversible B. Alternative splicing of primary RNA transcript (rare) -Explains co-expression of multiple isotypes by a single B cell. Anti antibodies Anti-nuclear antibodies (ANAs, also known as anti-nuclear factor or ANF) are autoantibodies directed against contents of the cell nucleus. They are present in higher than normal numbers in autoimmune disease. The ANA test measures the pattern and amount of autoantibody which can attack the body's tissues as if they were foreign material. Autoantibodies are present in low titers in the general population, but in about 5% of the population, their concentration is increased, and about half of this 5% have an autoimmune disease. One can check for the presence of ANAs in blood serum by means of a laboratory test. There are also additional tests that allow one to test for individual ANAs. The general ANA test is usually one of two types: indirect immunofluorescence or ELISA. The indirect immunofluoresence is considered to be the more accurate of the two,[citation needed] but the ELISA version is gaining popularity because of its lower cost.[citation needed] [edit] Associated diseases The normal titer of ANA is 1:40 or less. Higher titers are indicative of an autoimmune disease. The presence of ANA is indicative of lupus erythematosus (present in 80-90% of cases), though they also appear in some other auto-immune diseases such as[citation needed] Sjögren's syndrome (60%), rheumatoid arthritis, autoimmune hepatitis, scleroderma and polymyositis & dermatomyositis (30%), and various non-rheumatological conditions associated with tissue damage. ANA are also directed to the nuclear pore complex in primary biliary cirrhosis.[citation needed] Other conditions with high ANA titre include[citation needed] Addison disease, Idiopathic thrombocytopenic purpura (ITP), Hashimoto's, Autoimmune hemolytic anemia, Type I diabetes mellitus, Mixed connective tissue disorder. [edit] Sensitivity The following table list the sensitivity of different types of ANAs for different diseases, in this case what percentage of those with the disease have the ANA. Some ANAs appear in several types of disease, resulting in lower specificity of the test. ANA type Tar Sen get siti anti vity gen SLE Dru Diff Lim Sjö Infl g- use ited gre am ind syst Scl n ma uce emi ero syn tor d c der dro y LE scle ma me my rosi opa s thy All Vari>95 >95 70- 70- 50- 40AN ous 90 90 80 60 As (by indir ect IF) Ant DN 40- i- A 60 dsD NA - - - - Ant Cor 20- i- e 30 Sm pro tein s of snR NPs - - - - Ant Hist 50- >95 i- one 70 hist s one - - - Ant An 30- i- snR 40 U1 NP RN P 15 10 - - Ant Typ i eI Scl- top 70 ois om era se - 28- 10- 70 18 - Ant Cen i- tro cen me tro ric me pro re tein s - 22- 90 26 - SS- RN 30- A Ps 50 (Ro ) - - 70- 10 95 SS- RN 10- B Ps 15 (La) - - 60- 90 Jo- Hist 1 idin etRN A liga se - - - - 25 - = less than 5% sensitivity Unless else specified in boxes, then ref is: [2] About 30% to 40% of people with rheumatoid arthritis have a high ANA titer. UNIT-III INTRODUCTION A substace that can produce a specific immune response when it is introduced in to the tissues of an animal and that can react specifically with specific immune cell is known as an antigen.Antibody is the immunological substance produced against the antigen.The interaction between antigen and antibody is called antigen-antibody reaction.The antibody binds with the antigen form a complex molecule called immune complex or antigen-antibody complex. Strength of antigen-antibody binding The reaction between antigen and antibody is highly specific.Specificity refers to the discriminate abi of a particular antibody to combine with only one type of antigen.The strength of antigen –antibody can be def by the following factors, 1. Binding forces of antigen and antibody 2. Avidity 3. Bonus Effect 4. Cross Effects 1.BINDING FORCES OF ANTIGEN-ANTIBODY The binding between antigen and antibody reaction is due to three factors namely, a , Closeness between antigen and antibody b , Intermolecular forces c , Affinity of antibody A. when the antigen and antibody are closely fit,the strength of binding is great.When they are apart,the binding strength is low. B. The force which operate between two macromolecules,as for example between protein and protein ,also e between antigen and antibody ag-ab reaction.The intermolecular forces which operate between antigen antibody are non-covalent forces and are of 4 types 1.Electrostatic forces 2.Hydrogen bonding 3.Hydrophobic bonding 4.Vander Waals bonding C. Affinity refers to the strength of binding between a particular molecule of antibody and a single antige determinant.Antibodies which bond strongly to the antigenic determinantare called high affinity antibodies.Affin is used to denote the binding capacity of an antibody with a univalent antigen. 2.AVIDITY Avidity refers to the capacity of an antiserum containing various antibodies to combine with the wh antigen that stimulated the production of antibodies.Avidity is used to denote the overall capacity of antibodies combine with multivalent antigen. Avidity is the strength of the bond after the formation of antigen-antibody complex. A multivalent antigen has many types of antigenic determinants.When it is injected into the blood ,e antigenic determinants stimulates the production of a particular antibody.The various antibodies produced by sin antigen combine with the different antigenic determinants of the antigen. 3. BONUS EFFECT The antigen-antibody reaction,the antibody not only binds with the antigen but also the antigens are brid by a single antibody.In some cases two antigens may be bridged by a single antibody.Such binding is weak and Ag-Ab reaction may be reversible in such cases. But when two antigens are bridged by two antibodies,the binding will be strong and the Ag-Ab complex w not dissociate. This phenomenon of giving extra-strength to the antigen-antibody complex by the binding of two antibod to the two antigen molecule is called bonus effect. The bonus effect is highly possible because the antigens are multivalent and there are many types antibodies. Bonus effect increases the binding strength of antigen and antibody molecule. 4. CROSS REACTION An antiserum raised against a given antigen may sometimes react with another closely related antigen.T reaction is called cross reaction and the antigen which produces the cross reaction is called cross reaction antig The cross reaction is due to the presence of one or more identical antigenic determinants on the related antigen. Eg:The antiserum raised against the albumin of hen’s egg cross react with the albumin of duck’s egg. Avidity and affinity In proteins, avidity is a term used to describe the combined strength of multiple bond interactions. Avidity is distinct from affinity, which is a term used to describe the strength of a single bond. As such, avidity is the combined synergistic strength of bond affinities rather than the sum of bonds. It is commonly applied to antibody interactions in which multiple antigen binding sites simultaneously interact with a target. Individually, each binding interaction may be readily broken, however, when many binding interactions are present at the same time, transient unbinding of a single site does not allow the molecule to diffuse away, and binding of that site is likely to be reinstated. The overall effect is synergistic, strong binding of antigen to antibody (e.g. IgM is said to have low affinity but high avidity because it has 10 weak binding sites as opposed to the 2 strong binding sites of IgG, IgE and IgD). If the clustered proteins form a matrix, such as a clathrin-coat, the interaction is described by the term matricity. Antigen The basic principle of any immunochemical technique is that a specific antibody will combine with its specific antigen to give an exclusive antibody-antigen complex An ANTIGEN is defined as “any foreign substance that elicits an immune response (e.g., the production of specific antibody molecules) when introduced into the tissues of a susceptible animal and is capable of combining with the specific antibodies formed”. Antigens are generally of high molecular weight and commonly are proteins or polysaccharides. Polypeptides, lipids, nucleic acids and many other materials can also function as antigens. Immune responses may also be generated against smaller substances, called haptens, if these are chemically coupled to a larger carrier protein, such as bovine serum albumin, keyhole limpet hemocyanin (KLH) or other synthetic matrices. A variety of molecules such as drugs, simple sugars, amino acids, small peptides, phospholipids, or triglycerides may function as haptens. Thus, given enough time, just about any foreign substance will be identified by the immune system and evoke specific antibody production. However, this specific immune response is highly variable and depends much in part on the size, structure and composition of antigens. Antigens that elicit strong immune responses are said to be strongly immunogenic. Antigen-Antibody Interaction The specific association of antigens and antibodies is dependent on hydrogen bonds, hydrophobic interactions, electrostatic forces, and van der Waals forces. These are all bonds of a weak, non-covalent nature, yet some of the associations between antigen and antibody can be quite strong. Like antibodies, antigens can be multivalent, either through multiple copies of the same epitope, or through the presence of multiple epitopes that are recognized by multiple antibodies. Interactions involving multivalency can produce more stabilized complexes, however multivalency can also result in steric difficulties, thus reducing the possibility for binding. All antigen-antibody binding is reversible, however, and follows the basic thermodynamic principles of any reversible bimolecular interaction: where KA is the affinity constant, Ab and Ag are the molar concentrations of unoccupied binding sites on the antibody or antigen respectively, and Ab–Ag is the molar concentration of the antibody-antigen complex. The time taken to reach equilibrium is dependent on the rate of diffusion and the affinity of the antibody for the antigen, and can vary widely. The affinity constant for antibody-antigen binding can span a wide range, extending from below 105 mol–1 to above 1012 mol–1. Affinity constants can be affected by temperature, pH and solvent. Affinity constants can be determined for monoclonal antibodies, but not for polyclonal antibodies, as multiple bondings take place between polyclonal antibodies and their antigens. Quantitative measurements of antibody affinity for antigen can be made by equilibrium dialysis. Repeated equilibrium dialyses with a constant antibody concentration but varying ligand concentration are used to generate Scatchard plots, which give information about affinity valence and possible cross-reactivity. Affinity describes the strength of interaction between antibody and antigen at single antigenic sites. Within each antigenic site, the variable region of the antibody “arm” interacts through weak non-covalent forces with antigen at numerous sites; the more interactions, the stronger the affinity. Avidity is perhaps a more informative measure of the overall stability or strength of the antibody-antigen complex. It is controlled by three major factors: antibody-epitope affinity; the valence of both the antigen and antibody; and the structural arrangement of the interacting parts. Ultimately these factors define the specificity of the antibody, that is, the likelihood that the particular antibody is binding to a precise antigen epitope. Cross-reactivity refers to an antibody or population of antibodies binding to epitopes on other antigens. This can be caused either by low avidity or specificity of the antibody or by multiple distinct antigens having identical or very similar epitopes. Cross-reactivity is sometimes desirable when one wants general binding to a related group of antigens or when attempting cross-species labeling when the antigen epitope sequence is not highly conserved in evolution. Immunofluorescence Definition Immunofluorescence is a laboratory technique to identify specific antibodies or antigens. Antibody identification is usually performed on blood (serum). ELISA Enzyme-linked immunosorbent assay (ELISA), also known as an enzyme immunoassay (EIA), is a biochemical technique used mainly in immunology to detect the presence of an antibody or an antigen in a sample. The ELISA has been used as a diagnostic tool in medicine and plant pathology, as well as a quality control check in various industries. In simple terms, in ELISA, an unknown amount of antigen is affixed to a surface, and then a specific antibody is applied over the surface so that it can bind to the antigen. This antibody is linked to an enzyme, and in the final step a substance is added that the enzyme can convert to some detectable signal. Thus in the case of fluorescence ELISA, when light of the appropriate wavelength is shone upon the sample, any antigen/antibody complexes will fluoresce so that the amount of antigen in the sample can be inferred through the magnitude of the fluorescence. Performing an ELISA involves at least one antibody with specificity for a particular antigen. The sample with an unknown amount of antigen is immobilized on a solid support (usually a polystyrene microtiter plate) either non-specifically (via adsorption to the surface) or specifically (via capture by another antibody specific to the same antigen, in a "sandwich" ELISA). After the antigen is immobilized the detection antibody is added, forming a complex with the antigen. The detection antibody can be covalently linked to an enzyme, or can itself be detected by a secondary antibody which is linked to an enzyme through bioconjugation. Between each step the plate is typically washed with a mild detergent solution to remove any proteins or antibodies that are not specifically bound. After the final wash step the plate is developed by adding an enzymatic substrate to produce a visible signal, which indicates the quantity of antigen in the sample. Traditional ELISA typically involves chromogenic reporters and substrates which produce some kind of observable color change to indicate the presence of antigen or analyte. Newer ELISAlike techniques utilize fluorogenic, electrochemiluminescent, and real-time PCR reporters to create quantifiable signals. These new reporters can have various advantages including higher sensitivities and multiplexing. Technically, newer assays of this type are not strictly ELISAs as they are not "enzyme-linked" but are instead linked to some non-enzymatic reporter. However, given that the general principles in these assays are largely similar, they are often grouped in the same category as ELISAs. Applications ELISA results using S-OIV A neuraminidase antibody at 1 μg/ml to probe the immunogenic and the corresponding seasonal influenza A neuraminidase peptides at 50, 10, 2 and 0 ng/ml. Because the ELISA can be performed to evaluate either the presence of antigen or the presence of antibody in a sample, it is a useful tool for determining serum antibody concentrations (such as with the HIV test or West Nile Virus). It has also found applications in the food industry in detecting potential food allergens such as milk, peanuts, walnuts, almonds, and eggs. ELISA can also be used in toxicology as a rapid presumptive screen for certain classes of drugs. The ELISA was the first screening test widely used for HIV because of its high sensitivity. In an ELISA, a person's serum is diluted 400-fold and applied to a plate to which HIV antigens are attached. If antibodies to HIV are present in the serum, they may bind to these HIV antigens. The plate is then washed to remove all other components of the serum. A specially prepared "secondary antibody" — an antibody that binds to other antibodies — is then applied to the plate, followed by another wash. This secondary antibody is chemically linked in advance to an enzyme. Thus, the plate will contain enzyme in proportion to the amount of secondary antibody bound to the plate. A substrate for the enzyme is applied, and catalysis by the enzyme leads to a change in color or fluorescence. ELISA results are reported as a number; the most controversial aspect of this test is determining the "cut-off" point between a positive and negative result. A cut-off point may be determined by comparing it with a known standard. If an ELISA test is used for drug screening at workplace, a cut-off concentration, 50 ng/mL, for example, is established, and a sample will be prepared which contains the standard concentration of analyte. Unknowns that generate a signal that is stronger than the known sample are "positive". Those that generate weaker signal are "negative." ELISA can also be used to determine the level of antibodies in faecal content...specifically the direct method Types "Indirect" ELISA The steps of "indirect" ELISA follows the mechanism below: A buffered solution of the protein antigen to be tested for is added to each well of a microtiter plate, where it is given time to adhere to the plastic through charge interactions. A solution of non-reacting protein, such as bovine serum albumin, or casein is added to block any plastic surface in the well that remains uncoated by the protein antigen. Then the serum is added, which contains a mixture of the serum donor's antibodies, of unknown concentration, some of which may bind specifically to the test antigen that is coating the well. Afterwards, a secondary antibody is added, which will bind any antibody produced by a member of the donor's species (for example, an antibody produced in a mouse that will bind any rabbit antibody). This secondary antibody often has an enzyme attached to it, which has a negligible effect on the binding properties of the antibody. A substrate for this enzyme is then added. Often, this substrate changes color upon reaction with the enzyme. The color change shows that secondary antibody has bound to primary antibody, which strongly implies that the donor has had an immune reaction to the test antigen. This can be helpful in a clinical setting, and in R&D. The higher the concentration of the primary antibody that was present in the serum, the stronger the color change. Often a spectrometer is used to give quantitative values for color strength. The enzyme acts as an amplifier; even if only few enzyme-linked antibodies remain bound, the enzyme molecules will produce many signal molecules. Within common-sense limitations the enzyme can go on producing color indefinitely, but the more primary antibody is present in the donor serum, the more secondary antibody + enzyme will bind, and the faster color will develop. A major disadvantage of the indirect ELISA is that the method of antigen immobilization is nonspecific; when serum is used as the source of test antigen, all proteins in the sample may stick to the microtiter plate well, so small concentrations of analyte in serum must compete with other serum proteins when binding to the well surface. The sandwich or direct ELISA provides a solution to this problem, by using a "capture" antibody specific for the test antigen to pull it out of the serum's molecular mixture. ELISA may be run in a qualitative or quantitative format. Qualitative results provide a simple positive or negative result (yes or no) for a sample. The cutoff between positive and negative is determined by the analyst and may be statistical. Two or three times the standard deviation (error inherent in a test) is often used to distinguish positive from negative samples. In quantitative ELISA, the optical density (OD) of the sample is compared to a standard curve, which is typically a serial dilution of a known-concentration solution of the target molecule. For example if your test sample returns an OD of 1.0, the point on your standard curve that gave OD = 1.0 must be of the same analyte concentration as your sample. Sandwich ELISA A sandwich ELISA. (1) Plate is coated with a capture antibody; (2) sample is added, and any antigen present binds to capture antibody; (3) enzyme linked capture antibody used as detecting antibody is added, and binds to antigen; (4) substrate is added, and is converted by enzyme to detectable form. A less-common variant of this technique, called "sandwich" ELISA, is used to detect sample antigen. The steps are as follows: 1. 2. 3. 4. 5. Prepare a surface to which a known quantity of capture antibody is bound. Block any non specific binding sites on the surface. Apply the antigen-containing sample to the plate. Wash the plate, so that unbound antigen is removed. Apply enzyme linked primary antibodies as detection antibodies which also bind specifically to the antigen. 6. Wash the plate, so that the unbound antibody-enzyme conjugates are removed. 7. Apply a chemical which is converted by the enzyme into a color or fluorescent or electrochemical signal. 8. Measure the absorbency or fluorescence or electrochemical signal (e.g., current) of the plate wells to determine the presence and quantity of antigen. The image to the right includes the use of a secondary antibody conjugated to an enzyme, though technically this is not necessary if the primary antibody is conjugated to an enzyme. However, use of a secondary-antibody conjugate avoids the expensive process of creating enzyme-linked antibodies for every antigen one might want to detect. By using an enzyme-linked antibody that binds the Fc region of other antibodies, this same enzyme-linked antibody can be used in a variety of situations. Without the first layer of "capture" antibody, any proteins in the sample (including serum proteins) may competitively adsorb to the plate surface, lowering the quantity of antigen immobilized.Use of the purified specific antibody to attach the antigen to the plastic eliminates a need to purify the antigen from complicated mixtures before the measurement, simplifying the assay, and increasing the specificity and the sensitivity of the assay. Competitive ELISA A third use of ELISA is through competitive binding. The steps for this ELISA are somewhat different than the first two examples: 1. Unlabeled antibody is incubated in the presence of its antigen. (Sample) 2. These bound antibody/antigen complexes are then added to an antigen coated well. 3. The plate is washed, so that unbound antibody is removed. (The more antigen in the sample, the less antibody will be able to bind to the antigen in the well, hence "competition.") 4. The secondary antibody, specific to the primary antibody is added. This second antibody is coupled to the enzyme. 5. A substrate is added, and remaining enzymes elicit a chromogenic or fluorescent signal. For competitive ELISA, the higher the sample antigen concentration, the weaker the eventual signal. The major advantage of a competitive ELISA is the ability to use crude or impure samples and still selectively bind any antigen that may be present. (Note that some competitive ELISA kits include enzyme-linked antigen rather than enzymelinked antibody. The labeled antigen competes for primary antibody binding sites with your sample antigen (unlabeled). The more antigen in the sample, the less labeled antigen is retained in the well and the weaker the signal). Commonly the antigen is not first positioned in the well. Reverse ELISA A new technique uses a solid phase made up of an immunosorbent polystyrene rod with 4-12 protruding ogives. The entire device is immersed in a test tube containing the collected sample and the following steps (washing, incubation in conjugate and incubation in chromogenous) are carried out by dipping the ogives in microwells of standard microplates pre-filled with reagents. The advantages of this technique are as follows: 1. The ogives can each be sensitized to a different reagent, allowing the simultaneous detection of different antibodies and different antigens for multi-target assays; 2. The sample volume can be increased to improve the test sensitivity in clinical (saliva, urine), food (bulk milk, pooled eggs) and environmental (water) samples; 3. One ogive is left unsensitized to measure the non-specific reactions of the sample; 4. The use of laboratory supplies for dispensing sample aliquots, washing solution and reagents in microwells is not required, facilitating ready-to-use lab-kits and on-site kits. 5. Enzyme-linked immunosorbent assay (ELISA): ELISA stands for "enzyme-linked immunosorbent assay." This is a rapid immunochemical test that involves an enzyme (a protein that catalyzes a biochemical reaction). It also involves an antibody or antigen (immunologic molecules). 6. ELISA tests are utilized to detect substances that have antigenic properties, primarily proteins (as opposed to small molecules and ions such as glucose and potassium). Some of these include hormones, bacterial antigens and antibodies. 7. There are variations of this test, but the most basic consists of an antibody attached to a solid surface. This antibody has affinity for (will latch on to) the substance of interest, for example, human chorionic gonadotropin (HGC), the commonly measured protein which indicates pregnancy. A mixture of purified HCG linked (coupled) to an enzyme and the test sample (blood, urine, etc) are added to the test system. If no HCG is present in the test sample, then only HCG with linked enzyme will bind. The more HCG which is present in the test sample, the less enzyme linked HCG will bind. The substance the enzyme acts on is then added, and the amount of product measured in some way, such as a change in color of the solution. 8. ELISA tests are generally highly sensitive and specific and compare favorably with radioimmune assay (RIA) tests. They have the added advantages of not needing radioisotopes or a radiation-counting apparatus ELISA Procedure Polyoxyethylene sorbitol monolaurate (Tween 20) was purchased from BioRad Laboratories (Hercules, CA). Skim milk powder was obtained from Difco/Becton Dickinson (Atlanta, GA). Horseradish peroxidase (HRPO)-conjugated mouse anti-human IgG (affinity purified, -chain specific monoclonal clone HP6043) was obtained from Hybridoma Reagent Laboratories (Baldwin, MD). Peroxidase substrate 2,2'-azino-di(3-ethyl-benzthiazoline-6-sulfonate) (ABTS), hydrogen peroxide (H2O2), and peroxidase stop solution were obtained from Kirkegaard & Perry Laboratories (KPL, Gaithersburg, MD). All other laboratory reagents were obtained from Sigma Chemical Co. (St. Louis, MO) unless otherwise specified. Sterile, Type I endotoxin-free water was used for all ELISA procedures. Immulon II-HB flat-bottom 96-well microtiter plates (Thermo Labsystems, Franklin, MA), were coated for 16 hrs at +4°C with 100 µL/well of rPA at a concentration of 2.0 µg/mL in 0.01 M phosphate-buffered saline (PBS), pH 7.4 (Life Technologies, Gaithersburg, MD). Plates were stored at +4°C without blocking and used within 7 days of preparation. Antigen-coated plates were then washed three times (ELX405 microplate washer, BioTek Instruments Inc., Winooski, VT) with PBS containing 0.1% Tween 20 and blotted dry by inversion on clean paper towels. Control and serum antibodies were tested without a separate blocking step. Serum standards and sera for testing were prepared at the appropriate dilutions in PBS containing 5% skim milk and 0.5% Tween 20, pH 7.4. The human standard reference serum and test sera were serially diluted twofold in the plate in the same buffer solution. The minimum dilution of test serum was 1/50. Three positive control sera from three separate donors and one negative control serum were each used at single dilution factors selected to give a range of optical density (OD) values across the standard reference curve. The final volume in all wells was 100 µL. Test and standard sera were incubated in a humidified chamber (covered tray) for 60 min at 37°C, and the plates were then washed three times with PBS containing 0.1% Tween 20. Bound anti-PA IgG was then detected by using HRPO-conjugated mouse anti-human IgG Fc PAN monoclonal HP6043 diluted in PBS containing 5% skim milk and 0.5% Tween 20 (100 µL/well), and plates were incubated in a humidified chamber (covered tray) for 60 min at 37°C. Plates were again washed three times with PBS containing 0.1% Tween 20, and bound conjugate was detected colorimetrically by using ABTS/H2O2 substrate (100 µL/well). Color development was over 30 min (±5 min) and was stopped by addition of 100 µL of Peroxidase Stop Solution (KPL) to all wells of the test plates. OD values were read within 30 min of addition of the stop solution with a MRX Revelation microtiter plate reader (Thermo Labsystems, Franklin, MA) at a wavelength of 410 nm with a 610-nm reference filter. Data were analyzed by using a fourparameter (4-PL) logistic-log curve fitting model with ELISA for Windows software. A calibration factor for the standard reference serum was used to determine the concentration of anti-PA IgG in micrograms per milliliter of serum (µg/mL). Radioimmunoassay Radioimmunoassay (RIA) is a very sensitive technique used to measure concentrations of antigens (for example, hormone levels in the blood) without the need to use a bioassay. Although the RIA technique is extremely sensitive and extremely specific, it requires specialized equipment and is costly. It also requires special precautions, since radioactive substances are used. Therefore, today it has been largely supplanted by the ELISA method, where the antigenantibody reaction is measured using colorimetric signals instead of a radioactive signal. The RAST test (radioallergosorbent test) is an example of radioimmunoassay. It is used to detect the causative allergen for an allergy. Method To perform a radioimmunoassay, a known quantity of an antigen is made radioactive, frequently by labeling it with gamma-radioactive isotopes of iodine attached to tyrosine. This radiolabeled antigen is then mixed with a known amount of antibody for that antigen, and as a result, the two chemically bind to one another. Then, a sample of serum from a patient containing an unknown quantity of that same antigen is added. This causes the unlabeled (or "cold") antigen from the serum to compete with the radiolabeled antigen ("hot") for antibody binding sites. As the concentration of "cold" antigen is increased, more of it binds to the antibody, displacing the radiolabeled variant, and reducing the ratio of antibody-bound radiolabeled antigen to free radiolabeled antigen. The bound antigens are then separated from the unbound ones, and the radioactivity of the free antigen remaining in the supernatant is measured. Using known standards, a binding curve can then be generated which allows the amount of antigen in the patient's serum to be derived. History It was developed by Rosalyn Yalow and Solomon Aaron Berson in the 1950s. In 1977, Rosalyn Sussman Yalow received the Nobel Prize in Medicine for the development of the RIA for insulin: the precise measurement of minute amounts of such a hormone was considered a breakthrough in endocrinology. With this technique, separating bound from unbound antigen is crucial. Initially, the method of separation employed was the use of a second "anti-antibody" directed against the first for precipitation and centrifugation. The use of charcoal suspension for precipitation was extended but replaced later by Drs. Werner and Acebedo at Columbia University for RIA of T3 and T4. An ultramicro RIA for human TSH was published in BBRC (1975) by Radioimmunoassay The technique of radioimmunoassay has revolutionized research and clinical practice in many areas, e.g., blood banking diagnosis of allergies endocrinology The technique was introduced in 1960 by Berson and Yalow as an assay for the concentration of insulin in plasma. It represented the first time that hormone levels in the blood could be detected by an in vitro assay. The Technique A mixture is prepared of o radioactive antigen Because of the ease with which iodine atoms can be introduced into tyrosine residues in a protein, the radioactive isotopes 125I or 131I are often used. o antibodies against that antigen. Known amounts of unlabeled ("cold") antigen are added to samples of the mixture. These compete for the binding sites of the antibodies. At increasing concentrations of unlabeled antigen, an increasing amount of radioactive antigen is displaced from the antibody molecules. The antibody-bound antigen is separated from the free antigen in the supernatant fluid, and the radioactivity of each is measured. From these data, a standard binding curve, like this one shown in red, can be drawn. Radioimmunoassay (RIA) RIA involves the separation of the drug using the specificity of antibody - antigen binding and quantitation using radioactivity. Components of RIA Assay Kit Drug Antibody Labelled Drug General Procedure for Performing a RIA Analysis Mix sample containing drug with fixed quantity of labelled drug and antibody Allow to equilibrate - incubate Separate drug bound to antibody from unbound drug o Charcoal adsorption of antibody (and bound drug) o Antibody - antibody binding precipitates bound drug o Antibody bonded to container Measure radioactivity associated with bound labelled drug o low drug concentration means more bound radioactivity and higher measurement o high drug concentration means less bound radioactivity and lower measurement Determine standard curve o Non-linear plot of radioactivity versus concentration o Logit-log concentration plot is linear A Blank and Three Standard Samples RIA before and after Incubation - Blank and Three Standard Samples Table 3.7.1 Bound and Free Drug Concentrations Tot Bo Fre al un e [Dr d [Dr ug] [Dr ug] ug] 0 6 0 3 4 2 6 3 3 12 2 4 FLOW CYTOMETRY Flow cytometry (abbreviated: FCM) is a technique for counting and examining microscopic particles, such as cells and chromosomes, by suspending them in a stream of fluid and passing them by an electronic detection apparatus. The technology has applications in a number of fields, including molecular biolog y, pathology, immunology, plant biology and marine biology. It is used in diagnose blood cancer and application in research & clinical practice. Light of single wave length is directed onto hydro dynamically focused stream of fluid. These fluorescent light rays scattered because of the presence of suspended particle present in the fluid. These fluorescent particles are picked by a no. of detector, which is connected to the instrument. The instrument used for flow cytometry is flow cytometre. Both ELISA & flow cytometry have application in immunology, clinical, diagnostic fields. ELISA ( Enzyme-Linked Immunosorbent Assay) A 96-well microtiter plate being used for ELISA. Enzyme-linked immunosorbent assay (ELISA), also known as an enzyme immunoassay (EIA), is a biochemical technique used mainly in immunology to detect the presence of an antibody or an antigen in a sample. The ELISA has been used as a diagnostic tool in medicine and plant pathology, as well as a quality control check in various industries. In simple terms, in ELISA, an unknown amount of antigen is affixed to a surface, and then a specific antibody is applied over the surface so that it can bind to the antigen. This antibody is linked to an enzyme, and in the final step a substance is added that the enzyme can convert to some detectable signal. Thus in the case of fluorescence ELISA, when light of the appropriate wavelength is shone upon the sample, any antigen/antibody complexes will fluoresce so that the amount of antigen in the sample can be inferred through the magnitude of the fluorescence. Performing an ELISA involves at least one antibody with specificity for a particular antigen. The sample with an un known amount of antigen is immobilized on a solid support (usually a polystyrene microtiter plate) either non-specifically (via adsorption to the surface) or specifically (via capture by another antibody specific to the same antigen, in a "sandwich" ELISA). After the antigen is immobilized the detection antibody is added, forming a complex with the antigen. The de tection antibody can be covalently linked to an enzyme, or can itself be detected by a secondary antibody which is linked to an enzyme through bioconjugation. Between each step the plate is typically washed with a mild detergent solution to remove any proteins or antibodies that are not specifically bound. After the final wash step the plate is developed by adding an enzymatic substrate to produce a visible signal, which indicates the quantity of antigen in the sample. Traditional ELISA typically involves chromogenic reporters and substrates which produce some kind of observable color change to indicate the presence of antigen or analyte. Newer ELISA -like techniques utilize fluorogenic, electrochemiluminescent, and real-time PCR reporters to create quantifiable signals. These new reporters can have various advantages including higher sensitivities and multiplexing [ 1 ] [ 2 ] . Technically, newer assays of this type are not strictly ELISAs as they are not "enzyme-linked" but are instead linked to some non -enzymatic reporter. However, given that the general principles in these assays are largely similar, they are often grouped in the same category as ELISAs . Applications ELISA results using S-OIV A neuraminidase antibody at 1 μg/ml to probe the immunogenic and the corresponding seasonal influenza A neuraminidase peptides at 50, 10, 2 and 0 ng/ml. Because the ELISA can be performed to evaluate either the presence of antigen or the presence of antibody in a sample, it is a useful tool for determining serum antibody concentrations (such as with the HIV test [ 3 ] or West Nile Virus). It has also found applications in the food industry in detecting potential food allergens such as milk, peanuts, walnuts, almonds, and eggs. [ 4 ] ELISA can also be used in toxicology as a rapid presumptive screen for certain classes of drugs. The ELISA was the first screening test widely used for HIV because of its high sensitivity. In an ELISA, a person' s serum is diluted 400-fold and applied to a plate to which HIV antigens are attached. If antibodies to HIV are present in the serum, they may bind to these HIV antigens. The plate is then washed to remove all other components of the serum. A specially prepared "secondary antibody" — an antibody that binds to other antibodies — is then applied to the plate, followed by another wash. This secondary antibody is chemically linked in advance to an enzyme. Thus, the plate will contain enzyme in proportion to the amount of secondary antibody bound to the plate. A substrate for the enzyme is applied, and catalysis by the enzyme leads to a change in color or fluorescence. ELISA results are reported as a number; the most controversial aspect of this test is determining the "cut-off" point between a positive and negative result. A cut-off point may be determined by comparing it with a known standard. If an ELISA test is used for drug screening at workplace, a cut -off concentration, 50 ng/mL, for example, is established , and a sample will be prepared which contains the standard concentration of analyte. Unknowns that generate a signal that is stronger than the known sample are "positive". Those that generate weaker signal are "negative." ELISA can also be used to determi ne the level of antibodies in faecal content...specifically the direct method History Before the development of the EIA/ELISA, the only option for conducting an immunoassay was radioimmunoassay, a technique using radioactivelylabeled antigens or antibodies. In radioimmunoassa y, the radioactivity provides the signal which indicates whether a specific antigen or antibody is present in the sample. Radioimmunoassay was first described in a paper by Rosalyn Sussman Yalow and Solomon Berson published in 1960 [ 5 ] . Because radioactivity poses a potential health threat, a safer alternative was sought. A suitable alternative to radioimmunoassay would substitute a non-radioactive signal in place of the radioactive signal. When enzymes (such as peroxidase) react with appropriate substrates (such as ABTS or 3,3’,5,5’-Tetramethylbenzidine ), this causes a change in color, which is used as a signal. However, the signal has to be associated with the presence of antibody or antigen, which is why the enzyme has to be linked to an appropriate anti body. This linking process was independently developed by Stratis Avrameas and G.B. Pierce [ 6 ] . Since it is necessary to remove any unbound antibody or antigen by washing, the a ntibody or antigen has to be fixed to the surface of the container, i.e. the immunosorbent has to be prepared. A technique to accomplish this was published by Wide and Jerker Porath in 1966. [ 7 ] In 1971, Peter Perlmann and Eva Engvall at Stockholm University in Sweden, and Anton Schuurs and Bauke van Weemen in The Netherlands, independently published papers which synthesized this knowledge into methods to perform EIA/ELISA. Types "Indirect" ELISA The steps of "indirect" ELISA foll ows the mechanism below: A buffered solution of the protein antigen to be tested for is added to each well of a microtiter plate, where it is given time to adhere to the plastic through charge interactions. A solution of non-reacting protein, such as bovine serum albumin, or casein is added to block any plastic surface in the well that remains uncoated by the protein antigen. Then the serum is added, which contains a mixture of the serum donor's antibodies, of unknown concentration, some of which may bind specifically to the test antigen that is coating the well. Afterwards, a secondary antibody is added, which will bind any antibody produced by a member of the donor's species (for example, an antibody produced in a mouse that will bind any rabbit antibod y). This secondary antibody often has an enzyme attached to it, which has a negligible effect on the binding properties of the antibody. A substrate for this enzyme is then added. Often, this substrate changes color upon reaction with the enzyme. The colo r change shows that secondary antibody has bound to primary antibody, which strongly implies that the donor has had an immune reaction to the test antigen. This can be helpful in a clinical setting, and in R&D. The higher the concentration of the primary antibody that was present in the serum, the stronger the color change. Often a spectrometer is used to give quantitative values for color strength. The enzyme acts as an amplifier; even if only few enzyme -linked antibodies remain bound, the enzyme molecules will produce many signal molecules. Within common -sense limitations the enzyme can go on producing color indefinitely, but the more primary antibody is present in the donor serum, the more secondary antibody + enzyme will bind, and the faster color will develop. A major disadvantage of the indirect ELISA is that the method of antigen immobilization is non -specific; when serum is used as the source of test antigen, all proteins in the sample may stick to the microtiter plate well, so small concentrations of analyte in serum must compete with other serum proteins when binding to the well surface. The sandwich or direct ELISA provides a solution to this problem, by using a "capture" antibody specific for the test a ntigen to pull it out of the serum's molecular mixture. ELISA may be run in a qualitative or quantitative format. Qualitative results provide a simple positive or negative result (yes or no) for a sample. The cutoff between positive and negative is determi ned by the analyst and may be statistical. Two or three times the standard deviation (error inherent in a test) is often used to distinguish positive from negative samples. In quantitative ELISA, the optical density (OD) of the sample is compared to a standard curve, which is typically a serial dilution of a known-concentration solution of the target molecule. For example if your test sample returns an OD of 1.0, the point on your standard curve that gave OD = 1.0 must be of the same analyte concentration a s your sample. Sandwich ELISA A sandwich ELISA. (1) Plate is coated with a capture antibody; (2) sample is added, and any antigen present binds to capture antibody; (3) enzyme linked capture antibody used as detecting antibody is added, and binds to antigen; (4) substrate is added, and is converted by enzyme to detectable form. A less-common variant of this technique, called "sandwich" ELISA, is used to detect sample antigen. The steps are as follows: 1. Prepare a surface to which a known quantity of cap ture antibody is bound. 2. Block any non specific binding sites on the surface. 3. Apply the antigen -containing sample to the plate. 4. Wash the plate, so that unbound antigen is removed. 5. Apply enzyme linked primary antibodies as detection antibodies which also bind specifically to the antigen. 6. Wash the plate, so that the unbound antibody -enzyme conjugates are removed. 7. Apply a chemical which is converted by the enzyme into a color or fluorescent or electrochemical signal. 8. Measure the absorbency or fluorescenc e or electrochemical signal (e.g., current) of the plate wells to determine the presence and quantity of antigen. The image to the right includes the use of a secondary antibody conjugated to an enzyme, though technically this is not necessary if the prim ary antibody is conjugated to an enzyme. However, use of a secondary antibody conjugate avoids the expensive process of creating enzyme -linked antibodies for every antigen one might want to detect. By using an enzyme linked antibody that binds the Fc regio n of other antibodies, this same enzyme-linked antibody can be used in a variety of situations. Without the first layer of "capture" antibody, any proteins in the sample (including serum proteins) may competitively adsorb to the plate surface, lowering the quantity of antigen immobilized.Use of the purified specific antibody to attach the antigen to the plastic eliminates a need to purif y the antigen from complicated mixtures before the measurement, simplif ying the assay, and increasing the specificity and the sensitivity of the assay. Competitive ELISA A third use of ELISA is through competitive binding. The steps for this ELISA are somewhat different than the first two examples: 1. Unlabeled antibody is incubated in the presence of its antigen. (Sample) 2. These bound antibody/antigen complexes are then added to an antigen coated well. 3. The plate is washed, so that unbound antibody is removed. (The more antigen in the sample, the less antibody will be able to bind to the antigen in the well, hence "competiti on.") 4. The secondary antibody , specific to the primary antibody is added. This second antibody is coupled to the enzyme. 5. A substrate is added, and remaining enzymes elicit a chromogenic or fluorescent signal. For competitive ELISA, the higher the sample antigen concentration, the weaker the eventual signal. The major advantage of a competitive ELISA is the ability to use crude or impure samples and still selectively bind any antigen that may be present. (Note that some competitive ELISA kits include enzym e-linked antigen rather than enzyme -linked antibody. The labeled antigen competes for primary antibody binding sites with your sample antigen (unlabeled). The more antigen in the sample, the less labeled antigen is retained in the well and the weaker the signal). Commonly the antigen is not first positioned in the well. Reverse ELISA A new technique uses a solid phase made up of an immunosorbent polystyrene rod with 4 -12 protruding ogives. The entire device is immersed in a test tube containing the collecte d sample and the following steps (washing, incubation in conjugate and incubation in chromogenous) are carried out by dipping the ogives in microwells of standard microplates pre-filled with reagents. The advantages of this technique are as follows: 1. The ogives can each be sensitized to a different reagent, allowing the simultaneous detection of different antibodies and different antigens for multi-target assays; 2. The sample volume can be increased to improve the test sensitivity in clinical (saliva, urine), food (bulk milk, pooled eggs) and environmental (water) samples; 3. One ogive is left unsensitized to measure the non -specific reactions of the sample; 4. The use of laboratory supplies for dispensing sample aliquots, washing solution and reagents in microwel ls is not required, facilitating ready-to-use lab-kits and on-site kits. INTRODUCTION The complement system is a biochemical cascade that helps, or “complements”, the ability of antibodies to clear pathogens from an organism. It is part of the immune system called the innate immune system that is not adaptable and does not change over the course of an individual's lifetime. However, it can be recruited and brought into action by the adaptive immune system. The complement system consists of a number of small proteins found in the blood, generally synthesized by the liver, and normally circulating as inactive precursors (pro-proteins). When stimulated by one of several triggers, proteases in the system cleave specific proteins to release cytokines and initiate an amplifying cascade of further cleavages. The end-result of this activation cascade is massive amplification of the response and activation of the cell-killing membrane attack complex. Over 25 proteins and protein fragments make up the complement system, including serum proteins, serosal proteins, and cell membrane receptors. These proteins are synthesized mainly in the liver, and they account for about 5% of the globulin fraction of blood serum. Three biochemical pathways activate the complement system: the classical complement pathway, the alternative complement pathway, and the mannose-binding lectin pathway. History In the late 19th century, Hans Ernst August Buchner found that blood serum contained a "factor" or "principle" capable of killing bacteria. In 1896, Jules Bordet, a young Belgian scientist in Paris at the Pasteur Institute, demonstrated that this principle had two components: one that maintained this effect after being heated, and one that lost this effect after being heated. The heat-stable component was responsible for the immunity against specific microorganisms, whereas the heat-sensitive (heat-labile) component was responsible for the non-specific antimicrobial activity conferred by all normal serum. This heat-labile component is what we now call "complement." The term "complement" was introduced by Paul Ehrlich in the late 1890s, as part of his larger theory of the immune system. According to this theory, the immune system consists of cells that have specific receptors on their surface to recognize antigens. Upon immunization with an antigen, more of these receptors are formed, and they are then shed from the cells to circulate in the blood. These receptors, which we now call "antibodies," were called by Ehrlich "amboceptors" to emphasize their bifunctional binding capacity: They recognize and bind to a specific antigen, but they also recognize and bind to the heat-labile antimicrobial component of fresh serum. Ehrlich, therefore, named this heat-labile component "complement," because it is something in the blood that "complements" the cells of the immune system. In the early half of the 1930s, a team led by the renowned Irish researcher, Jackie Stanley, stumbled upon the allimportant opsonization-mediated effect of C3b. Building off Ehrlich's work, Stanley's team proved the role of complement in both the innate as well as the cell-mediated immune response. Ehrlich believed that each antigen-specific amboceptor has its own specific complement, whereas Bordet believed that there is only one type of complement. In the early 20th century, this controversy was resolved when it became understood that complement can act in combination with specific antibodies, or on its own in a non-specific way. Functions of the Complement The following are the basic functions of the complement 1. Opsonization- enhancing phagocytosis of antigens 2. Chemotaxis- attracting macrophages and neutrophils 3. Lysis- rupturing membranes of foreign cells 4. Clumping of antigen bearing agents 5. Altering the molecular structure of viruses Lectin pathway (MBL - MASP) The lectin pathway is homologous to the classical pathway, but with the opsonin, mannosebinding lectin (MBL), and ficolins, instead of C1q. This pathway is activated by binding mannose-binding lectin to mannose residues on the pathogen surface, which activates the MBLassociated serine proteases, MASP-1, and MASP-2 (very similar to C1r and C1s, respectively),which can then split C4 into C4a and C4b and C2 into C2a and C2b. C4b and C2a then bind together to form the C3-convertase, as in the classical pathway. Ficolins are homologous to MBL and function via MASP in a similar way. In invertebrates without an adaptive immune system, ficolins are expanded and their binding specificities diversified to compensate for the lack of pathogen-specific recognition molecules. Activation of complements by antigen-associated antibody In the classical pathway, C1 binds with its C1q subunits to Fc fragments (made of CH2 region) of IgG or IgM which has formed a complex with antigens. C4b and C3b are also able to bind to antigen-associated IgG or IgM, to its Fc portion . Such immunoglobulin-mediated binding of the complement may be interpreted as that the complement uses the ability of the immunoglobulin to detect and bind to non-self antigens as its guiding stick. The complement itself is able to bind non-self pathogens after detecting their pathogen-associated molecular patterns (PAMPs). however, utilizing specificity of antibody, complements are able to detect non-self enemies much more specifically. There must be mechanisms that complements bind to Ig but would not focus its function to Ig but to the antigen. Figure 2 shows the classical and the alternative pathways with the late steps of complement activation schematically. Some components have a variety of binding sites. In the classical pathway C4 binds to Ig-associated C1q and C1r2s2 enzyme cleave C4 to C4b and 4a. C4b binds to C1q, antigen-associated Ig (specifically to its Fc portion), and even to the microbe surface. C3b binds to antigen-associated Ig and to the microbe surface. Ability of C3b to bind to antigenassociated Ig would work effectively against antigen-antibody immune complexes to make them soluble. In the figure, C2b refers to the larger of the C2 fragments. Regulation of the complement system The complement system has the potential to be extremely damaging to host tissues, meaning its activation must be tightly regulated. The complement system is regulated by complement control proteins, which are present at a higher concentration in the blood plasma than the complement proteins themselves. Some complement control proteins are present on the membranes of selfcells preventing them from being targeted by complement. One example is CD59, also known as protectin which inhibits C9 polymerisation during the formation of the membrane attack complex. Role in disease It is thought that the complement system might play a role in many diseases with an immune component, such as Barraquer-Simons Syndrome, asthma, lupus erythematosus, glomerulonephritis, various forms of arthritis, autoimmune heart disease, multiple sclerosis, inflammatory bowel disease, and ischemia-reperfusion injuries. The complement system is also becoming increasingly implicated in diseases of the central nervous system such as Alzheimer's disease and other neurodegenerative conditions. Deficiencies of the terminal pathway predispose to both autoimmune disease and infections (particularly Neisseria meningitis, due to the role that the C56789 complex plays in attacking Gram-negative bacteria). Mutations in the complement regulators factor H and membrane cofactor protein have been associated with atypical haemolytic uraemic syndrome. Moreover, a common single nucleotide polymorphism in factor H (Y402H) has been associated with the common eye disease agerelated macular degeneration. Both of these disorders are currently thought to be due to aberrant complement activation on the surface of host cells. Mutations in the C1 inhibitor gene can cause hereditary angioedema, an autoimmune condition resulting from reduced regulation of the complement pathway. Mutations in the MAC components of complement--esp. C8--are often implicated in recurrent Nessaria infection. .Th e Cla ssic al Co mp le me nt Pat hw ay In nat e im mu nit y ref ers to ant ige nno ns pec ific def ens e me cha nis ms tha ta hos t use s im me dia tel y or wit hin sev era l ho urs aft er exp osu re to an ant ige n . Th is is the im mu nit y one is bor n wit h an d is the init ial res po nse by the bo dy to eli mi nat e mi cro bes an d pre ven t inf ecti on. Unl ike ada pti ve im mu nit y, inn ate im mu nit y doe s not rec ogn ize eve ry pos sibl e anti gen . Inst ead , it is des ign ed to rec og niz ea few hig hly con ser ved str uct ure s pre sen t in ma ny diff ere nt mi cro org ani sm s. Th e stru ctu res rec ogn ize d are call ed pat ho gen ass oci ate d mo lec ula r pat ter ns and incl ude LP S fro m the gra mneg ativ e cell wal l, pep tid ogl yca n, lip ote cho ic aci ds fro m the gra mpos itiv e cell wal l, the sug ar ma nno se (co m mo n in mic rob ial gly coli pid s and gly cop rot ein s but rar e in tho se of hu ma ns), bac teri al DN A, Nfor my lme thi oni ne fou nd in bac teri al pro tein s, dou ble stra nde d RN A fro m vir use s, and glu can s fro m fun gal cell wal ls. Mo st bod y def ens e cell s hav e pat ter nrec og niti on rec ept ors for the se co m mo n pat hog enass oci ate d mo lec ula r patt ern s a nd so the re is an im me diat e res pon se aga inst the inv adi ng mic roo rga nis m. Pat hog enass oci ate d mo lec ula r patt ern s can als o be rec ogn ize d by a seri es of sol ubl e patt ern rec ogn itio n rec ept ors in the blo od that fun ctio n as ops oni ns and init iate the co mp lem ent pat hw ays . In all, the inn ate im mu ne sys tem is tho ugh t to rec ogn ize app rox ima tely 103 mo lec ula r patt ern s. All of this wil l be dis cus sed in gre ater det ail in upc om ing sec tio ns. Th e inn ate im mu ne res pon ses inv olv e: p h a g o c y t i c c e l l s ( n e u t r o p h i l s , m o n o c y t e s , a n d m a c r o p h a g e s ) ; c e l l s t h a t r e l e a s e i n f l a m m a t o r y m e d i a t o r s ( b a s o p h i l s , m a s t c e l l s , a n d e o s i n o p h i l s ) ; n a t u r a l k i l l e r c e l l s ( N K c e l l s ) ; a n d m o l e c u l e s s u c h a s c o m p l e m e n t p r o t e i n s , a c u t e p h a s e p r o t e i n s , a n d c y t o k i n e s . Ex am ple s of inn ate im mu nit y incl ude ana to mic al bar rier s, me cha nic al re mo val, bac teri al ant ago nis m, patt ern rec ogn itio n rec ept ors, anti gen non spe cifi c def ens e che mic als, the co mp lem ent pat hw ays , pha goc yto sis, infl am mat ion , and fev er. In the nex t sev eral sec tio ns we wil l loo k at eac h of the se in gre ater det ail. We wil l no w tak ea clo ser loo k at the 3 pat hw ays of the co mp lem ent sys tem . Th e co mp lem ent sys tem ref ers to a seri es of pro tein s circ ulat ing in the blo od and bat hin g the flui ds sur rou ndi ng tiss ues . Th e pro tein s circ ulat e in an ina ctiv e for m, but in res pon se to the rec ogn itio n of mo lec ula r co mp one nts of mic roo rga nis m, the y bec om e seq uen tial ly acti ved , wo rki ng in a cas cad e wh ere in the bin din g of one pro tein pro mo tes the bin din g of the nex t pro tein in the cas cad e. Th ere are 3 co mp lem ent pat hw ays that ma ke up the co mp lem ent sys tem : the cla ssic al co mp le me nt pat hw ay, the lect in pat hw ay, an d the alt ern ati ve co mp le me nt pat hw ay. Th e pat hw ays diff er in the ma nn er in wh ich the y are act iva ted an d ulti ma tel y pro du ce a key enz ym e call ed C3 con ver tas e: We wil l no w tak ea clo ser loo k at the cla ssic al co mp lem ent pat hw ay. Th e Cla ssic al Co mp le me nt Pat hw ay Alt hou gh at lea st 21 diff ere nt ser um pro tein s hav e thu s far bee n ide ntif ied as par t of the cla ssic al co mp lem ent pat hw ay, one can loo k at it as a pat hw ay that is pri ma rily act iva ted by eit her Ig G or Ig M bin din g to an ant ige n and inv olv es 11 ma jor ser um pro tei n co mp one nts . Ig G and Ig M are cla sse s of anti bod y mo lec ule s that wil l be dis cus sed in gre ater det ail in Uni t 3, but as me nti one d pre vio usl y, one of the maj or def ens es aga inst mic rob es is the im mu ne def ens es' pro du cti on of ant ibo dy m ole cul es aga ins t tha t mi cro be. Th e "tip s" of the anti bod y (th e Fa b por tio n hav e sha pes that are co mp lem ent ary to epit ope s por tio ns of mic rob ial pro tein s and gly cop rot ein s fou nd on the sur fac e of the mic rob e. Th e Fc por tio n of Ig G and Ig M can acti vat e the cla ssic al co mp lem ent pat hw ay by ena bli ng the firs t enz ym e in the pat hw ay, C1, to ass em ble. Th e rea ctio ns are as foll ow s: a. Ty pic ally to act iva te the cla ssic al co mp lem ent pat hw ay, Ig G or Ig M is ma de in res pon se to an anti gen . Th e Fa b por tio n of Ig G (2 mo lec ule s) or Ig M (1 mo lec ule ) rea cts wit h epi top es of that anti gen .A pro tein call ed C1 q firs t bin ds to the Fc po rtio n of anti gen bou nd Ig G or Ig M afte r whi ch C1r and C1 s atta ch to for m C1, the firs t enz ym e of the pat hw ay b. Th e acti vat ed C1 no w enz ym atic ally cle ave s C4 int o C4 a and C4 b. Th e C4 b the n bin ds to adj ace nt pro tein s and car boh ydr ate s on the sur fac e of the anti gen and the n bin ds C2. Th e acti vat ed C1 cle ave s C2 int o C2 a and C2 b for mi ng C4 b2 a, the C3 con ver tas e. No w the cla ssic al co mp lem ent pat hw ay is acti vat ed. C3 con ver tas e can no w cle ave hu nd red s of mo lec ule s of C3 int o C3 a an d C3 b. c. So me mo lec ule s of C3 b bin d to C4 b2a , the C3 con ver tas e, to for m C4 b2 a3 b, a C5 con ver tas e that cle ave s C5 int o C5 a and C5 b. d. C5 b bin ds to the sur fac e of the tar get cell and sub seq uen tly bin ds C6, C7, C8, and a nu mb er of mo no me rs of C9 to for m C5 b6 789 n, the Me mb ran e Att ack Co mp lex (M AC ). As me nti one d abo ve, co mp one nts of the co mp lem ent pat hw ays car ry out 6 be nef icia l inn ate def ens e fun cti ons . Th ese incl ude : a. tri gge rin g infl am ma tio n C 5 a i s t h e m o s t p o t e n t c o m p l e m e n t p r o t e i n t r i g g e r i n g i n f l a m m a t i o n . I t c a u s e s m a s t c e l l s t o r e l e a s e v a s o d i l a t o r s s u c h a s h i s t a m i n e s o t h a t b l o o d v e s s e l s b e c o m e m o r e p e r m e a b l e ; i t i n c r e a s e s t h e e x p r e s s i o n o f a d h e s i o n m o l e c u l e s o n l e u k o c y t e s a n d t h e v a s c u l a r e n d o t h e l i u m s o t h a t l e u k o c y t e s c a n s q u e e z e o u t o f t h e b l o o d v e s s e l s a n d e n t e r t h e t i s s u e ( d i a p e d e s i s ) ; i t c a u s e s n e u t r o p h i l s t o r e l e a s e t o x i c o x y g e n r a d i c a l s f o r e x t r a c e l l u l a r k i l l i n g ; a n d i t i n d u c e s f e v e r . T o a l e s s e r e x t e n t C 3 a a n d C 4 a a l s o p r o m o t e i n f l a m m a t i o n . A s w e w i l l s e e l a t e r i n t h i s u n i t , i n f l a m m a t i o n i s a p r o c e s s i n w h i c h b l o o d v e s s e l s d i l a t e a n d b e c o m e m o r e p e r m e a b l e , t h u s e n a b l i n g b o d y d e f e n s e c e l l s a n d d e f e n s e c h e m i c a l s t o l e a v e t h e b l o o d a n d e n t e r t h e t i s s u e s . b. che mo tac tic all y att rac tin g ph ago cyt es to the inf ecti on site C 5 a a l s o f u n c t i o n s a s a c h e m o a t t r a c t a n t f o r p h a g o c y t e s . P h a g o c y t e s w i l l m o v e t o w a r d s i n c r e a s i n g c o n c e n t r a t i o n s o f C 5 a a n d s u b s e q u e n t l y a t t a c h , v i a t h e i r C R 1 r e c e p t o r s t o t h e C 3 b m o l e c u l e s a t t a c h e d t o t h e a n t i g e n . T h i s w i l l b e d i s c u s s e d i n g r e a t e r d e t a i l l a t e r i n t h i s u n i t u n d e r p h a g o c y t o s i s . c. pro mo tin g the att ach me nt of ant ige ns to ph ago cyt es (en ha nce d att ach me nt or ops oni zat ion ) C 3 b a n d t o a l e s s e r e x t e n t , C 4 b c a n f u n c t i o n a s o p s o n i n s , t h a t i s , t h e y c a n a t t a c h a n t i g e n s t o p h a g o c y t e s . O n e p o r t i o n o f t h e C 3 b b i n d s t o p r o t e i n s a n d p o l y s a c c h a r i d e s o n m i c r o b i a l s u r f a c e s ; a n o t h e r p o r t i o n a t t a c h e s t o C R 1 r e c e p t o r s o n p h a g o c y t e s , B l y m p h o c y t e s , a n d d e n d r i t i c c e l l s f o r e n h a n c e d p h a g o c y t o s i s . . A c t u a l l y , C 3 b m o l e c u l e c a n b i n d t o p r e t t y m u c h a n y p r o t e i n o r p o l y s a c c h a r i d e . H u m a n c e l l s , h o w e v e r , p r o d u c e F a c t o r H t h a t b i n d s t o C 3 b a n d a l l o w s F a c t o r I t o i n a c t i v a t e t h e C 3 b . O n t h e o t h e r h a n d , s u b s t a n c e s s u c h a s L P S o n b a c t e r i a l c e l l s f a c i l i t a t e t h e b i n d i n g o f F a c t o r B t o C 3 b a n d t h i s p r o t e c t s t h e C 3 b f r o m i n a c t i v a t i o n b y F a c t o r I . I n t h i s w a y , C 3 b d o e s n o t i n t e r a c t w i t h o u r o w n c e l l s b u t i s a b l e t o i n t e r a c t w i t h m i c r o b i a l c e l l s . C 3 a a n d C 5 a i n c r e a s e t h e e x p r e s s i o n o f C 3 b r e c e p t o r s o n p h a g o c y t e s a n d i n c r e a s e t h e i r m e t a b o l i c a c t i v i t y . d. cau sin g lysi s of gra mneg ati ve bac teri a an d hu ma n cell s dis pla yin g for eig n epi top es ; and C 5 b 6 7 8 9 n , f u n c t i o n s a s a M e m b r a n e A t t a c k C o m p l e x ( M A C ) . T h i s h e l p s t o d e s t r o y g r a m n e g a t i v e b a c t e r i a a s w e l l a s h u m a n c e l l s d i s p l a y i n g f o r e i g n a n t i g e n s ( v i r u s i n f e c t e d c e l l s , t u m o r c e l l s , e t c . ) b y c a u s i n g t h e i r l y s i s ; a n d . I t c a n a l s o d a m a g e t h e e n v e l o p e o f e n v e l o p e d v i r u s e s . e. ser vin g as a sec on d sig nal for act iva tin g nai ve Bly mp hoc yte s ; S o m e C 3 b i s c o n v e r t e d t o C 3 d . C 3 d b i n d s t o C R 2 r e c e p t o r s o n B l y m p h o c y t e s . T h i s s e r v e s a s a s e c o n d s i g n a l f o r t h e a c t i v a t i o n o f B l y m p h o c y t e s w h o s e B c e l l r e c e p t o r s h a v e j u s t i n t e r a c t e d w i t h t h e i r c o r r e s p o n d i n g a n t i g e n . f. re mo vin g har mf ul im mu ne co mp lex es fro m the bo dy C 3 b a n d t o a l e s s e r e x t e n t , C 4 b h e l p t o r e m o v e h a r m f u l i m m u n e c o m p l e x e s f r o m t h e b o d y . T h e C 3 b a n d C 4 b a t t a c h t h e i m m u n e c o m p l e x e s t o C R 1 r e c e p t o r s o n e r y t h r o c y t e s . T h e e r y t h r o c y t e s t h e n d e l i v e r t h e c o m p l e x e s t o f i x e d m a c r o p h a g e s w i t h i n t h e s p l e e n a n d l i v e r f o r d e s t r u c t i o n . I m m u n e c o m p l e x e s c a n l e a d t o a h a r m f u l T y p e I I I h y p e r s e n s i t i v i t y , a s w i l l b e d i s c u s s e d l a t e r i n U n i t 3 u n d e r H y p e r s e n s i t i v i t i e s THE CLASSICAL PATHWAY: The classical pathway of the complement system is a major effector of the humoral branch of the human immune response. The trigger for the classical pathway is either IgG or IgM antibody bound to antigen. Binding of antibody to antigen exposes a site on the antibody which is a binding site for the first complement component, C1. C1 is a macromolecular complex made up of the molecules C1q, C1r, and C1s. By itself, C1q is a hexameric molecule comprised of "stalks" and "knobs". The protruding knobs of the C1q molecule bind to exposed sites on antigen-bound antibody molecules. Pairs of C1r and C1s molecules associate with one another to make a figure-8 shape. This figure-8 fits over the knobs of the C1q molecule to make a complete, intact C1 molecule When the intact macromolecular C1 binds to the exposed regions of at least two antigen-bound antibodies, the C1r and C1s subunits are activated. Activated C1s is responsible for the cleavage of the next two involved complement components, C4 and C2. (Remember, the numbers indicate the order in which the components were discovered, not the order in which they activate in the cascade.) C4 is cleaved into two fragments. The larger C4b molecule attaches to the target membrane nearby while the small C4a molecule floats away. An exposed site on deposited C4b is available to interact with the next complement component, C2. Again, activated C1s cleaves the C2 molecule into two pieces. In this case, the fragment that remains is C2a. The smaller C2b fragment floats away. What remains bound to the membrane is C4b2a, also known as the C3 convertase because its role is to convert the next complement component, C3, into its active form. The C3 convertase of the classical pathway splits C3 into two fragments, C3a and C3b. The convertase has the ability to cleave multiple C3 molecules, forming hundreds of C3a and C3b fragments. The C3a fragments float away and have a role in inducing an inflammatory response (more on this later). Of critical importance, some of the C3b binds to the C4b2a to form C4b2a3b - a.k.a. the C5 convertase. The C5 convertase, much like the C3 convertase before it, catalyzes the cleavage of hundreds to thousands of C5 complement component into C5a and C5b before it reverts to inactivity. C5a floats away and contributes to inflammation while the C5b fragment binds to the antigen surface. This binding of C5b is the initial step in the formation of the membrane attack complex (MAC). THE MEMBRANE ATTACK COMPLEX: The membrane-bound complement component C5b is bound by the next complement molecule, C6. The resulting bimolecular complex next binds C7 and then C8. The C5b-8 complex acts as a receptor for a variable number of membrane-disrupting C9 molecules. The resultant C5b-8 complex and poly-C9 is given the name "membrane attack complex." The MAC creates a transmembrane pore leading to the lysis of the target cell. CONCLUSION The alternative complement pathway does not require antibody for its activation. Rather, a variety of antigens such as bacterial lipopolysaccharide and components of viruses and other pathogens have the ability to activate this pathway. It is thought to have evolved earlier than the classical pathway, which depends on the relatively recently evolved antibody molecule. Like the classical pathway, the alternative pathway produces both a C3 and a C5 convertase which leads to the production of C5b and then to the formation of the MAC. The specific molecular players and the path followed along the way are, however, different. The complement component C3 is spontaneously cleaved at low levels. This means that there are C3a and C3b fragments freely floating in serum. The C3b component can attach to a number of different surfaces, both foreign and host cells alike. C3b is quickly inactivated by the sialic acid found on most mammalian cell surfaces. Microbes, most of which lack sialic acid, are stable sites for C3b deposition. (Sialic acid inactivation of C3b is one type of complement evasion strategy utilized by certain pathogens, discussed below.) Membrane-bound C3b fragments are bound by Factor B which is, in turn, cleaved by Factor D. The fragment Ba floats away, while Bb stays associated with C3b. The resulting C3bBb molecule is the alternative pathway C3 convertase. The C3 convertase of the alternative pathway is, however, not particularly stable. In order to effectively split a relevant number of C3 molecules, the C3 convertase requires the stabilization of another molecule, properdin (P), which binds to the C3bBb complex and extends the half-life of its activity. Hybridoma technology Hybridoma technology is a technology of forming hybrid cell lines (called hybridomas) by fusing a specific antibody-producing B cell with a myeloma (B cell cancer) cell that is selected for its ability to grow in tissue culture and for an absence of antibody chain synthesis. The antibodies produced by the hybridoma are all of a single specificity and are therefore monoclonal antibodies (in contrast to polyclonal antibodies). The production of monoclonal antibodies was invented by Cesar Milstein, Georges J. F. Köhler and Niels Kaj Jerne in 1975. C o nt en ts [hid e] 1 M e t h o d 2 A p p l i c a t i o n s o 2 . 1 I n d i a g n o s t i c h i s t o p a t h o l o g y 3 S e e a l s o 4 R e f e r e n c e s 5 E x t e r n a l l i n k s [edit] Method (1) Immunisation of a mouse (2) Isolation of B cells from the spleen (3) Cultivation of myeloma cells (4) Fusion of myeloma and B cells (5) Separation of cell lines (6) Screening of suitable cell lines (7) in vitro (a) or in vivo (b) multiplication (8) Harvesting Laboratory animals (mammals, e.g. mice) are first exposed to an antigen to which we are interested in isolating an antibody against. Usually this is done by a series of injections of the antigen in question, over the course of several weeks. Once splenocytes are isolated from the mammal's spleen, the B cells are fused with immortalized myeloma cells. The myeloma cells are selected beforehand to ensure they are not secreting antibody themselves and that they lack the hypoxanthine-guanine phosphoribosyltransferase (HGPRT) gene, making them sensitive to the HAT medium (see below). The fusion is accomplished using polyethylene glycol or the Sendai virus. It is performed by making the cell membranes more permeable.[clarification needed] Fused cells are incubated in HAT medium (hypoxanthine-aminopterin-thymidine medium) for roughly 10 to 14 days. Aminopterin blocks the pathway that allows for nucleotide synthesis. Hence, unfused myeloma cells die, as they cannot produce nucleotides by the de novo or salvage pathways because they lack HGPRT. Removal of the unfused myeloma cells is necessary because they have the potential to outgrow other cells, especially weakly established hybridomas. Unfused B cells die as they have a short life span. In this way, only the B cellmyeloma hybrids survive, since the HGPRT gene coming from the B cells is functional. These cells produce antibodies (a property of B cells) and are immortal (a property of myeloma cells). The incubated medium is then diluted into multi-well plates to such an extent that each well contains only one cell. Since the antibodies in a well are produced by the same B cell, they will be directed towards the same epitope, and are thus monoclonal antibodies. The next stage is a rapid primary screening process, which identifies and selects only those hybridomas that produce antibodies of appropriate specificity. The hybridoma culture supernatant, secondary enzyme labeled conjugate, and chromogenic substrate, are then incubated, and the formation of a colored product indicates a positive hybridoma. Alternatively, immunocytochemical screening can also be used.[1] The B cell that produces the desired antibodies can be cloned to produce many identical daughter clones. Supplemental media containing interleukin-6 (such as briclone) are essential for this step. Once a hybridoma colony is established, it will continually grow in culture medium like RPMI1640 (with antibiotics and fetal bovine serum) and produce antibodies.[1] Multiwell plates are used initially to grow the hybridomas, and after selection, are changed to larger tissue culture flasks. This maintains the well-being of the hybridomas and provides enough cells for cryopreservation and supernatant for subsequent investigations. The culture supernatant can yield 1 to 60 µg/ml of monoclonal antibody, which is maintained at 20 °C or lower until required.[1] By using culture supernatant or a purified immunoglobulin preparation, further analysis of a potential monoclonal antibody producing hybridoma can be made in terms of reactivity, specificity, and cross-reactivity.[1] Applications This section may need to be wikified to meet Wikipedia's quality standards. Please help by adding relevant internal links, or by improving the section's layout. (January 2010) It has bee n sug ges ted tha t this arti cle or sec tion be me rge d into Mo noc lon al anti bod ies. (Dis cus s) The use of monoclonal antibodies is numerous and includes the prevention, diagnosis, and treatment of disease. For example, monoclonal antibodies can distinguish subsets of B cells and T cells, which is helpful in identifying different types of leukaemias. In diagnostic histopathology With the help of monoclonal antibodies, tissues and organs can be classified based on their expression of certain defined markers, which reflect tissue or cellular genesis. Prostate specific antigen, placental alkaline phosphatase, human chorionic gonadotrophin, α-fetoprotein and others are organ-associated antigens and the production of monoclonal antibodies against these antigens helps in determining the nature of a primary tumor.[1] Monoclonal antibodies are especially useful in distinguishing morphologically similar lesions, like mesothelioma and adenocarcinoma, and in the determination of the organ or tissue origin of undifferentiated metastases. Selected monoclonal antibodies help in the detection of occult metastases by immuno-cytological analysis of bone marrow, other tissue aspirates, as well as lymph nodes and other tissues.[1] One study[2] performed a sensitive immuno-histochemical assay on bone marrow aspirates of 20 patients with localized prostate cancer. Three monoclonal antibodies (T16, C26, and AE-1), capable of recognizing membrane and cytoskeletal antigens expressed by epithelial cells to detect tumour cells, were used in the assay. Bone marrow aspirates of 22% of patients with localized prostate cancer (stage B, 0/5; Stage C, 2/4), and 36% patients with metastatic prostate cancer (Stage D1, 0/7 patients; Stage D2, 4/4 patients) had antigen-positive cells in their bone marrow. It was concluded that immuno-histochemical staining of bone marrow aspirates are very useful to detect occult bone marrow metastases in patients with apparently localized prostate cancer. Although immuno-cytochemistry using tumor-associated monoclonal antibodies has led to an improved ability to detect occult breast cancer cells in bone marrow aspirates and peripheral blood, further development of this method is necessary before it can be used routinely.[3] One major drawback of immuno-cytochemistry is that only tumor-associated and not tumor-specific monoclonal antibodies are used, and as a result, some cross-reaction with normal cells can occur.[4] The detection of small quantities of invasive or metastatic cells by normal histopathological staining with haematoxylin and eosin is not always sensitive. The use of monoclonal antibodies increases the sensitivity to a large extent. For example, the use of monoclonal antibodies to cytokeratin in the investigation of the sentinel axillary lymph node for metastatic breast cancer increases nodal positivity by up to 10%.[1] In order to effectively stage breast cancer and assess the efficacy of purging regimens prior to autologous stem cell infusion, it is important to detect even small quantities of breast cancer cells. Immuno-histochemical methods are ideal for this purpose because they are simple, sensitive, and quite specific. Franklin et al.[5] performed a sensitive immuno-cytochemical assay by using a combination of four monoclonal antibodies (260F9, 520C9, 317G5 and BrE-3) against tumor cell surface glycoproteins to identify breast tumour cells in bone marrow and peripheral blood. They concluded from the results that immuno-cytochemical staining of bone marrow and peripheral blood is a sensitive and simple way to detect and quantify breast cancer cells. One of the main reasons for metastatic relapse in patients with solid tumours is the early dissemination of malignant cells. The use of monoclonal antibodies (mAbs) specific for cytokeratins can identify disseminated individual epithelial tumor cells in the bone marrow. One study[6] reports on having developed an immuno-cytochemical procedure for simultaneous labeling of cytokeratin component no. 18 (CK18) and prostate specific antigen (PSA). This would help in the further characterization of disseminated individual epithelial tumor cells in patients with prostate cancer. The twelve control aspirates from patients with benign prostatic hypertrophy showed negative staining, which further supports the specificity of CK18 in detecting epithelial tumour cells in bone marrow. In most cases of malignant disease complicated by effusion, neoplastic cells can be easily recognized. However, in some cases, malignant cells are not so easily seen or their presence is doubtful to call it a positive report. The use of immuno-cytochemical techniques increases diagnostic accuracy in these cases. Ghosh, Mason and Spriggs[7] analysed 53 samples of pleural or peritoneal fluid from 41 patients with malignant disease. Conventional cytological examination had not revealed any neoplastic cells. Three monoclonal antibodies (anti-CEA, Ca 1 and HMFG-2) were used to search for malignant cells. Immunocytochemical labelling was performed on unstained smears, which had been stored at -20°C up to 18 months. Twelve of the forty-one cases in which immuno-cytochemical staining was performed, revealed malignant cells. The result represented an increase in diagnostic accuracy of approximately 20%. The study concluded that in patients with suspected malignant disease, immuno-cytochemical labeling should be used routinely in the examination of cytologically negative samples and has important implications with respect to patient management. The use of immuno-cytochemical techniques can help to avoid performing procedures, which are painful, uncomfortable and expensive to the patient. It can also help to speed up the start of appropriate treatment. Another application of immuno-cytochemical staining is for the detection of two antigens in the same smear. Double staining with light chain antibodies and with T and B cell markers can indicate the neoplastic origin of a lymphoma.[8] One study has reported the isolation of a hybridoma cell line (clone 1E10), which produces a monoclonal antibody (IgM, k isotype). This monoclonal antibody shows specific immunocytochemical staining of nucleoli.[9] Tissues and tumours can be classified based on their expression of certain markers, with the help of monoclonal antibodies. They help in distinguishing morphologically similar lesions and in determining the organ or tissue origin of undifferentiated metastases. Immuno-cytological analysis of bone marrow, tissue aspirates, lymph nodes etc. with selected monoclonal antibodies help in the detection of occult metastases. Monoclonal antibodies increase the sensitivity in detecting even small quantities of invasive or metastatic cells. Monoclonal antibodies (mAbs) specific for cytokeratins can detect disseminated individual epithelial tumour cells in the bone marrow. Immuno-cytochemical staining can also detect the presence of two antigens in the same smear. UNIT - IV MHC antigens - types and functions AUTOIMMUNITY . Autoimmunity is the failure of an organism to recognize its own constituent parts as self, which allows an immune response against its own cells and tissues. Any disease that results from such an aberrant immune response is termed an autoimmune disease . Prominent examples include Coeliac disease, diabetes mellitus type 1 (IDDM), systemic lupus erythematosus (SLE), Sjögren's syndrome, Churg-Strauss Syndrome , Hashimoto's thyroiditis , Graves' disease, idiopathic thrombocytopenic purpura, and rheumatoid arthritis (RA). See List of autoimmune di seases. The misconception that an individual's immune system is totally incapable of recognizing self antigens is not new. Paul Ehrlich, at the beginning of the twentieth century, proposed the concept of horror autotoxicus , wherein a 'normal' body does not mount an immune response against its own tissues. Thus, any autoimmune response was perceived to be abnormal and postulated to be connected with human disease. Now, it is accepted that autoimmune responses are an integral part of vertebrate immune systems (sometimes termed 'natural autoimmunity'), normally prevented from causing disease by the phenomenon of immunological tolerance to self-antigens. Autoimmunity should not be confused with alloimmunity. Low-level autoimmunity While a high level of autoimmunity is unhealthy, a low level of autoimmunity may actually be beneficial. First, low -level autoimmunity might aid in the recognition of neoplastic cells by CD8+ T cells, and thus reduce the incidence of cancer. Second, autoimmunity may have a role in allowing a rapid immune response in the early stages of an infection when the availability of foreign antigens limits the response (i.e., when there are few pathogens present). In their study, Stefanova et al. (2002) injected an anti -MHC Class II antibody into mice expressing a single type of MHC Class II molecule (H 2 b ) to temporarily prevent CD4+ T cell -MHC interaction. Naive CD4+ T cells (those that have not encountered any antigens before) recovered from these mice 36 hours post -anti-MHC administration showed decreased responsiveness to the antigen pigeon cytochrome C peptide, as determined by Zap-70 phosphorylation, proliferation, and Interleukin-2 production. Thus Stefanova et al. (2002) d emonstrated that self -MHC recognition (which, if too strong may contribute to autoimmune dise ase) maintains the responsiveness of CD4+ T cells when foreign antigens are absent. [ 1 ] This idea of autoimmunity is conceptually similar to play -fighting. The playfighting of young cubs (TCR and self -MHC) may result in a few scratches or scars (low-level-autoimmunity), but is beneficial in the long -term as it primes the young cub for proper fights in the future. Immunological tolerance Pioneering work by Noel Rose and Witebsky in New York, and Roitt and Doniach at University College London provided clear evidence that, at least in terms of antibody-producing B lymphocytes, diseases such as rheumatoid arthritis and thyrotoxicosis are associated with of loss of immunological tolerance , which is the ability of an individual to ignore 'self', while reacting to 'non -self'. This breakage leads to the immune system's mounting an effective and specific immune response against self determinants. The exact genesis of immunological tolerance is still elusive, but several theories have been proposed since the mid -twentieth century to explain its origin. Three hypotheses have gained widespread attention among immuno logists: Clonal Deletion theory, proposed by Burnet, according to which self-reactive lymphoid cells are destroyed during the development of the immune system in an individual. For their work Frank M. Burnet and Peter B. Medawar were awarded the 1960 Nobel Prize in Physiology or Medicine "for discovery of acquired immunological tolerance". Clonal Anergy theory , proposed by Nossal, in which self -reactive Tor B-cells become inactivated in the normal individual and cannot amplify the immune response. [ 2 ] Idiotype Network theory , proposed by Jerne, wherein a network of antibodies capable of neutralizing self -reactive antibodies exists naturally within the body. [ 3 ] In addition, two other theories are under intense investigation: The so-called "Clonal Ignorance" theory, according to which host immune responses are directed to ignore self -antigens [ 4 ] The "Suppressor population" or " Regulatory T cell " theories, wherein regulatory T-lymphocytes (commonly CD4 + FoxP3 + cells, among others) function to prevent, downregulate, or limit autoaggressive immune responses cdimmune System. Tolerance can also be differentiated into 'Central' and 'Peripheral' tolerance, on whether or not the above -stated checking mechanisms operate in the central lymphoid organs (Thymus and Bone Marrow) or the peripheral lymphoid organs (lymph node, spleen, etc., where self -reactive B-cells may be destroyed). It must be emphasised that these theories are not mutually exclusive, and evidence has been mounting suggesting that all of these mechanisms may actively contribute to vertebrate immunological tolerance. A puzzling feature of the documented loss of tolerance seen in spontaneous human autoimmunity is that it is almost entirely restricted to the autoantibody responses produced by B lymphocytes. Loss of tolerance by T cells has been extremely hard to demonstrate, and where there is evidence for an abnormal T cell response it is usually not t o the antigen recognised by autoantibodies. Thus, in rheumatoid arthritis there are autoantibodies to IgG Fc but apparently no corresponding T cell response. In systemic lupus there are autoantibodies to DNA, which cannot evoke a T cell response, and limited evidence for T cell responses implicates nucleoprotein antigens. In Celiac disease there are autoantibodies to tissue transglutaminase but the T cell response is to the foreign protein gliadin. This disparity has led to the idea that human autoimmune di sease is in most cases (with probable exceptions including type I diabetes) based on a loss of B cell tolerance which makes use of normal T cell responses to foreign antigens in a variety of aberrant ways [ 5 ] . Genetic Factors Certain individuals are genetically susceptible to developing autoimmune diseases. This susceptibility is associated with multiple genes plus other risk factors. Genetically-predisposed individuals d o not always develop autoimmune diseases. Three main sets of genes are suspected in many autoimmune diseases. These genes are related to: Immunoglobulins T-cell receptors The major histocompatibility complexes (MHC). The first two, which are involved in the recognition of antigens, are inherently variable and susceptible to recombination. These variations enable the immune system to respond to a very wide variety of invaders, but may also give rise to lymphocytes capable of self-reactivity. Scientists such as H. McDevitt, G. also provided strong evidence to allotypes are strongly correlated Nepom, J. Bell and J. Todd have suggest that certain MHC class II with HLA DR2 is strongly positively correlated with Systemic Lupus Erythematosus, narcolepsy [ 6 ] and multiple sclerosis, and negatively correlated with DM Type 1. HLA DR3 is correlated strongly with Sjögren's syndrome , myasthenia gravis, SLE, and DM Type 1. HLA DR4 is correlated with the genesis of rheumatoid arthritis, Type 1 diabetes mellitus, and pemphigus vulgaris. Fewer correlations exist with MHC class I molecules. The most notable and consistent is the association between HLA B27 and ankylosing spondylitis. Correlations may exist between polymorphisms within class II MHC promoters and autoimmune disease. The contributions of genes outside the MHC compl ex remain the subject of research, in animal models of disease (Linda Wicker's extensive genetic studies of diabetes in the NOD mouse), and in patients (Brian Kotzin's linkage analysis of susceptibility to SLE). Sex M 2/ ult 1 [ 7 M 2/ ipl ] [ 7 ya 1 e ] st scl he er ni osi a s gr (M av S) is S9 y/ Rh 5/ s1 eu 2 [ [7 t m ] 7 e at ] m oi i d c ar l th u rit p is u s e r y t h e m a t o s u s ( S L E ) A person's sex also seems to have some role in the development of autoimmunity, classif ying most autoimmune diseases as sex-related diseases. Nearly 75% [ 7 ] of the more than 23.5 million Americans who suffer from autoimmune disease are women, although it is less -frequently acknowledged that millions of men also suffer from these disea ses. According to the American Autoimmune Related Diseases Association (AARDA), autoimmune diseases that develop in men tend to be more severe. A few autoimmune diseases that men are just as or more likely to develop as women, include: ankylosing spondylitis, type 1 diabetes mellitus, Wegener's granulomatosis , Crohn's disease and psoriasis. The reasons for the sex role in autoimmunity are unclear. Women appear to generally mount larger inflammatory responses than men when their immune systems are triggered, increasing the risk of autoimmu nity. [ 7 ] Involvement of sex steroids is indicated by that many autoimmune disease s tend to fluctuate in accordance with hormonal changes, for example, during pregnancy, in the menstrual cycle, or when using oral contraception. [ 7 ] A history of pregnancy also appears to leave a persistent increased risk for autoimmune disease. [ 7 ] It has been suggested that the slight exchange of cells between mothers and their children during pregnancy may induce autoimmunity. [ 8 ] This would tip the gender balance in the direction of the female. Another theory suggests the fema le high tendency to get autoimmunity is due to an imbalanced X chromosome inactivation . [ 9 ] The X-inactivation skew theory, proposed by Princeton University's Jeff Stewart, has recently been confirmed experimentally in scleroderma and autoimmune thyroiditis. [ 1 0 ] Other complex X -linked genetic susceptibility mechanisms are proposed and under investigation. [ 7 ] Environmental Factors An interesting inverse relationship exists between infectious diseases and autoimmune diseases. In areas where multiple infectious diseases are endemic, autoimmune diseases are quite rarely seen. The reverse, to some extent, seems to hold true. The hygiene hypothesis attributes these correlations to the immune manipulating strategies of pathogens. Whilst such an observation has been variously termed as spurious and ineff ective, according to some studies, parasite infection is associated with reduced activity of autoimmune disease. [ 1 1 ] [ 1 2 ] [ 1 3 ] The putative mechanism is that the parasite attenuates the host immune response in order to protect itself. This may pro vide a serendipitous benefit to a host that also suffers from autoimmune disease. The details of parasite immune modulation are not yet known, but may include secretion of anti inflammatory agents or interference with the host immune signaling. A paradoxical observation has been the strong association of certain microbial organisms with autoimmune diseases. For example, Klebsiella pneumoniae and coxsackievirus B have been strongly correlated with ankylosing spondylitis and diabetes mellitus type 1 , respectively. This has been explained by the tendency of the infecting organism to produce superantigens that are capable of polyclonal activation of B-lymphoc ytes, and production of large amounts of antibodies of varying specificities, some of which may be self-reactive (see below). Certain chemical agents and drugs can also be associated with the genesis of autoimmune conditions, or conditions that simulate autoimmune diseases. The most striking of these is the drug-induced lupus erythematosus. Usually, withdrawal of the offending drug cures the symptoms in a patient. Cigarette smoking is now established as a major risk factor for both incidence and severity of rheumatoid arthritis. [ c i t a t i o n n e e d e d ] This may relate to abnormal citrullination of proteins, since the effects of smoking correlate with the presence of antibodies to citrullinated peptides. [ c i t a t i o n needed] Pathogenesis of autoimmunity Several mechanisms are thought to be operative in the pathogenesis of autoimmune diseases, against a backdrop of genetic predisposition and environmental modulation. It is beyond the scope of this article to discuss each of these mechanisms exhaustively, but a summary of some of the important mechanisms have been described: T-Cell Bypass - A normal immune system requires the activation of B-cells by T-cells before the former can produce antibodi es in large quantities. This requirement of a T -cell can be bypassed in rare instances, such as infection by organisms producing super-antigens, which are capable of initiating polyclonal activation of B -cells, or even of T-cells, by directly binding to the β -subunit of T-cell receptors in a non -specific fashion. T-Cell-B-Cell discordance - A normal immune response is assumed to involve B and T cell responses to the same antige n, even if we know that B cells and T cells recognise very different things: conformations on the surface of a molecule for B cells and pre processed peptide fragments of proteins for T cells. However, there is nothing as far as we know that requires this. All that is required is that a B cell recognising antigen X endocytoses and processes a protein Y (normally =X) and presents it to a T cell. Roosnek and Lanzavecchia showed that B cells recognising IgGFc could get help from any T cell responding to an ant igen co-endocytosed with IgG by the B cell as part of an immune complex. In coeliac disease it seems likely that B cells recognising tissue transglutamine are helped by T cells recognising gliadin. Aberrant B cell receptor-mediated feedback - A feature of human autoimmune disease is that it is largely restricted to a small group of antigens, several of which have known signaling roles in the immune response (DNA, C1q, IgGFc, Ro, Con. A receptor, Peanut agglutinin receptor(PNAR)). This fact gave rise to the idea that spontaneous autoimmunity may result when the binding of antibody to certain antigens leads to aberrant signals being fed back to parent B cells through membrane bound ligands. These ligands include B cell receptor (for antigen), IgG Fc receptors , CD21, which binds complement C3d, Toll -like receptors 9 and 7 (which can bind DNA and nucleoproteins) and PNAR. More indirect aberrant activation of B cells can also be envisaged with autoantibodies to acetyl choline receptor (on thymic myoid cells) and hormone and hormone binding proteins. Together with the concept of T -cell-B-cell discordance this idea forms the basis of the hypothesis of self perpetuating autoreactive B cells [ 1 4 ] . Autoreactive B cells in spontaneous autoimmunity are seen as surviving because of subversion both of the T cell help pathway and of the feedback signal through B cell receptor, thereby overcoming the negative signals responsible for B cell self -tolerance without necessarily requiring loss of T cell self -tolerance. Molecular Mimicry - An exogenous antigen may share structural similarities with certain host antigens; thus, any antibody produced against this antigen (which mimics the self -antigens) can also, in theory, bind to the host antigens, and amplify the immune response. The idea of molecular mimicry a rose in the context of Rheumatic Fever, which follows infection with Group A beta -haemolytic streptococci. Although rheumatic fever has been attributed to molecular mimicry for half a century no antigen has been formally identified (if anything too many have been proposed). Moreover, the complex tissue distribution of the disease (heart, joint, skin, b asal ganglia) argues against a cardiac specific antigen. It remains entirely possible that the disease is due to e.g. an unusual interaction between immune complexes, complement components and endothelium. Idiotype Cross-Reaction - Idiotypes are antigenic epitopes found in the antigen-binding portion (Fab) of the immunoglobulin molecule. Plotz and Oldstone presented evid ence that autoimmunity can arise as a result of a cross-reaction between the idiotype on an antiviral antibody and a host cell receptor for the virus in question. In this case, the host-cell receptor is envisioned as an internal image of the virus, and the anti-idiotype antibodies can react with the host cells. Cytokine Dysregulation - Cytokines have been recently divided into two groups according to the population of cells whose functio ns they promote: Helper T -cells type 1 or type 2. The second category of cytokines, which include IL -4, IL-10 and TGF-β (to name a few), seem to have a role in prevention of exaggeration of proinflammatory immune responses. Dendritic cell apoptosis - immune system cells called dendritic cells present antigens to active lymphocytes. Dendritic cells that are defective in apoptosis can lead to inappropriate systemic lymphocyte activation and consequent decline in self -tolerance. [ 1 5 ] Epitope spreading or epitope drift - when the immune reaction changes from targeting the primary epitope to also targeting other epitopes. [ 1 6 ] In contrast to molecular mimicry, the other epitopes need not be structurally similar to the primary one. The roles of specialized immunoregulatory cell types, such as regulatory T cells, NKT cells, γδ T-cells in the pathogenesis of autoimmune disease are under investigation. Classification Autoimmune diseases can be broadly divided into systemic and organ specific or localised autoimmune disorders, depending on the principal clinico-pathologic features of each disease. Systemic autoimmune diseases include SLE, Sjögren's syndrome, scleroderma, rheumatoid arthritis, and dermatomyositis. These conditions tend to be associated with autoantibo dies to antigens which are not tissue specific. Thus although polymyositis is more or less tissue specific in presentation, it may be included in this group because the autoantigen s are often ubiquitous t -RNA synthetases. Local syndromes which affect a specific organ or tissue: o Endocrinologic: Diabetes mellitus type 1 , Hashimoto's thyroiditis, Addison's disease o Gastrointestinal: Coeliac disease, Pernicious anaemia o Dermatologic: Pemphigus vulgaris, Vitiligo o Haematologic: Autoimmune haemolytic anaemia , Idiopathic thrombocytopenic purpura o Neurological: Myasthenia gravis Using the traditional “organ specific” and “non -organ specific” classification scheme, many dis eases have been lumped together under the autoimmune disease umbrella. However, many chronic inflammatory human disorders lack the telltale associations of B and T cell driven immunopathology. In the last decade it has been firmly established that tissue "inflammation against self" does not necessarily rely on abnormal T and B cell responses. This has led to the recent proposal that the spectrum of autoimmunity should be viewed along an “immunological disease continuum,” with classical autoimmune diseases a t one extreme and diseases driven by the innate immune system at the other extreme. Within this scheme, the full spectrum of autoimmunity can be included. Many common human autoimmune diseases can be seen to have a substantial innate immune mediated immunopathology using this new scheme. This new classification scheme has implications for understanding disease mechanisms and for therapy development (see PLoS Medicine article. Diagnosis Diagnosis of autoimmune disorders largely rests on accurate history and physical examination of the patient, and high index of suspicion against a backdrop of certain abnormalities in routine laboratory tests (example, elevated C-reactive protein). In several systemic disorders, serological assays which can detect specific autoantibodies can be employed. Localised disorders are best diagnosed by immunofluorescence of biopsy specimens. Autoantibodies are used to diagnose many autoimmune diseases. The levels of autoantibodies are measured to determine the progress of the disease . Treatments Treatments for autoimmune disease have traditionally been immunosuppressive , anti-inflammatory, or palliative. [ 4 ] Nonimmunological therapies, such as hormone replacement in Hashimoto's thyroiditis or Type 1 diabetes mellitus treat outcomes of the autoaggressive response, thus these are palliative treatments. Dietary manipulation limits the severity of celiac disease . Steroidal or NSAID treatment limits inflammatory symptoms of many diseases. IVIG is used for CIDP and GBS. Specific immunomodulatory therapies, such as the TNFα antagonists (e.g. etanercept), the B cell depleting agent rituximab, the anti-IL-6 receptor tocilizumab and the costimulation blocker abatacept have been shown to be useful in treating RA. Some of these immunotherapies may be associated with increased risk of adverse effects, such as susceptibility to infection. Helminthic therapy is an experimental approach that involves inoculation of the patient with specific parasitic intestinal nematodes (helminths). There are currently two closely-related treatments available, inoculation with either Necator americanus, commonly known as hookworms, or Trichuris Suis Ova, commonly known as Pig Whipworm Eggs. [17][17][18][19][20][21] T cell vaccination is also being explored as a possible future therapy for auto-immune disorders. .